Abstract
Objective
To explore the incidence, characteristics, complications and socioeconomic impacts associated with falls in community-dwelling elderly.
Methods
From September 1, 2015 to October 12, 2015, a questionnaire-based survey was conducted involving a total of 2,012 elderly who lived in Guro-gu (Seoul), Yeongdeungpo-gu (Seoul), Yangpyeong-gu (Gyeonggi-do), Dalseong-gu (Daegu), and Jung-gu (Daegu). The subjects were interviewed using a structured questionnaire to obtain demographic characteristics and comprehensive falling histories. The socioeconomic cost related to falls was estimated using the statistical data provided by the Health Insurance Review and Assessment Service.
Results
Falls were recorded in 666 out of the 2,012 subjects (33.1%) during the past year. Frequent falls occurred during December, in the afternoons, when the floor was slippery. The most common injuries included the low back and the most common injury type was sprain. The total direct costs related to falls involving the 2,012 subjects were 303,061,019 KRW (Korean won). The average medical cost related to falls in the 2,012 subjects was 150,627 KRW and the average medical cost of 666 subjects who experienced falls was 455,047 KRW. Estimates of the total population over the age of 60 years showed that the annual direct costs associated with falls in Korea over the age of 60 years were about 1.378 trillion KRW.
Conclusion
This study was conducted to explore the incidence, characteristics, complications, and socioeconomic impacts of falls in community-dwelling elderly. This study is expected to be used as a source of basic data for the establishment of medical policy for the elderly and the development of a fall prevention program for the elderly in Korea.
Go to : 
A fall is a sudden, unintentional change in position that causes a person to move quickly downwards onto or towards the ground. The frequency of falls is increasing with age, and it is known that about a third of the elderly population aged 65 years or older and about half of those aged 80 years or older experience a fall in one year [1].
The elderly are at a greater risk of falling and sustaining injuries than younger individuals, and associated complications are also more severe than in the younger generations [2]. In the elderly, fractures of the hip, waist, wrist, and femur are occasionally caused by falls, and about 80%–90% of hip fractures are known to be triggered by falls [3]. In addition to physical impairment, falls affect emotions, leading to functional limitations and impairment [4].
In the elderly, falls are an important risk factor associated with quality of life and do not affect individuals alone. Korea has entered an aging society with an elderly population exceeding 7.1% of the total population in 2000 and is expected to enter an aging society in 2018. As the elderly population soars, socioeconomic losses including medical costs due to falls will continue to increase. In other words, in an aging society such as Korea, falls in the elderly represent a major challenge at the individual and social levels.
Despite studies involving the elderly falls in Korea, comprehensive studies including complications and socioeconomic impacts related to falls are lacking. In the present study [5], we investigated the current state of falls and the associated socioeconomic cost among the elderly population in rural areas. However, the limitation related to the exclusion of elderly populations in more diverse regions. Thus, this large-scale survey was planned to explore the incidence, characteristics, complications and socioeconomic impacts of falls in community-dwelling elderly.
Go to : 
The questionnaires were used to survey 2,012 elderly people aged over 60 years who visited public health centers. Approximately 400 elderly people were recruited from each of the following districts: Guro-gu (Seoul), Yeongdeungpo-gu (Seoul), Yangpyeong-gu (Gyeonggi-do), Dalseong-gu (Daegu), and Jung-gu (Daegu). The study included individuals from different cities and rural areas.
This study was conducted using a questionnaire. Our previous studies reviewed and compared the existing literature related to falls in the elderly. In addition, we developed our own questionnaire and evaluated the fitness of the questionnaire in a pilot study.
From September 1, 2015 to October 12, 2015, a questionnaire-based survey was conducted involving 2,012 elderly who lived in the five areas mentioned above. The subjects were interviewed using a structured questionnaire to obtain demographic characteristics and detailed falling histories including falling rates over lifetime and during the past year, time and place of fall, causes, fall-related injuries and complications, medical treatment and expenditure related to falls, and so on. In addition, the socioeconomic medical costs related to falls were estimated using the statistics provided by the Health Insurance Review and Assessment Service (HIRA).
To estimate the socioeconomic costs related to falls, we obtained data based on the above survey: injury area, injury type, need for hospitalization, duration of hospitalization, need for outpatient treatment, and frequency of outpatient visits related to falls. The fall injuries were converted into the International Classification of Diseases 10th revision (ICD-10) codes by combining the area and type of injury on the questionnaire. For example, if the injury site was femur and the injury type was fracture, it was converted to S72 code (fracture of femur) on the ICD-10 code.
In order to calculate the insured portion of the healthcare cost related to falls, we used the data of medical costs based on the ICD-10 codes of HIRA in 2014. Using the HIRA data, we obtained medical expense data for each ICD-10 code in Korea during 2014. However, since the ICD-10 code in the HIRA data does not exclusively include fall-related injuries, it was necessary to match the HIRA data with fall-related data on the questionnaire. The insured portions of the healthcare cost for subjects who were admitted to hospital or visited outpatient or oriental clinic were calculated as follows: (number of days of hospitalization or outpatient visits on the questionnaire) × (data of medical expenses per day from the HIRA).
For example, in the S72 code (fracture of femur), the total number of days spent in the outpatient clinics for femoral fractures among females was 42 days, and the outpatient medical expenses per day for the S72 code in the HIRA data was 38,021 KRW (Korean won). Therefore, the total cost incurred by women among the 2,012 subjects who used outpatient clinics for fall-related femoral fracture was 1,596,882 KRW. Thus, we estimated the medical expenditure of all the subjects based on ICD-10 code, gender, hospital admission or outpatient visit.
The healthcare cost of the uninsured portion was calculated based on the ‘Survey on the Benefit Coverage Rate of National Health Insurance in 2014’ of the National Health Insurance Service (NHIS).
The general characteristics of the subjects were analyzed using descriptive statistics. Based on the data from the questionnaire and HIRA, we estimated the socioeconomic costs related to falls. The statistical analysis was performed using SPSS software ver. 21.0 (IBM, Armonk, NY, USA).
Go to : 
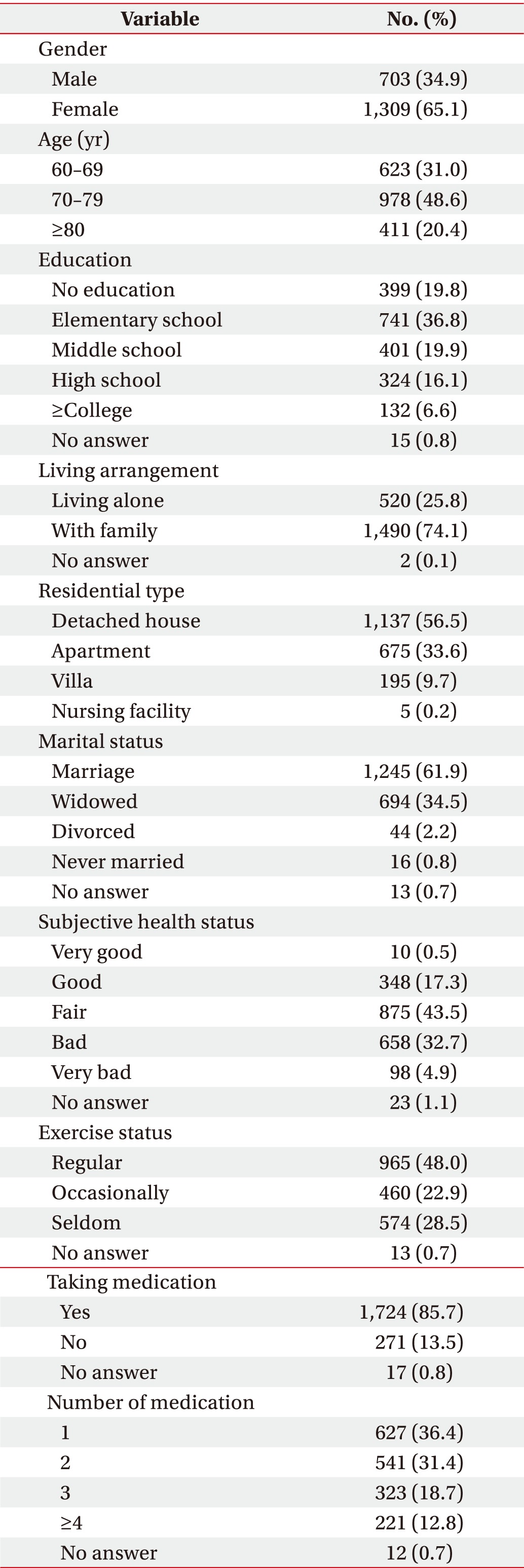
Women constituted 65.1% of the 2,012 subjects participating in the survey. In the age category, 48.6% ranged between 70 and 80 years. The number of individuals with elementary school graduation was the maximum, and those living with their family accounted for 74.1%. Individuals living in a detached house accounted for 56.5% of the residential type and the number of married participants accounted for 61.9%. A total of 43.5% reported normal in the perception of health status, and 48.0% performed regular exercise. Individual on medication constituted 85.7%, with more than half of them treated with one or two drugs (Table 1).
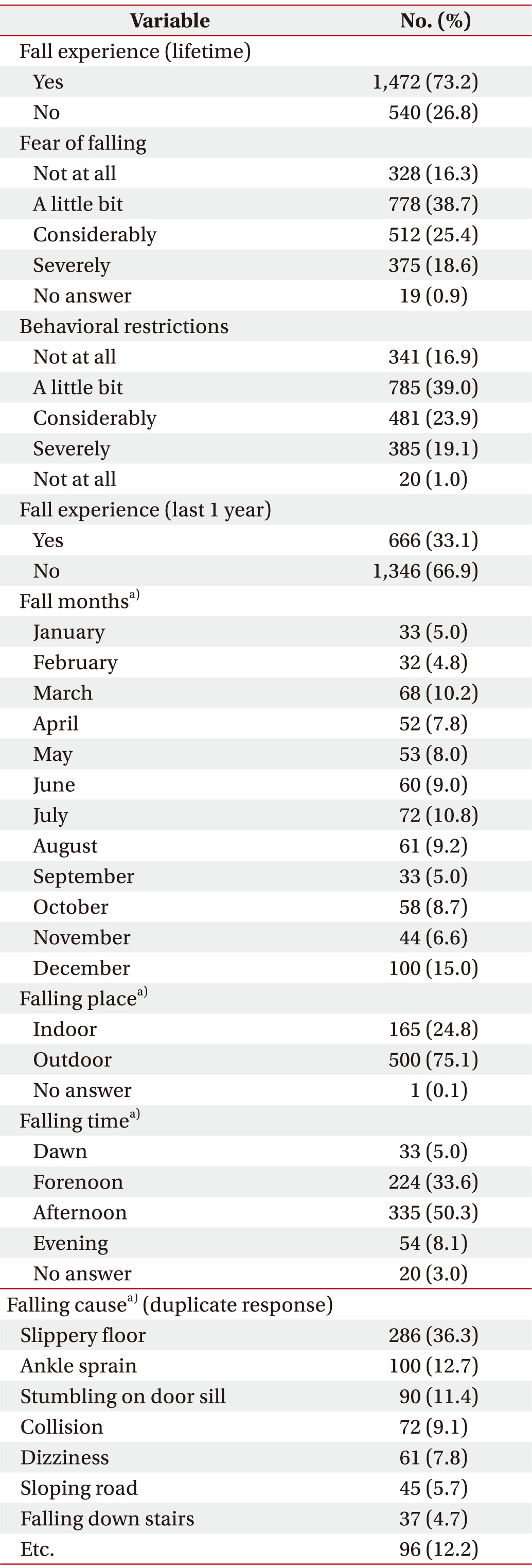
Of the total 2,012 subjects, 1,472 (73.2%) experienced falls in their lifetime and 666 (33.1%) experienced falls in the past year (from September 1, 2014 to August 31, 2015). The falls were most common in December of the past year and occurred mostly in the afternoon. The results of overlapping responses to the reasons included: slippery floor (36.3%), followed by ankle sprain, stumbling on door sill, and collision. When asked about the fear of falling and associated behavioral restrictions most of the participants responded: ‘a little bit’ (Table 2).
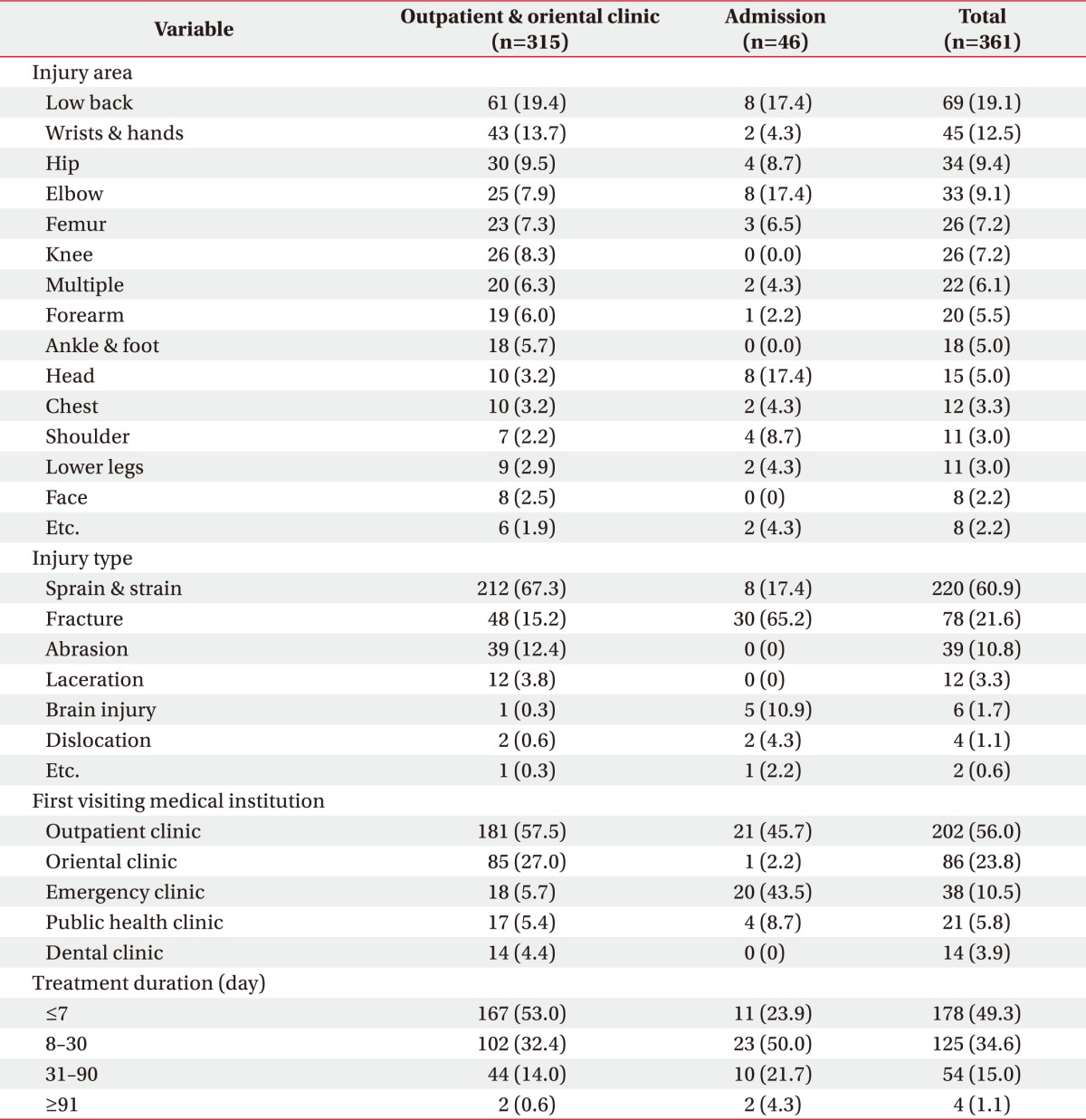
Among the 666 subjects who sustained falls in the past one year, 566 (85.0%) reported an injury due to fall, and 100 (15.0%) reported absence of injury. Among the 566 injuries, 323 (57.1%) underwent medical treatment, and 46 cases of admissions and 315 cases of outpatient and oriental clinic visits were reported. In terms of injury area, the low back was the most common (19.1%), followed by wrist, hip and elbow. Based on injury type, sprains and strains were the most frequent (67.3%) among the outpatients and admissions due to fracture were the highest at 65.2%. Among those visiting medical institutions first, patients mostly visited outpatient clinics (56.0%) and oriental clinics (23.8%). In terms of treatment duration, ‘less than a week’ was the highest response (53.0%) among the outpatients, and ‘more than 1 week to less than 1 month’ was the highest (50.0%) among hospital admissions (Table 3).
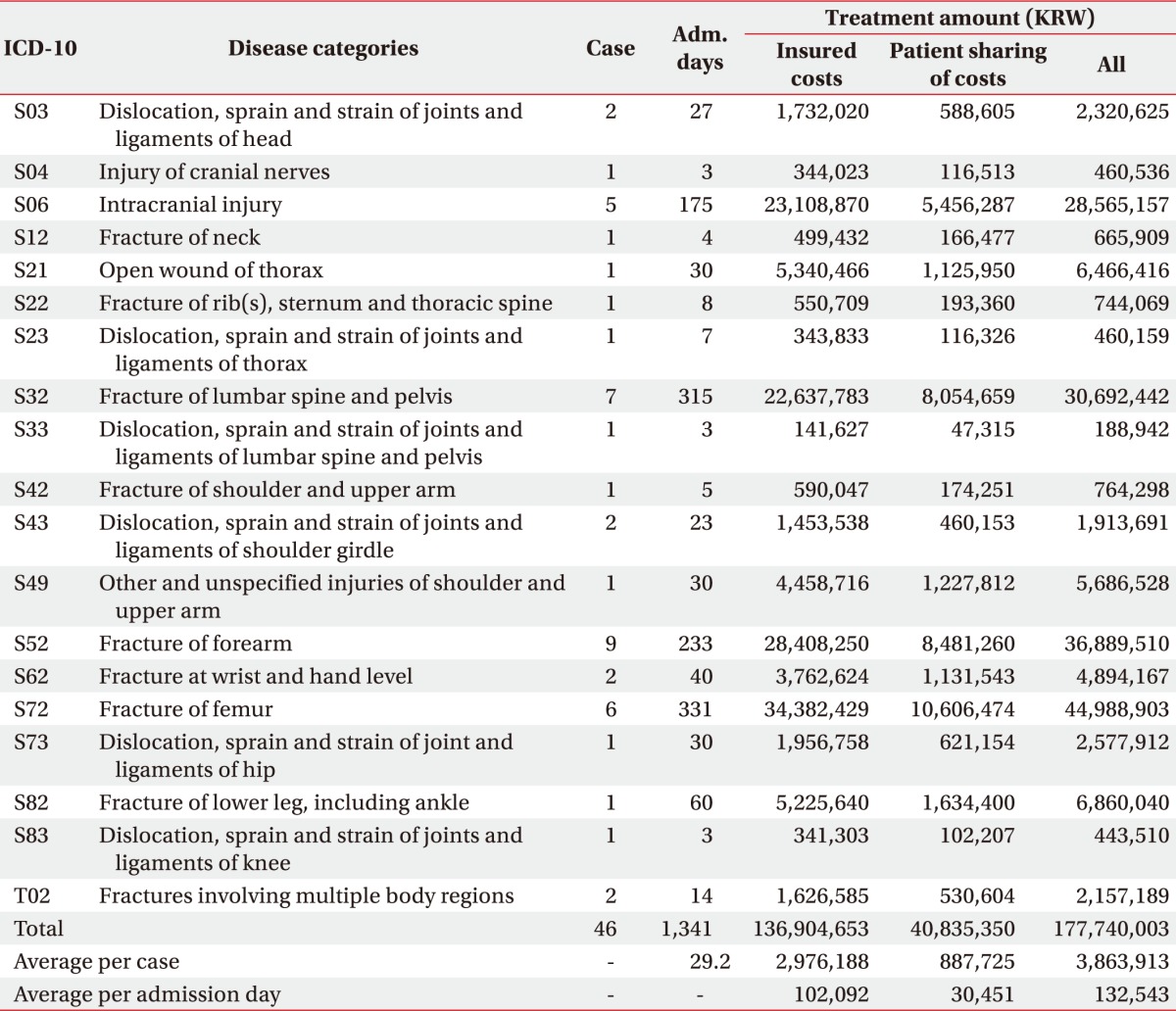
A total of 46 cases were hospitalized due to injuries associated with a fall in the past year. As shown in Table 4, the total cost of medical benefits of inpatients was 177,740,003 KRW, including insured costs amounting to 136,904,653 KRW and patient cost-sharing of 40,835,350 KRW. The average hospitalization cost per admission was 3,863,913 KRW, and the average patient cost-sharing per admission was 887,725 KRW. The average hospitalization cost per hospital day was 132,543 KRW and the average daily patient cost-sharing per hospital day was 30,451 KRW. The total number of hospitalization days was 1,341 days, and the average length of hospitalization per case was 29 days. In case of hospitalization, ICD-10 codes associated with the highest treatment cost were S72 (fracture of femur), followed by S52 (fracture of forearm), S32 (fracture of lumbar spine and pelvis), S06 (intracranial injury). The total hospitalization cost involving the first four codes was 141,136,011 KRW, which accounted for 79.4% of total inpatient cost.
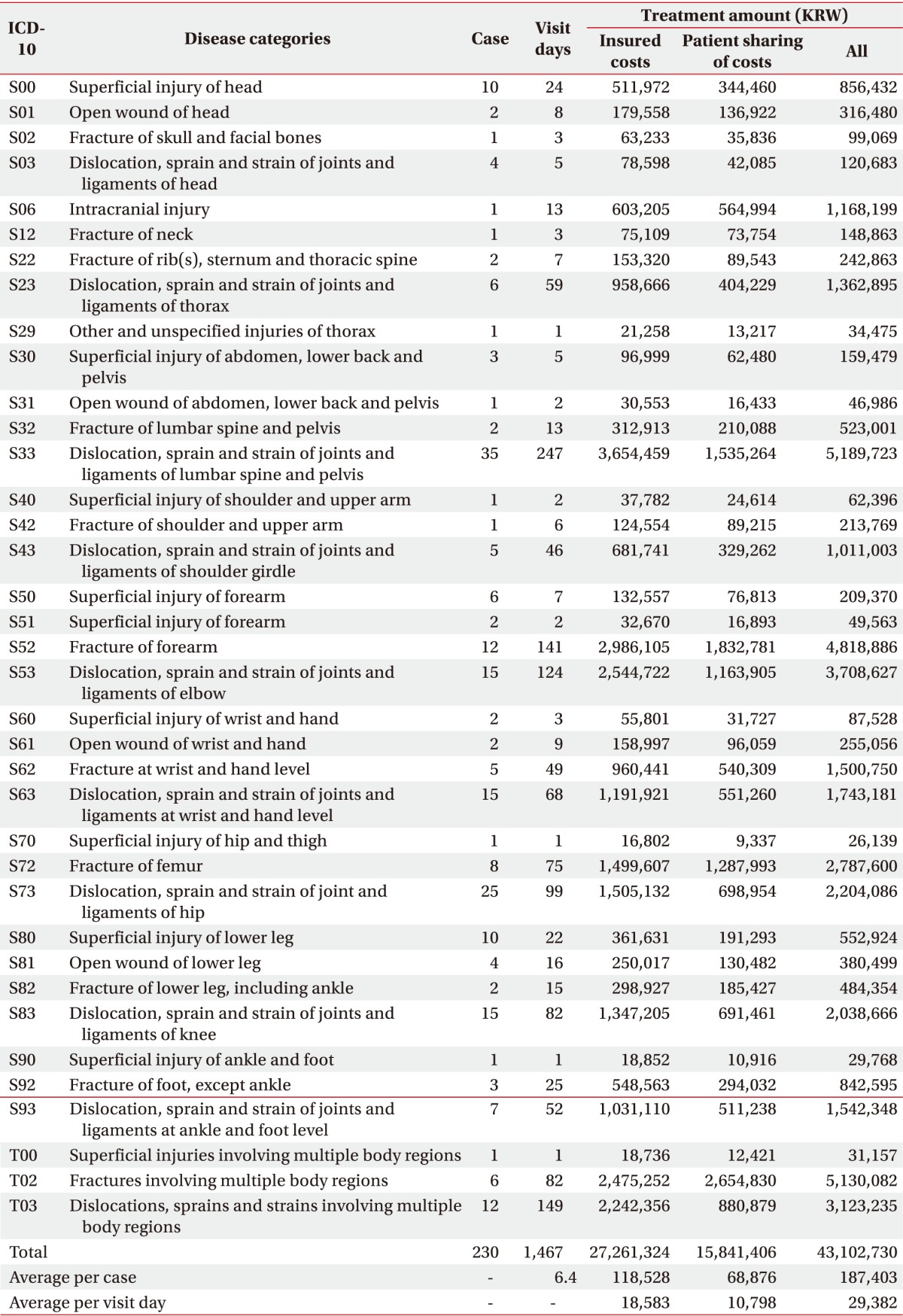
There were 230 cases undergoing outpatient treatment for fall-related injuries in the past year. As shown in Table 5, the total cost of medical benefits incurred by outpatients was 43,102,730 KRW, including insurance of 27,261,324 KRW and patient cost-sharing of 15,841,406 KRW. The average outpatient cost was 187,403 KRW and the average patient cost-sharing was 68,876 KRW. The average daily outpatient fee was 29,382 KRW and the average patient cost-sharing was 10,789 KRW. The total number of outpatient visits was 1,467 days, which involved 6.4 visits per case. Among outpatients, the highest cost of medical treatment according to ICD-10 code type was S33 (dislocation, sprain and strain of joints and ligaments of lumbar spine and pelvis), followed by T02 (fractures involving multiple body regions), S52 (fracture of forearm), S53 (dislocation, sprain and strain of joints and ligaments of elbow), T03 (dislocations, sprains and strains involving multiple body regions). The total hospitalization cost involving the first to fifth codes was 38,776,916 KRW, which accounted for 90.0% of total inpatient cost.
The number of patients who visited outpatient clinics due to falls during the past year was 85, the total number of visits was 347, and the number of oriental treatments per case was 4.1. The calculated oriental treatment costs were 8,355,066 KRW based on the daily oriental clinic expenses of 24,078 KRW indicated in the ‘Statistical Index of Medical Expenses in 2014’ of the Health Insurance Review and Assessment Service.
In case of hospitalization, the cost of prescription drugs is included in the admission fee, and therefore, we did not calculate the inpatient drug fee separately. The total number of outpatients cases associated with falls in the past year was 230, and the total number of outpatient visits was 1,467. However, among individuals sustaining falls during the past year, 152 visited only pharmacies directly, without consulting any professionals at medical institutions. The medication costs were calculated at 11,158,148 KRW based on the daily medication expenses of 6,892 KRW indicated in the ‘Statistical Index of Medical Expenses in 2014’ of the Health Insurance Review and Assessment Service.
Of the 666 cases of fall reported during the past year, 60 utilized medical assistive equipment including 21 canes, 15 abdominal braces, 11 walkers, 8 joint supports, and 5 other devices. The purchase cost of these assistive devices according to the survey results amounted to a total of 2,755,000 KRW.
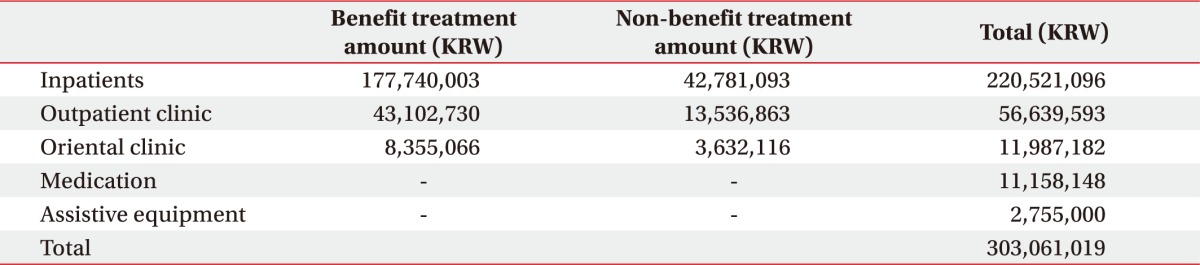
The health care cost of the uninsured portion was calculated according to the ‘Survey on the Benefit Coverage Rate of National Health Insurance in 2014’ of NHIS. The uninsured portion of total medical expenses was 19.4% for hospitalization, 23.9% for outpatient clinic, and 30.3% for oriental medical clinic. Accordingly, the non-benefit costs were 42,781,093 KRW for hospital admissions, 13,536,863 KRW for outpatient treatments, and 3,632,116 KRW for oriental treatments. The direct costs related to falls are calculated by adding the benefit and non-benefit costs. The total cost included 220,521,096 KRW involving hospital admission, 56,639,593 KRW covering outpatient treatment, 11,987,182 KRW for oriental treatment, 11,158,148 KRW for medications, and 2,755,000 KRW for medical assistive equipment, and the total direct costs related to falls sustained by 2,012 subjects were 303,061,019 KRW (Table 6). The average medical cost related to falls in the 2,012 subjects was 150,627 KRW and the average medical costs of 666 subjects who experienced falls during the last year were 455,047 KRW.
The total direct cost related to falls of 2,012 subjects was 303,061,019 KRW. According to the resident registration demographics available on the website of the Ministry of the Interior, as of December 2014, there are 9,147,370 people in Korea over 60 years of age. Estimates of the total population over the age of 60 years showed that annual direct medical costs associated with falls in Korea over the age of 60 years are about 1.378 trillion KRW.
Go to : 
In this study, 73.2% of the subjects experienced falls during their lifetime, and 33.1% of the falls occurred during the last year. These data are close to the annual 30.0% fall rate reported in a Western study [3]. The most frequent month for falls was December, was and they occurred outdoors, mostly in the afternoons. The most frequently reported cause was slippery floor, suggesting that a majority of falls occurred on roads with slippery ice during the winter and in the afternoon with a lot of activity. Increased awareness of the patterns of injury is needed to prevent falls.
Among the subjects, 666 experienced the incidents during the past year, and 566 of the subjects sustained injury as a result and 323 of them visit medical institutions for consultation or treatment. In other words, 16.1% of the total of 2,012 subjects visited medical institutions for fall-related injuries and 57.1% of the 566 people who fell used medical facilities.
Fall-related injuries treated medically involved: low back 19.1%, wrists and hands 12.5%, hip 9.4%, and elbow 9.1%. The findings suggest that the most impact is applied to the back when a fall occurs. The high rate of damage to wrists and hands is related to the action of putting the hand on the floor during the fall. The types of injury were sprain 60.9% and fracture 21.6%.
In this study, the socioeconomic costs associated with falls were estimated. The average medical costs of 666 subjects who experienced falls during the last year were 455,047 KRW. Therefore, if an elderly person sustains a fall, the average annual expense involved is 500,000 KRW, which is a significant economic burden for the elderly. The total direct cost for the 2,012 subjects was 303,061,019 KRW, amounting to a total of 1.378 trillion KRW in those aged 60 years or more. Therefore, falls in the elderly represent a great individual and socioeconomic burden.
The study limitation relates to the questionnaire-based format, and the results depend on the memories of the participants, suggesting a possible recall bias. In addition, since the survey involved the elderly who visited a public health center, the sample was not randomly selected. In addition, the medical expenses may be underestimated because it is impossible to include deaths due to falls and resulting complications. There may also be limitations in the methodology estimating the socioeconomic costs due to falls.
However, this large-scale study involved samples from the urban and rural areas to estimate the direct medical expenses due to falls in the elderly based on a questionnaire survey. A more accurate estimation may require additional items indicated in the national questionnaires such as the Community Health Survey.
The significance of this study relates to the development of an independent questionnaire to obtain objective and quantitative data related to geriatric falls. The study findings are expected to guide the development of medical policies and fall prevention programs for the elderly in Korea.
Go to : 
ACKNOWLEDGMENTS
This research was supported by the R&D grant (No. 2015005) on rehabilitation by Korea National Rehabilitation Center Research Institute, Ministry of Health & Welfare.
Go to : 
References
1. Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997; 337:1279–1284. PMID: 9345078.

2. Reyes-Ortiz CA, Al Snih S, Markides KS. Falls among elderly persons in Latin America and the Caribbean and among elderly Mexican-Americans. Rev Panam Salud Publica. 2005; 17:362–369. PMID: 16053646.

3. Grisso JA, Kelsey JL, Strom BL, Chiu GY, Maislin G, O'Brien LA, et al. Risk factors for falls as a cause of hip fracture in women. The Northeast Hip Fracture Study Group. N Engl J Med. 1991; 324:1326–1331. PMID: 2017229.
4. Franzoni S, Rozzini R, Boffelli S, Frisoni GB, Trabucchi M. Fear of falling in nursing home patients. Gerontology. 1994; 40:38–44. PMID: 8034202.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download