Abstract
Objective
To investigate the differences in biomechanical parameters measured by gait analysis systems between healthy subjects and subjects with plantar fasciitis (PF), and to compare biomechanical parameters between ‘normal, barefooted’ gait and arch building gait in the participants.
Methods
The researchers evaluated 15 subjects (30 feet) with bilateral foot pain and 15 subjects (15 feet) with unilateral foot pain who had a clinical diagnosis of PF. Additionally, 17 subjects (34 feet) who had no heel pain were recruited. Subjects were excluded if they had a traumatic event, prior surgery or fractures of the lower limbs, a leg length discrepancy of 1 cm or greater, a body mass index greater than 35 kg/m2, or had musculoskeletal disorders. The participants were asked to walk with an arch building gait on a treadmill at 2.3 km/hr for 5 minutes. Various gait parameters were measured.
Results
With the arch building gait, the PF group proved that gait line length and single support line were significantly decreased, and lateral symmetry of the PF group was increased compared to that of the control group. The subjects with bilateral PF displayed significantly increased maximum pressure over the heel and the forefoot during arch building gait. In addition, the subjects with unilateral PF showed significantly increased maximum pressure over the forefoot with arch building gait.
Plantar fasciitis (PF) is the most common cause of heel pain, yet its etiology is not well understood [12]. Recently, several studies proposed that PF is inflammation of the plantar fascia [3]. It is characterized by pain and stiffness in the heel, the medial arch of the foot, and can affect daily activities [34].
The symptoms vary in intensity and the foot pain usually occurs on the first step in the morning [5]. Sometimes the pain may improve after a few steps or within a few hours, but it often increases as the day progresses [1]. Typically, the prognosis of PF is quite good [1]. In more than 80% of patients, foot pain will disappear within a year [3].
The diagnosis of PF is clinical and based on a history of foot pain and pain upon palpation of the fascia [6]. Diagnostic imaging may be used to exclude other causes of pain. Radiographic examinations may help to identify heel spurs (found in 27% of cases), and ultrasound examinations of symptomatic patients may reveal thickened fascia and inflammation [78].
Conservative treatments, such as stretching of the plantar fascia or Achilles tendon, icing, heating, applying electrical modalities, using anti-inflammatory medications, applying extra-corporeal shock wave therapy, and using foot orthoses (e.g., an insole) are successful in improving function and reducing pain [91011121314]. Recently, some researchers proposed another solution for patients with foot pain. This short-foot exercise is done by pulling the first metatarsal head toward the heel without toe flexion and maintaining this position for 10 minutes to increase the medial longitudinal arch [15]. The exercise improves the intrinsic muscles of the plantar foot by intensifying and optimizing the sole's contact with the floor [15]. Therefore, the small-foot exercise, which is same meaning of the arch building gait, increases dynamic stability. Additionally, the exercise may improve the sense of balance and mitigate pain severity. There have been insufficient studies focused on objective measures of patients who have bilateral or unilateral PF. In addition, most PF studies are conducted while in a static status.
The aim of this study is to investigate the differences in biomechanical parameters measured by gait analysis systems, comparing healthy subjects with those who have PF. Using a dynamic analysis, the research assesses the patterns of subjects with PF, while barefoot and with an arch building gait.
Thirty subjects, who were either hospitalized or outpatients at the Kyung Hee University Hospital at Gangdong between March 1, 2015 and June 30, 2016, were selected for this study. The researchers studied 15 subjects (30 feet) with bilateral foot pain and 15 subjects (15 feet) with unilateral foot pain who had a clinical diagnosis of PF for more than four months. Additionally, 17 normal subjects (34 feet) who had no heel pain were recruited. Subjects were excluded if they had any of the following conditions: (1) a traumatic event; (2) a prior surgery of the lower limbs; (3) fractures of the lower limbs; (4) a leg length discrepancy of 1 cm or greater; (5) a body mass index greater than 35 kg/m2; (6) musculoskeletal disorders such as neuropathy, patellofemoral syndrome, rheumatoid arthritis, calcaneal spurs; and (7) any disorder of the central or peripheral nervous system.
The Zebris gait analysis system was used to obtain numerical data for kinetic and kinematic gait parameters (Zebris Medical GmbH, Isny im Allgau, Germany). The Zebris instrumented gait analysis system (FDM-T; Zebris Medical GmbH) comprises a capacitance-based, foot pressure platform housed within a treadmill. The pressure platform has a sensing area of 150×50 cm and the sensor unit has 5,370 pressure/force sensors. The foot is mapped at high resolution to facilitate the detection of even the subtlest changes in force distribution, including center of pressure (COP) trajectories during static stance and gait.
Participants were asked to walk barefoot on a treadmill with a relaxed posture at 2.3 km/hr for 5 minutes. Participants were educated about the short foot exercise before employing the arch building motion. The researchers requested that they walk while raising the arch of their feet by pulling the big toe toward the heel, which makes the foot ‘shorter’, for about 10 minutes (Fig. 1). They practiced this arch building gait and then walked with an arch building gait on the treadmill at 2.3 km/hr for 5 minutes. They flexed the metatarsophalangeal and proximal interphalangeal joints during gait, while minimizing distal interphalangeal flexion.
Major gait parameters included the following values.
Geometry—foot rotation (°): rotation toward (−) and away from (+) the angle between the longitudinal axis of the foot and the direction of gait; step length (cm): the distance from the heel contact of one foot to that of the other foot); phase: stance phase (%), swing phase (%), load response (%), mid-stance (cm), pre-swing (cm).
Time—step time (s): the time from heel contact of one foot to that of the other foot).
COP—gait line length (mm): the length of the movement of the COP during the entire stance phase; single support line (mm): the length of the movement of the COP during single-leg support; anterior/posterior position (mm): the distance from the line connecting the heels of both feet to the mean point where the COP line intersects; lateral symmetry (°): the horizontal distance from the center point of the horizontal line connecting the COP lines of both feet to the intersecting center point, (Fig. 2).
Maximum force—forefoot (N), midfoot (N), and heel (N): the mean value of the maximum force measured across the forefoot, midfoot, and heel.
Maximum pressure—forefoot (N/cm2), midfoot (N/cm2), and heel (N/cm2): the mean value of maximum pressure measured across the forefoot, midfoot, and heel).
Furthermore, force and pressure parameters were calculated for each gait trial. These parameters were calculated using the absolute value of the differences between corresponding right and left values.
To compare the subjects' group (bilateral or unilateral PF) with the control group, the researchers used the one-way ANOVA (paired t-test) technique for quantitative variables with normal distribution and the Wilcoxon signed-rank test for quantitative variables without normal distribution. To compare the barefooted gait with arch building gait in subjects with bilateral and unilateral PF, the researchers used the Student t-test for quantitative variables with normal distribution and the Mann-Whitney U-test for quantitative variables without normal distribution. The statistical analyses were conducted using the SPSS program ver. 17.0 (SPSS Inc., Chicago, IL, USA). Statistical significance for these analyses was established at 5% (p<0.05).
Thirty patients, who were either hospitalized or outpatients at the Kyung Hee University Hospital at Gangdong between March 1, 2015 and June 30, 2016, were selected for this study. Fifteen subjects (30 feet) with bilateral foot pain (Group B), 15 subjects (15 feet) with unilateral foot pain (Group C) and 17 subjects (34 feet) without foot pain (Group C) were included as the study groups and the control group, respectively. The characteristics of both groups are summarized in Table 1.
The PF group demonstrated that step length (bilateral, 41.13±6.17 cm; unilateral, 41.40±7.20 cm) and step time (bilateral, 0.34±0.79 seconds; unilateral, 0.46±0.83 seconds) were significantly decreased (p<0.001) during barefooted gait (Table 2).
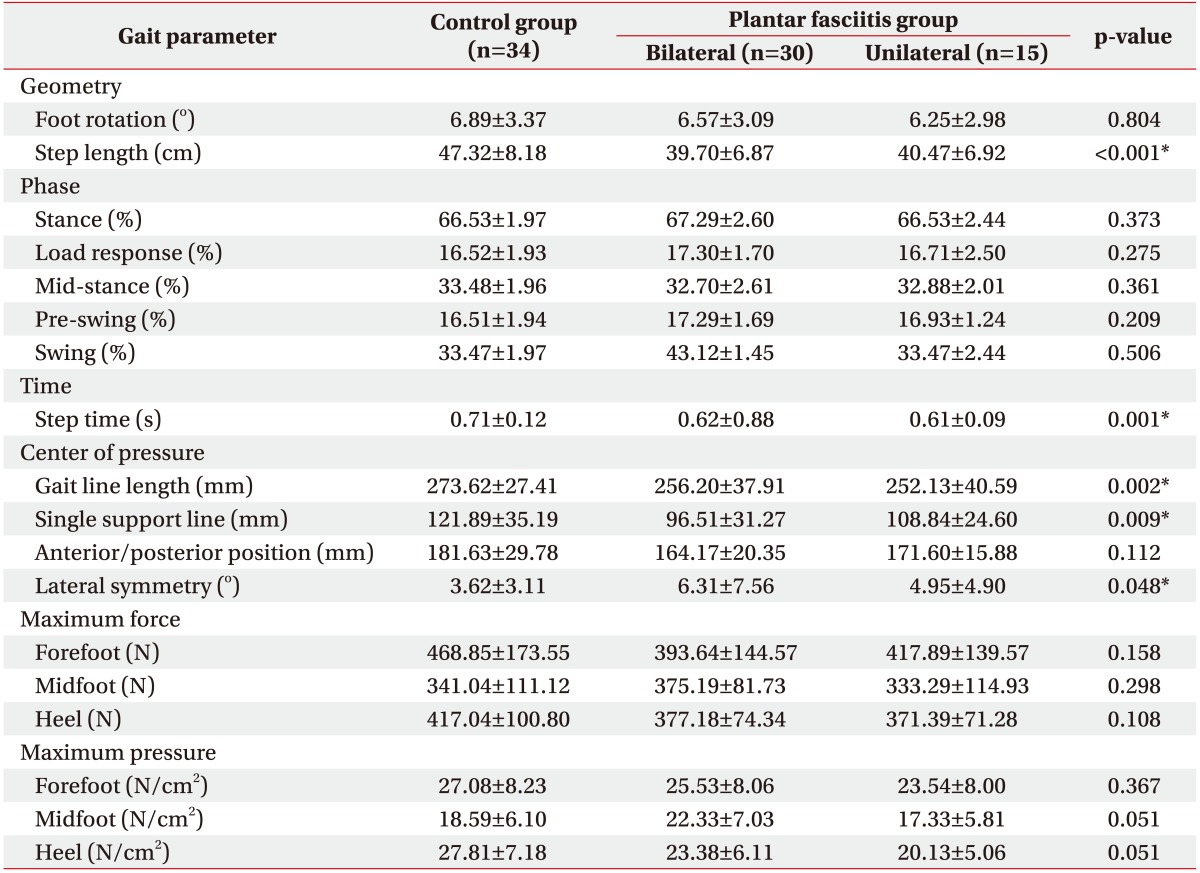
Similarly, the PF group demonstrated that step length (bilateral, 39.70±6.87 cm; unilateral, 40.47±6.92 cm) and step time (bilateral, 0.62±0.88 seconds; unilateral, 0.61±0.09 seconds) were significantly decreased (p<0.001) during arch building gait (Table 3).
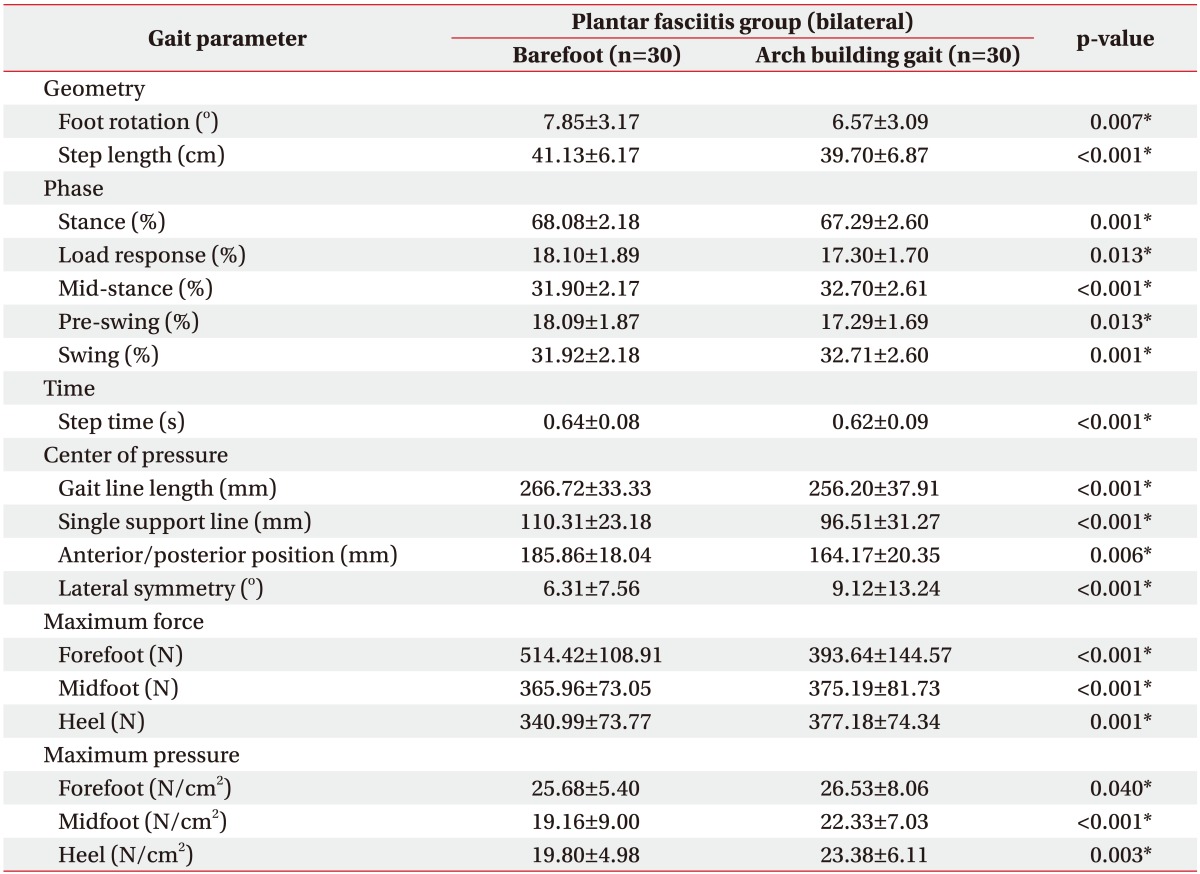
In the group of subjects with bilateral PF, foot rotation (6.57°±3.09°), step length (39.70±6.87 cm), and step time (0.62±0.09 seconds) were significantly decreased (p<0.001) during arch building gait (Table 4).
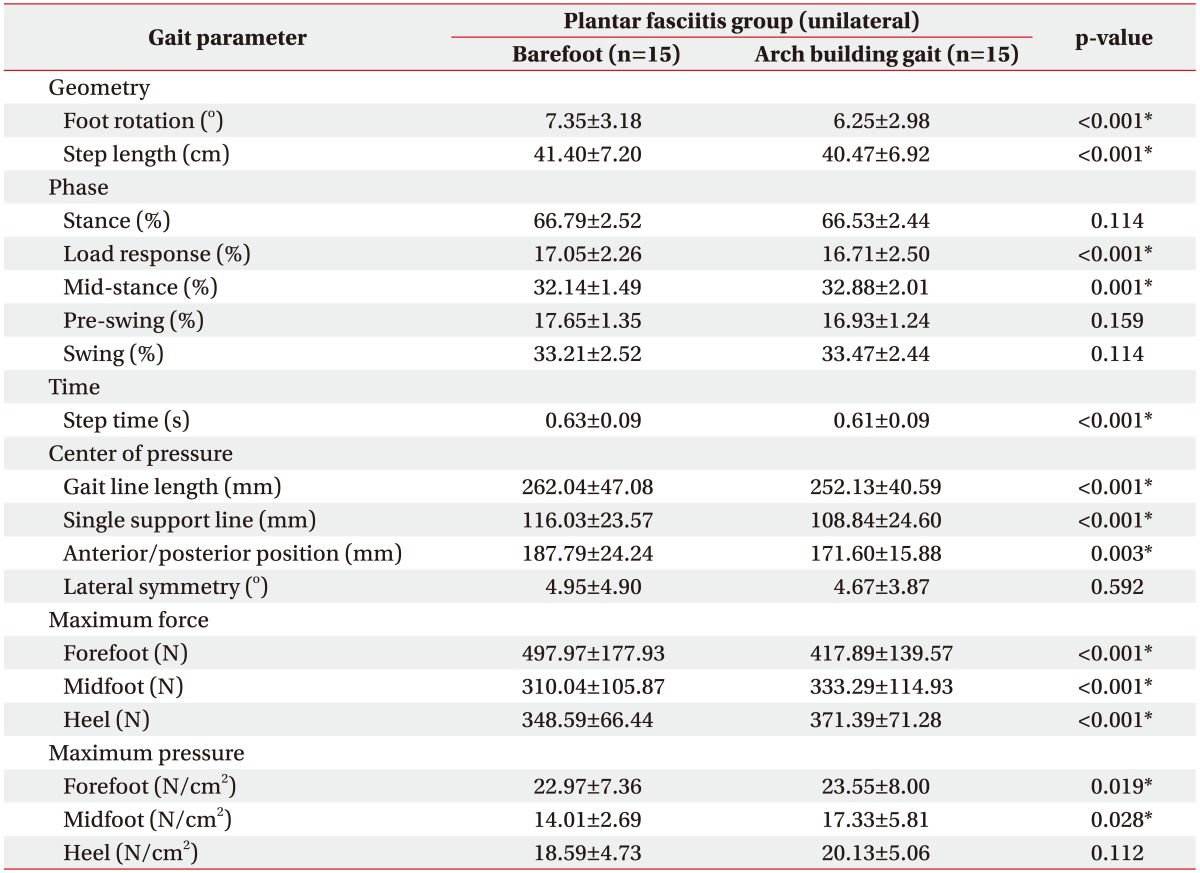
In the group of subjects with unilateral PF, foot rotation (6.25°±2.98°), step length (40.47±6.92 cm), and step time (0.61±0.09 seconds) were significantly decreased (p<0.001) during arch building gait (Table 5).
The PF group demonstrated that gait line length (bilateral, 266.72±33.33 mm; unilateral, 262.04±47.08 mm) and single support line (bilateral, 110.31±23.18 mm; unilateral, 116.03±23.57 mm) were significantly decreased (p<0.001) during barefooted gait (Table 2).
During arch building gait (Table 3), the PF group proved that gait line length (bilateral, 256.20±37.91 mm; unilateral, 252.13±40.59 mm) and single support line (bilateral, 96.51±31.27 mm; unilateral, 108.84±24.60 mm) were significantly decreased (p=0.002, p=0.009). In addition, lateral symmetry (bilateral, 6.31°±7.56°; unilateral, 4.95°±4.90°) of the PF group was increased (p=0.048), compared to that of the control group (3.62°±3.11°).
In the group of subjects with bilateral PF (Table 4), gait line length (256.20±37.91 mm; p<0.001), single support line (96.51±31.27 mm; p<0.001), and anterior/posterior position (164.17±20.35 mm; p=0.006) were significantly decreased during arch building gait. Furthermore, lateral symmetry (9.12°±13.24°; p<0.001) was significantly increased (p<0.001) during arch building gait, compared to that of barefooted gait.
In the group of subjects with unilateral PF (Table 5), gait line length (252.13±40.59 mm, p<0.001), single support line (108.84±24.60 mm; p<0.001), and anterior/posterior position (171.60±15.88 mm; p=0.003) were significantly decreased during arch building gait, compared to that of barefooted gait.
The PF group demonstrated that maximum force over the heel (bilateral, 340.99±73.77 N; unilateral, 348.59±66.44 N) and maximum pressure over the heel (bilateral, 19.80±4.98 N/cm2; unilateral, 18.59±4.73 N/cm2) were significantly less (p<0.001, p=0.048) than the values of the control group. Besides maximum force over the midfoot (365.96±73.05 N), the maximum pressure over the midfoot (19.16±9.00 N/cm2) in subjects with bilateral PF was also significantly increased (p=0.009, p=0.020), compared to that of the control group (Table 2).
In the group of subjects with bilateral PF (Table 4), maximum force over the midfoot (375.19±81.73 N) and over the heel (377.18±74.34 N) was significantly increased (p<0.001) during arch building gait, compared to that of barefooted gait. In addition, maximum pressure over the forefoot (26.53±8.06 N/cm2), over the midfoot (22.33±7.03 N/cm2), and over the heel (23.38±6.11 N/cm2) was significantly increased (p=0.040, p<0.001, and p=0.003) during arch building gait (Fig. 3), compared to that of barefooted gait (Fig. 4).
In the group of subjects with unilateral PF (Table 5), maximum force over the midfoot (333.29±114.93 N) and over the heel (371.39±71.28 N) was significantly increased (p<0.001) during arch building gait, compared to that of barefooted gait. In addition, maximum pressure over the forefoot (23.55±8.00 N/cm2) and over the midfoot (17.33±5.81 N/cm2) was significantly increased (p=0.019, p=0.028) during arch building gait, compared to that of barefooted gait.
Several studies focusing on PF have shown its association with the medial longitudinal arch, that is, the externally applied force and pressure on the vertical structure of the foot during walking [16]. In fact, there is a consensus that PF is associated with the degree of pain and disease prognosis. In addition, recent studies have also shown interest in the biomechanics of rearfoot alignment [17], which has led to the conclusion that biomechanics should be considered as a risk factor for PF. However, the foot is one of the most complex and intricate body parts. As such, it is difficult to fully understand the causes and prognosis of pain in patients with PF based on only a few parameters.
Accordingly, this study assessed the COP, maximum force and the maximum pressure exerted on the forefoot, midfoot, and heel. This analysis was done to identify not only the biomechanics (e.g., geometry, phase, and time) of the healthy subjects and the subjects with PF, but also to evaluate horizontal distribution in the feet.
Daly et al. [18] reported that only 14% of the pressure was applied to the real foot site in patients with PF. As shown in Table 2, the maximum force and maximum pressure applied to the heel area were less in the subjects with unilateral and bilateral PF, compared to that of the normal group during barefooted gait. The researchers can consider the pain in the heel area to be induced by inflammation of the plantar fascia attached to the heel. Thus, the heel area could not be supported properly, unlike that experienced in the gait of healthy people. In the midfoot area, the subjects with bilateral PF showed significant increases in maximum force and maximum pressure, which may be attributed to the force and pressure being distributed to the midfoot area. The subjects with unilateral PF showed decreases in maximum force and maximum pressure applied to the midfoot, which may be due to the center of gravity being applied more to the pain-free, normal foot during gait.
In subjects with bilateral PF, the comparison between walking on flat ground and applying the arch building gait showed decreased gait line length, single support line, and antero-posterior position, along with increased lateral symmetry (Table 4). This is because during arch building gait, the full length of the foot is reduced as intrinsic muscles are contracted to build the arch. Moreover, considering that the lateral symmetry increased and the intersection point of central pressure moved significantly in the posterior direction, the researchers determined that the center point was redistributed to the outer side. With respect to force and pressure observed in the subjects with bilateral PF, increases in the maximum force and maximum pressure applied to the heel area were found. The maximum pressure applied to the forefoot area also increased. Based on these findings, we can deduce that the entire center of gravity moved to the back of the foot and the redistribution of pressure occurred during arch building gait.
As shown in Table 5, similar results were found between the subjects with unilateral PF and those with bilateral PF. The results showed a decrease in the COP parameters, an increase in the maximum force applied on the heel area, an increase in the maximum force and maximum pressure on the midfoot area, and an increase in the maximum pressure on the forefoot area. Despite the decrease in the maximum force on the forefoot, the maximum pressure increased in this location, which may be attributed to the reduced contact area.
As such, when a patient with bilateral or unilateral PF performs the arch building gait, the maximum pressure applied to the foot is redistributed, thereby showing biomechanics similar to that of the healthy group. Conventional rehabilitation exercises applied in patients with PF typically include massaging the soles and stretching of the plantar fascia, Achilles tendon, and hamstrings. This means that gait designed for greater arch building, such as that associated with the short foot exercise, may be helpful to patients.
Another significance of this study is that the biomechanics of the subjects with PF were not identified in a static state, but rather in a dynamic state using a gait analysis system. As normal and arch building gaits were compared and analyzed on a treadmill, data that appeared during normal gait was collected, while objective data were acquired by converting the various parameters into computer graphics and numeric values. In other words, we closely investigated actual gait patterns exhibited during moving status in real time.
The limitations of the present study were as follows: first, the number of participants (particularly those in the unilateral PF group) was small. Second, the effects of the arch building gait were not quantified as pain scores. Third, an additional study is needed on the long-term effects of implementing the arch building gait by comparing the results from before and after the application of the arch building gait. Finally, the gait speed of the participants was 2.3 km/hr, which was slower than that of the subjects with normal gait. Therefore, further studies are needed reflecting speed like that of normal gait activity.
In conclusion, this study involved conducting a twofold comparative analysis. It explored not only the biomechanic differences between normal subjects and subjects with PF, but also the differences between subjects applying normal versus arch building gait with respect to COP length and the position of the intersecting point of the COP. Thus, we confirmed that during arch building gait, biomechanical changes occurred causing the center of gravity to move toward the back of the foot, and the contact area and maximum pressure on the foot to be redistributed. Applying these findings to rehabilitation exercises and the development of proper orthoses may improve the treatment and prognosis of PF.
References
1. Goff JD, Crawford R. Diagnosis and treatment of plantar fasciitis. Am Fam Physician. 2011; 84:676–682. PMID: 21916393.
2. Karabay N, Toros T, Hurel C. Ultrasonographic evaluation in plantar fasciitis. J Foot Ankle Surg. 2007; 46:442–446. PMID: 17980840.

3. Oliveira HA, Jones A, Moreira E, Jennings F, Natour J. Effectiveness of total contact insoles in patients with plantar fasciitis. J Rheumatol. 2015; 42:870–878. PMID: 25774062.

4. Irving DB, Cook JL, Young MA, Menz HB. Impact of chronic plantar heel pain on health-related quality of life. J Am Podiatr Med Assoc. 2008; 98:283–289. PMID: 18685048.

5. Stuber K, Kristmanson K. Conservative therapy for plantar fasciitis: a narrative review of randomized controlled trials. J Can Chiropr Assoc. 2006; 50:118–133. PMID: 17549177.
6. McMillan AM, Landorf KB, Barrett JT, Menz HB, Bird AR. Diagnostic imaging for chronic plantar heel pain: a systematic review and meta-analysis. J Foot Ankle Res. 2009; 2:32. PMID: 19912628.

7. Osborne HR, Allison GT. Treatment of plantar fasciitis by LowDye taping and iontophoresis: short term results of a double blinded, randomised, placebo controlled clinical trial of dexamethasone and acetic acid. Br J Sports Med. 2006; 40:545–549. PMID: 16488901.
8. Healey K, Chen K. Plantar fasciitis: current diagnostic modalities and treatments. Clin Podiatr Med Surg. 2010; 27:369–380. PMID: 20691370.

9. Donley BG, Moore T, Sferra J, Gozdanovic J, Smith R. The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot Ankle Int. 2007; 28:20–23. PMID: 17257533.

10. Hyland MR, Webber-Gaffney A, Cohen L, Lichtman PT. Randomized controlled trial of calcaneal taping, sham taping, and plantar fascia stretching for the short-term management of plantar heel pain. J Orthop Sports Phys Ther. 2006; 36:364–371. PMID: 16776486.

11. Roos E, Engstrom M, Soderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int. 2006; 27:606–611. PMID: 16919213.

12. Kalaci A, Cakici H, Hapa O, Yanat AN, Dogramaci Y, Sevinc TT. Treatment of plantar fasciitis using four different local injection modalities: a randomized prospective clinical trial. J Am Podiatr Med Assoc. 2009; 99:108–113. PMID: 19299346.
13. Thomson CE, Crawford F, Murray GD. The effectiveness of extra corporeal shock wave therapy for plantar heel pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2005; 6:19. PMID: 15847689.

14. Othman AM, Ragab EM. Endoscopic plantar fasciotomy versus extracorporeal shock wave therapy for treatment of chronic plantar fasciitis. Arch Orthop Trauma Surg. 2010; 130:1343–1347. PMID: 20033696.

15. Lynn SK, Padilla RA, Tsang KK. Differences in static- and dynamic-balance task performance after 4 weeks of intrinsic-foot-muscle training: the short-foot exercise versus the towel-curl exercise. J Sport Rehabil. 2012; 21:327–333. PMID: 22715143.

16. Wearing SC, Smeathers JE, Yates B, Sullivan PM, Urry SR, Dubois P. Sagittal movement of the medial longitudinal arch is unchanged in plantar fasciitis. Med Sci Sports Exerc. 2004; 36:1761–1767. PMID: 15595298.

17. Ribeiro AP, Trombini-Souza F, Tessutti V, Rodrigues Lima F, Sacco Ide C, Joao SM. Rearfoot alignment and medial longitudinal arch configurations of runners with symptoms and histories of plantar fasciitis. Clinics (Sao Paulo). 2011; 66:1027–1033. PMID: 21808870.

18. Daly PJ, Kitaoka HB, Chao EY. Plantar fasciotomy for intractable plantar fasciitis: Clinical Results and Biomechanical Evaluation. Foot Ankle. 1992; 13:188–195. PMID: 1634150.

Fig. 1
Description of arch building gait. (A) Resting foot (barefoot). (B) Contracted foot (arch building).
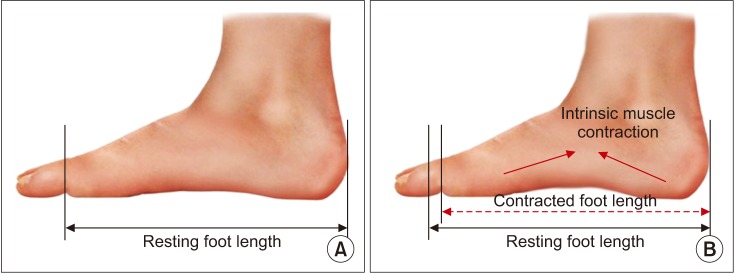
Fig. 2
Center of pressure parameters. (A) Gait line length. (B) Single support line. (C) Anterior/posterior position. (D) Lateral symmetry.
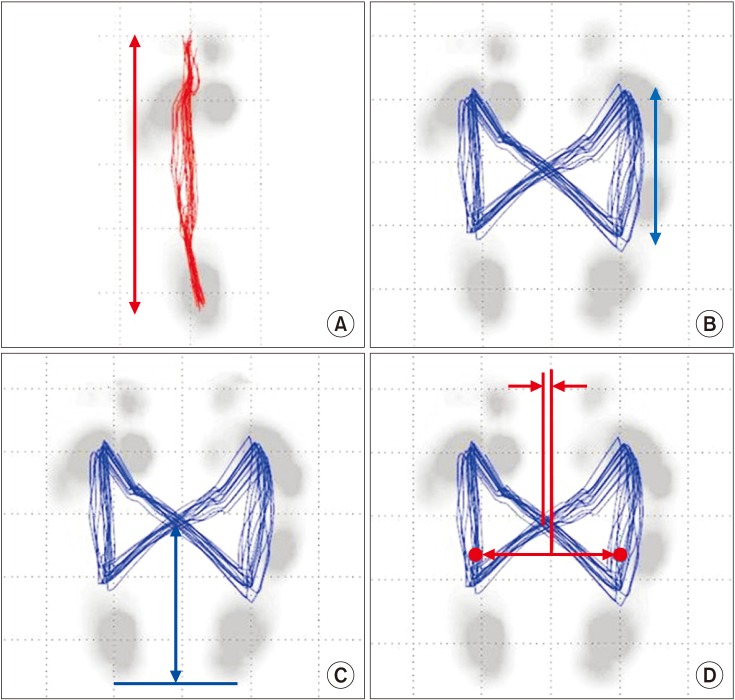
Fig. 3
Arch building gait. The data was presented by Zebris system (Zebris Medical GmbH, Isny im Allgau, Germany). COP, center of pressure.
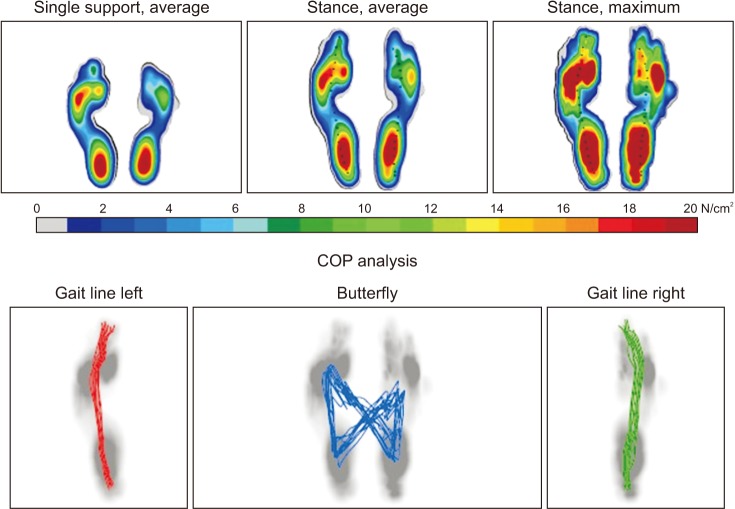
Fig. 4
Barefoot gait. The data was presented by Zebris system (Zebris Medical GmbH, Isny im Allgau, Germany). COP, center of pressure.
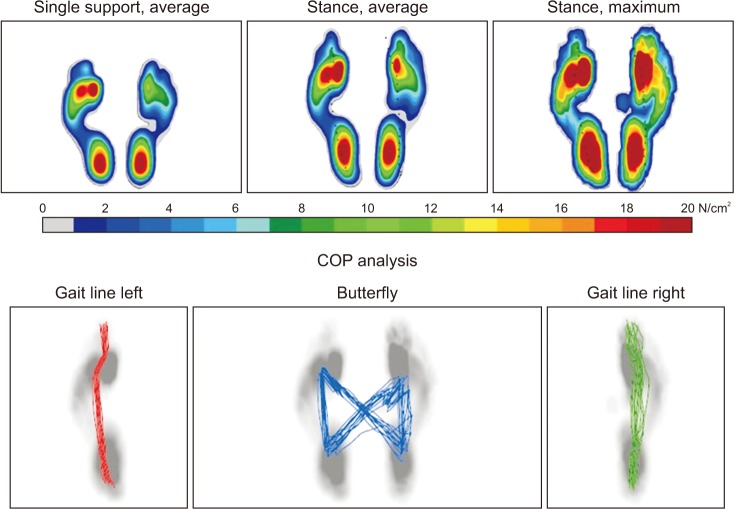
Table 1
The demographic characteristics of the control group (Group A) and the plantar fasciitis groups—bilateral (Group B), unilateral (Group C)
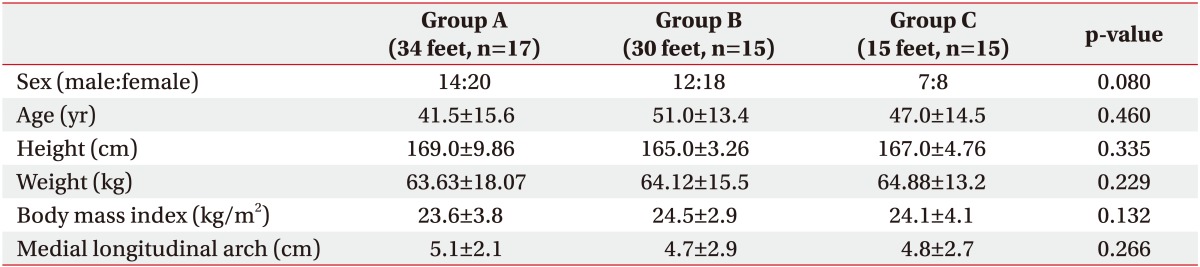
Table 2
A comparison of both plantar fasciitis groups (bilateral, unilateral) and the control group on barefoot gait analysis
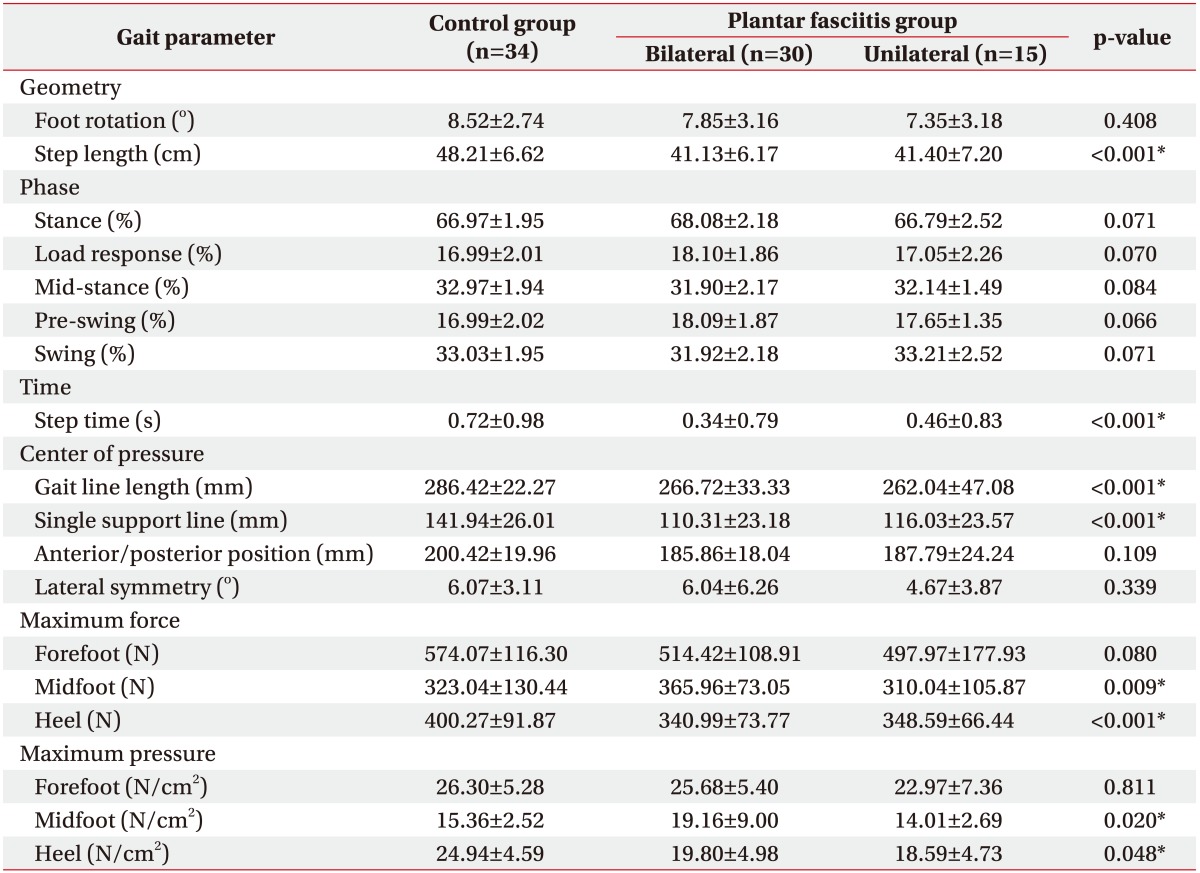
Table 3
A comparison of the plantar fasciitis groups (bilateral, unilateral) and the control group during arch building gait




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download