Abstract
Peroneal neuropathy is a common mononeuropathy of the lower limb. Some studies have reported cases of peroneal neuropathy after vascular surgery or intervention. However, no cases of peroneal neuropathy with occlusion of a single peripheral artery have been previously reported. A 73-year-old man was referred with a 3-week history of left-sided foot drop. He had a history of valvular heart disease and arrhythmia, and had previously been treated with percutaneous coronary intervention. Computed tomography angiogram of the lower extremity showed proximal occlusion of the left anterior tibial artery. An electrodiagnostic study confirmed left common peroneal neuropathy. After diagnosis, anticoagulation therapy was started and he received physical therapy.
Peroneal neuropathy is a common mononeuropathy of the lower extremities [1]. Clinically, peroneal neuropathy can be seen in various conditions, such as compression, trauma, fracture, and stretching.
Some cases of peroneal neuropathy after vascular surgery or intervention have been reported [234]. However, there have been no reported cases of peroneal neuropathy with specific occlusion of a peripheral artery. Here, we present one such case of a patient with foot drop and single arterial occlusion in the lower limb.
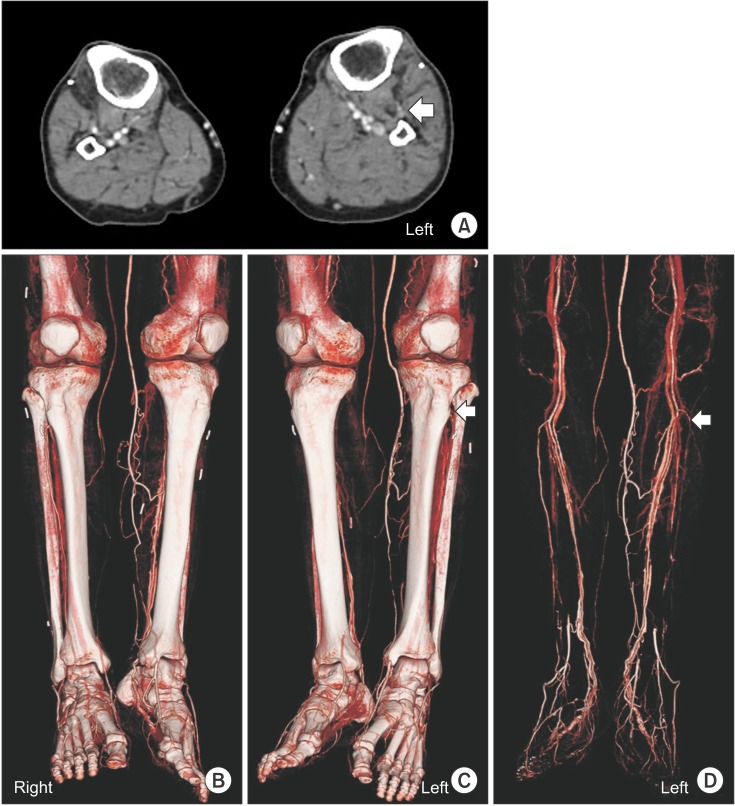
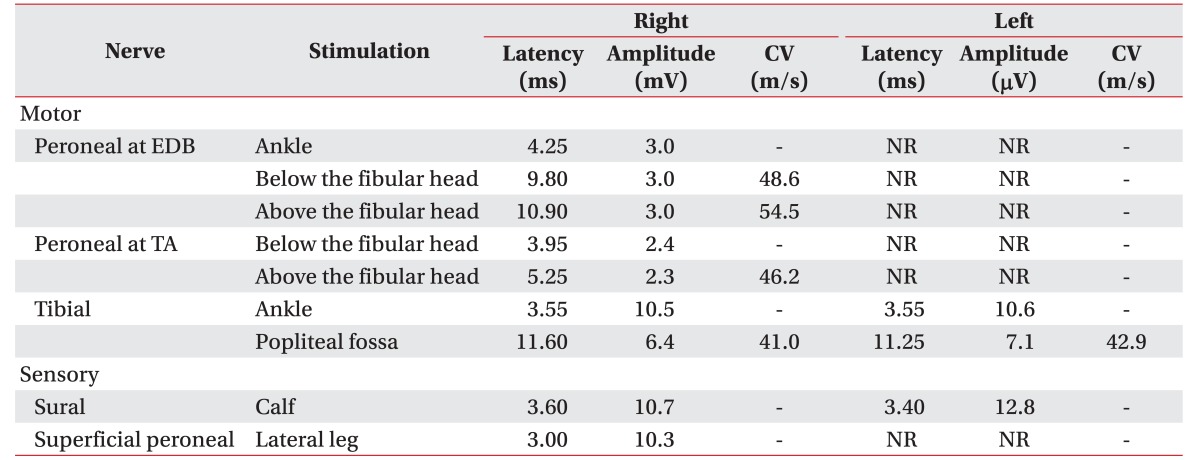
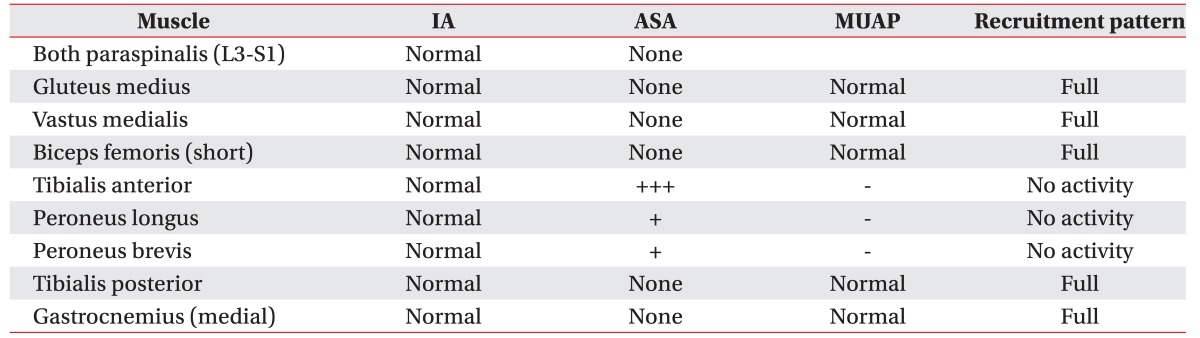
A 73-year-old male (height, 158 cm; weight, 62 kg) was referred by the cardiology department to the rehabilitation department because of a 3-week history of left foot drop. He also complained of numbness and a tingling sensation on the left lateral side of the lower leg and dorsum of the foot. At the time of referral, the left leg and foot were soft and non-tender. Only the right dorsalis pedis was pulsatile, but not on the left side. Pain in the left lateral lower leg and dorsum of foot was scored 3/10 on the Numeric Pain Rating Scale. The Medical Research Council scale for weakness showed the following grades (right/left): hip extension 5/5, knee flexion 5/5, ankle dorsiflexion 5/1, and hallucis extension 5/1. He had no lower back pain and the straight leg raise reached 80° on both sides. A positive Tinel's sign behind the fibular neck on the left side was noted. In a nerve conduction study, there was no compound motor action potential in the left deep peroneal nerve on the left extensor digitorum brevis or tibialis anterior muscle recordings, and no evoked sensory nerve action potential in the left superficial peroneal nerve (Table 1). Needle electromyography showed abnormal spontaneous activity at rest and no motor unit action potential activity in the left tibialis anterior, peroneus longus, and peroneus brevis muscles (Table 2). Computed tomography (CT) angiogram showed proximal occlusion of the left anterior tibial artery (ATA) (Fig. 1) without any abnormal findings of the soft tissue. This led to a diagnosis of left common peroneal neuropathy due to occlusion of the left ATA. The patient was treated with oral warfarin.
The patient's medical history was reviewed. He did not have diabetes mellitus. He received a mitral valve replacement 5 years ago due to mitral stenosis, and echocardiography showed a moderate degree of aortic stenosis and regurgitation. In addition, he had complete atrioventricular block and valvular atrial fibrillation; and had a pacemaker inserted three years prior to referral. However, he had been prescribed only an antiplatelet agent because of a history of cerebellar intracranial hemorrhage 2 years previously.
Approximately 4 weeks prior to referral, he visited another hospital suffering from chest pain, and received percutaneous coronary angiography which took about 30 minutes. After percutaneous coronary angiography, he received conservative care in a general ward, without any physical restrain or requirement for absolute bed rest. He could ambulate the ward with only minimal assistance. Some days later, he complained of left leg weakness and a brain CT was performed to rule out an acute brain lesion. Magnetic resonance imaging (MRI) was contraindicated because of the cardiac pacemaker. The brain CT showed a subacute ischemic lesion in the right posterior temporal region but it did not clinically correlate with the weakness. Although he complained of foot drop and paresthesia, there were no symptoms of anterior compartment syndrome such as tenderness, redness or swelling of low leg. No deep vein thrombosis or abnormal findings of soft tissues were found upon ultrasonography of the left leg. After improvement of the chest pain, he was discharged home. Two weeks later he was admitted to the cardiology department in the present hospital due to chest pain, and was referred to the rehabilitation department. After diagnosis of the left common peroneal neuropathy and improvement of the chest discomfort with conservative therapy, he was transferred and received rehabilitation.
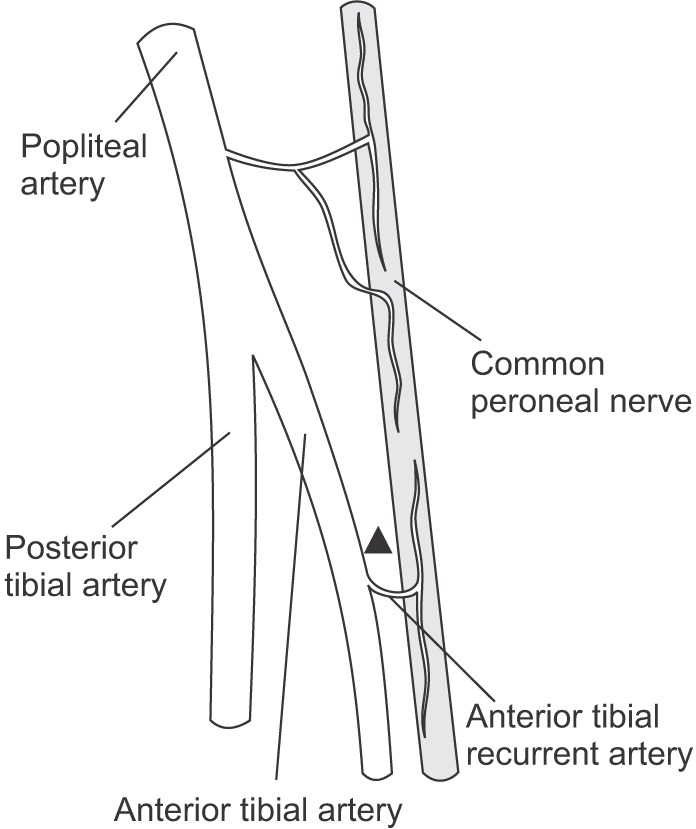
Peroneal neuropathy is either caused by prolonged posture (23.1%), surgical complication (20.3%), weight loss (14.5%), trauma (11.6%), or is idiopathic (16%) [1]. Although ischemia also has been implicated as one of the causes, this is the first reported case of ischemic common peroneal neuropathy induced by occlusion of the artery supplying nerve. There is currently a lack of research concerning the blood supply of the common peroneal nerve (CPN). It is known that the CPN has fewer supplying arteries and anastomoses than the tibial or sciatic nerves [5]. This suggests a potentially increased susceptibility of the peroneal nerve to compression, trauma, or other ischemic damage. According to a study by Kadiyala et al. [6], a single branch from the popliteal artery supplies the CPN in the popliteal fossa and the anterior recurrent tibial artery that branches from the ATA supplies the nerve distal to the fossa. In their study, these arteries anastomose at a point 30 to 60 mm distal to the mid-point of the popliteal fossa (Fig. 2). However, the distance between these vasa nervorum is 116 mm on average, whereas the distance between vasa nervorum of the tibial nerve is 41 mm on average. Because the distance between the vasa nervorum of the CPN is longer and supply lesser intraneural vessels, CPN has poor vascularization and is vulnerable to ischemic damage. In the study of Ryan et al. [7], the mean distance of the distal common peroneal nerve from the fibular apex to the deep and superficial peroneal bifurcation point in males was 37.6 mm. Based on this anatomy, and the ischemic susceptibility of the distal common peroneal nerve, tibialis anterior and peroneus longus muscles that are innervated by nerve branches from CPN could be damaged from ischemic injury and show abnormal findings in needle electromyography. We reviewed previous studies concerning ischemic peroneal neuropathy. One case reported femoral bypass surgery as a potential cause of the peroneal and tibial neuropathy [3]. In another case, peroneal palsy was reported after over 5 hours of leg ischemia due to femoral artery cannulation when performing cardiopulmonary bypass [2]. Although this case discusses the ischemic vulnerability of peroneal nerve, it deals with the ischemic insult of proximal artery of lower extremity, similar to previous report. Moreover, we could not figure out other ischemic insults of peripheral nerves such as the tibial nerve, because there was no clinical information such as electrodiagnostic findings, symptoms and physical examination. Unlike that case, we report that the common peroneal neuropathy occurred as a result of the specific supplying arterial occlusion. The other report presented a case of sciatic neuropathy that resulted from thromboembolism secondary to a femoral artery aneurysm, with ischemic injury due to nutrient artery obstruction [8]. McDermott et al. [9] suggested that peripheral arterial disease impairs peroneal nerve function. In our case, ankle brachial index of affected leg was 90.5, which was in the normal range of ankle brachial index. However, there were no reports of a case of an ischemic peroneal nerve injury from occlusion of single artery supplying peripheral nerve. We report the ischemic common peroneal neuropathy due to occlusion of supplying artery without underlying peripheral arterial disease, which makes our case unique. In 1966, Machacek and Machacek [10] reported a case of unilateral foot drop, after trauma. Clinical necrosis of the lower leg muscle was found, and surgery was performed. At postoperative angiography, there was an occlusion at the ATA. The foot drop in this case was thought to be due to anterior compartment syndrome which caused insult of lower leg muscles and peripheral nerves. This is dissimilar with our case in that there was no definite clinical evidence of anterior compartment syndrome.
In our case, the patient had no history of direct trauma or compression. However, he had a high risk of thromboembolism because of a history of percutaneous coronary intervention at symptom onset, arrhythmia, and valvular heart disease, with a mitral valve replacement. In addition, there was no radicular pain or symptoms suggestive of lumbosacral radiculopathy. Although a brain MRI could not be performed due to an implanted pacemaker, the presence of a subacute cerebral ischemic lesion suggests that there was a systemic thromboembolic event at the time of symptom onset. Therefore, after ruling out other possibilities, proximal occlusion of the ATA was thought to cause the peroneal neuropathy in this case.
Arterial occlusion-induced CPN palsy is rare and can be easily misdiagnosed. If foot drop occurred in patients with a risk factor of vascular embolism or thrombosis, an ischemic insult to the peroneal nerve should be part of the differential diagnosis. In addition to compression and trauma, nutrient arterial occlusion can be a cause of peroneal neuropathy. Special studies, such as CT angiogram or vascular sonography, could be seriously considered. Furthermore, we can conclude that the ATA has an important role in the blood supply to the CPN.
References
1. Aprile I, Caliandro P, La Torre G, Tonali P, Foschini M, Mondelli M, et al. Multicenter study of peroneal mononeuropathy: clinical, neurophysiologic, and quality of life assessment. J Peripher Nerv Syst. 2005; 10:259–268. PMID: 16221285.

2. Okada K, Sueda T, Shikata H, Orihashi K, Morita S, Hirai S, et al. Evoked spinal cord potential monitoring reveals peroneal nerve ischemia during thoracoabdominal repair: a case report. Ann Thorac Cardiovasc Surg. 1999; 5:350–352. PMID: 10550725.
3. Sprowson AP, Rankin K, Shand JE, Ferrier G. Common peroneal and posterior tibial ischemic nerve damage, a rare cause. Foot Ankle Surg. 2010; 16:e16–e17. PMID: 20483119.

4. Giannakopoulou C, Korakaki E, Hatzidaki E, Manoura A, Aligizakis A, Velivasakis E. Peroneal nerve palsy: a complication of umbilical artery catheterization in the full-term newborn of a mother with diabetes. Pediatrics. 2002; 109:e66. PMID: 11927739.

5. Ugrenovic SZ, Jovanovic ID, Kovacevic P, Petrović S, Simic T. Similarities and dissimilarities of the blood supplies of the human sciatic, tibial, and common peroneal nerves. Clin Anat. 2013; 26:875–882. PMID: 23280564.

6. Kadiyala RK, Ramirez A, Taylor AE, Saltzman CL, Cassell MD. The blood supply of the common peroneal nerve in the popliteal fossa. J Bone Joint Surg Br. 2005; 87:337–342. PMID: 15773642.

7. Ryan W, Mahony N, Delaney M, O'Brien M, Murray P. Relationship of the common peroneal nerve and its branches to the head and neck of the fibula. Clin Anat. 2003; 16:501–505. PMID: 14566896.

8. Eguchi K, Majima M. Sciatic neuropathy caused by disorder of a nutrient artery: a case report of thromboembolism secondary to profunda femoral artery aneurysm. Arch Phys Med Rehabil. 2001; 82:253–255. PMID: 11239320.

9. McDermott MM, Sufit R, Nishida T, Guralnik JM, Ferrucci L, Tian L, et al. Lower extremity nerve function in patients with lower extremity ischemia. Arch Intern Med. 2006; 166:1986–1992. PMID: 17030832.

10. Machacek J, Machacek F. Unusual cause of the peroneal nerve paralysis (Contribution on the “syndrome of the anterior tibial artery”). Z Orthop Ihre Grenzgeb. 1966; 102:317–321. PMID: 4385147.
Fig. 1
Computed tomography angiography of the lower extremities. (A) An axial image showing proximal occlusion of the left anterior tibial artery (arrow). (B, C, D) Three-dimensional reconstruction images demonstrate the left anterior tibial artery occlusion at the level of the fibular neck (arrow).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download