INTRODUCTION
According to Lance [
1], spasticity is commonly defined as a disorder of the sensorimotor system, characterized by a velocity-dependent increase in tonic stretch reflexes (‘muscle tone’) and exaggerated tendon jerks, as a result of hyperexcitability of the stretch reflex; moreover, spasticity is typical of upper motor neuron syndrome. The pathophysiological mechanisms of spasticity involve abnormalities in intraspinal processing, which usually regulates the excitatory and inhibitory signals in the intraspinal circuit, as well as imbalances in descending regulations, which modulate the excitatory and inhibitory descending inputs from the supraspinal roots [
2].
Spasticity is a common complication after stroke; onset may range from a few days to 18 months [
3]. The prevalence of spasticity ranges from 19% to 92% overall, and may reach up to 42.6% at 6 months after stroke [
24]. Although spasticity has positive effects, such as functional support of gait or standing in stroke patients, it also causes problems such as limitations of joint range of movement, difficulty in daily activities, pain, caregiver burden, and increase in treatment cost [
56]. Approximately 4% of patients with severe spasticity require interventions [
3]. The management of spasticity includes treatments such as range of motion exercises focusing on stretching, physical modalities, oral medications, intrathecal infusion of medications, and surgical interventions, including muscle tendon transfer [
6]. Extracorporeal shock-wave therapy (ESWT) has recently been applied as a noninvasive therapy for spasticity after stroke.
A shock wave is a sequence of single acoustic pulses, characterized by a high peak pressure, rapid pressure increase, short duration of application, and rapid propagation in three-dimensional spaces [
7]. The principles of shock-wave therapy are based on tensile forces in the negative phase, which generate cavitation bubbles, shear forces that are called a ‘jet stream,’ and the reflection of positive pressure that directly transfers energy to the target tissue [
89]. Several studies have shown that ESWT is effective for treating spasticity after stroke [
710]. In a meta-analysis of five studies, Lee et al. [
10] assessed the effect of ESWT in cases of spasticity after brain injury, and found a significant improvement (compared to the baseline values) in the Modified Ashworth Scale (MAS) after four ESWT sessions. In addition, Dymarek et al. [
7] reviewed articles on the antispasticity effect of ESWT over the last 10 years. Of 91 clinical articles identified, 8 showed relevant effects of ESWT on spasticity in the upper and lower extremities. However, only one randomized, controlled study, evaluated via the Cochrane method, was on a treatment group with 5 ESWT sessions on the finger flexor muscles; the treated group showed much more improvements in the MAS grade than the control group did. ESWT may therefore be a safe treatment for cases of spasticity after stroke.
Although previous studies have assessed the effect of ESWT on spasticity, only a few reports have described how to maximize the effect of ESWT on the muscles. In an
in vivo study on healthy rats, Kenmoku et al. [
11] reported that ESWT led to the degeneration and reduction in the number of acetylcholine receptors in the neuromuscular junctions, which suggests that it may decrease spasticity. ESWT is usually applied on the muscle belly [
7].
Because ESWT is based on the penetration of single acoustic pulses into a limited area, it is important to know exactly how to apply it [
7]. Despite this, there was only one study that focused on the ESWT application sites [
12]. Bae et al. [
12] compared the effect of ESWT applied at the muscle belly and at the myotendinous junction, given that the Ib afferent fiber of the Golgi tendon in the myotendinous junction inhibits α motor neurons; they found that treatment at the myotendinous junction was more effective than that at the muscle belly. However, in that study, only a few patients were enrolled in each group (muscle belly, n=12; myotendinous junction, n=11), the ESWT was applied to only one muscle of the biceps brachii, and only two groups were compared. They emphasized that further study was needed to supplement their study, in order to have more reliable results about the effect of ESWT applied at the muscle belly and at the myotendinous junction on spasticity in stroke patients.
In our study, we aimed to compare the effects of ESWT applied at the muscle belly and at the myotendinous junction on spasticity in the upper and lower limbs of chronic stroke patients.
Go to :

DISCUSSION
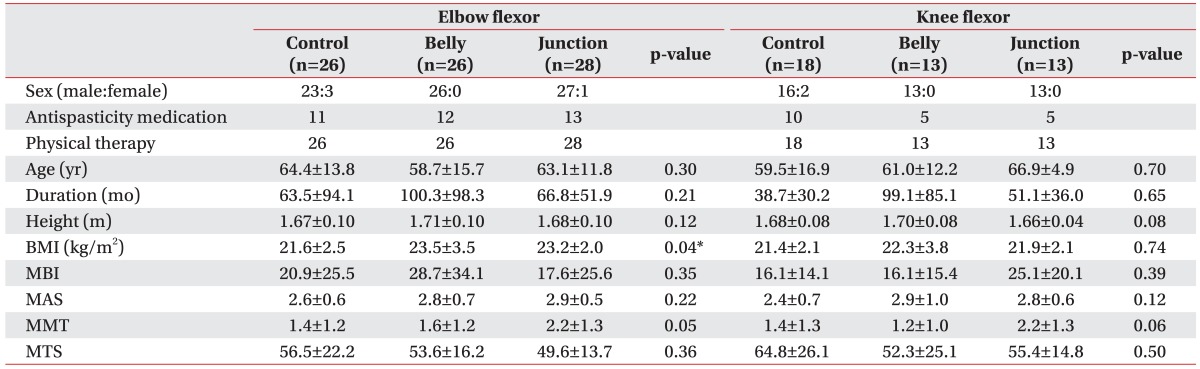
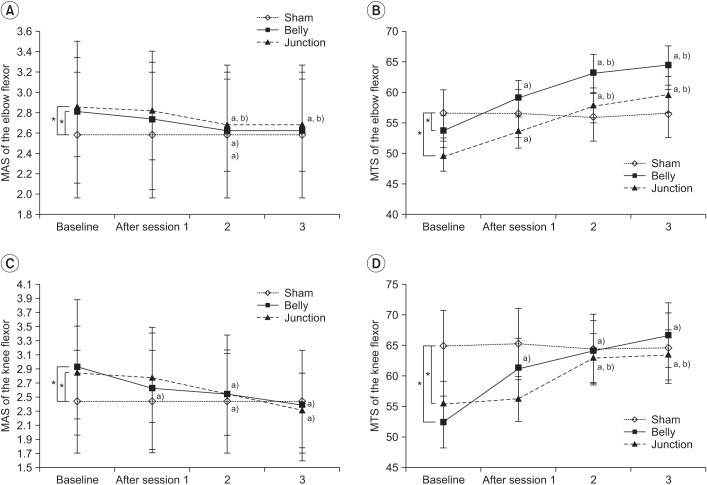
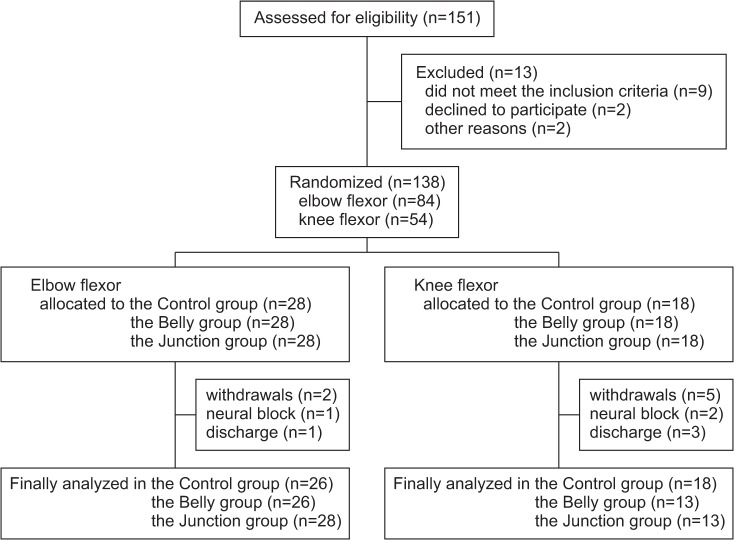
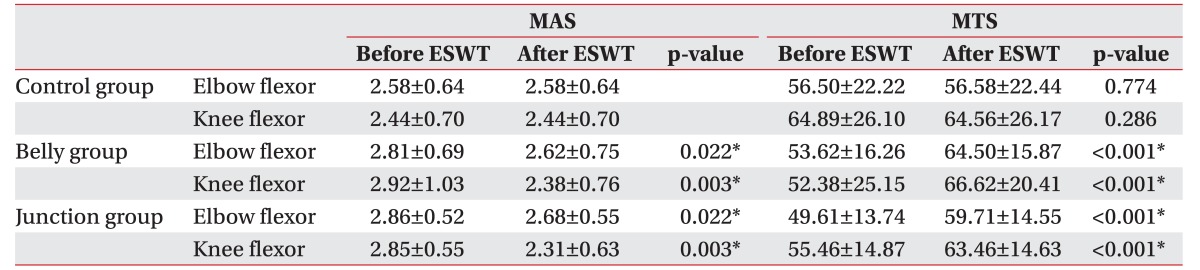
In this study, we sought to compare the effects of ESWT, applied at the belly or myotendinous junction, on the spasticity induced after stroke at the elbow and knee flexors in chronic patients. There was no significant difference in the MAS and MTS values between the belly and junction groups in both limbs. However, ESWT showed significant effects on spasticity at both sites, and progressive improvements were noted as the ESWT sessions were continued.
Several studies have described the effects of ESWT on stroke-induced spasticity [
712161718]. Yoo et al. [
16] reported that the stimulation of 21 chronic stroke patients with elbow flexor and wrist pronator spasticity led to significant improvements after 1 week, which persisted for at least 4 weeks. Moreover, the spasticity reduced as the number of sessions was increased. Sohn et al. [
17] stimulated the medial head of the gastrocnemius during 1 session (0.1 mJ/mm
2 and 1,500 shots) in chronic stroke patients, and found that the MAS of the ankle plantar flexor was significantly reduced. Moon et al. [
18] also stimulated the musculotendinous junction of the medial and lateral gastrocnemius three times (0.089 mJ/mm
2, 4 Hz, and 1,500 shots) in subacute stroke patients, and found that the ankle plantar flexor spasticity had significantly improved for at least a week after ESWT, but was not maintained for 4 weeks. The findings of this study are consistent with the abovementioned results. Although many previous studies have evaluated the effect of ESWT on spasticity, only a few studies have assessed the use of different application sites for obtaining better outcomes. One advantage of our randomized controlled study was the application of ESWT at sites of the muscle belly and myotendinous junction in both the upper and lower extremities, along with a control group.
The Golgi tendon in the myotendinous junction affects spasticity during the inverse stretch reflex via the Ib afferent fiber [
2]. Accordingly, we hypothesized that the effects of ESWT on spasticity may depend on the application site (muscle belly or myotendinous junction). In a study of 12 patients who underwent ESWT at the muscle belly and 11 patients who underwent ESWT at the myotendinous junction, Bae et al. [
12] reported that ESWT at the myotendinous junction yielded better results than ESWT at the muscle belly. In our study, we examined more patients (a total of 80 in the elbow flexor and 44 in the knee flexor muscles), performed ESWT at the upper and lower extremities, and also compared the results with a control group to improve the reliability. However, we did not observe a significant difference in the effects of ESWT between the muscle belly and myotendinous junction for both the elbow and knee flexor after treatment.
These findings may be associated with the mechanism of ESWT. Of several reported mechanisms underlying the effect of ESWT, the most widely reported is that shock waves induce the synthesis of nitric oxide, which plays major roles in vasodilatation, neoangiogenesis, increase of blood flow, and regulation of inflammation in many musculoskeletal diseases (plantar fasciitis, myofascial pain syndrome, and calcific tendinitis) [
192021]. Although the manner in which shock waves reduce spasticity remains unclear, previous studies [
1022] have suggested that the synthesis of nitric oxide reduces spasticity by means of an anti-inflammatory effect and by serving as a transmitter in the nervous system. Shock waves also alleviate the passive stiffness of muscles caused by connective tissue inactivity, and can affect muscle fibers around the tendon via direct mechanical stimuli. Most of the patients enrolled in this study were at a chronic stage after stroke (
Table 1). Spasticity in chronic patients could immobilize paralyzed muscles, which could consequently lead to soft tissue rearrangements, shortening of the muscles, and joint and soft tissue contracture. In addition, changes in muscle properties could also appear [
2]. Moreover, in chronic patients, ESWT may work by improving connective tissue stiffness and spastic muscle fibrosis [
7]. These findings were noted in both the muscle belly and myotendinous junction groups.
In addition, the finding that the MTS value of the elbow flexor showed significant improvements after even the first session may support the abovementioned reasoning. The improvements in the MTS value persisted throughout the sessions in both the belly and junction groups (
Fig. 2B). Moreover, the MTS value of the knee flexor had significantly improved after the first session in the belly group and the second session in the junction group (
Fig. 2D). The difference in the findings between the elbow and knee flexors might be explained as follows. Elbow flexion is primarily mediated by the biceps brachii and brachialis; in contrast, knee flexion is mediated through the activation of the semimembranosus, semitendinosus, biceps femoris, sartorius, popliteus, gastrocnemius, and gracilis muscles [
23]. In this study, we focused on the semitendinosus muscles in the knee flexors, although other muscles would still affect knee flexor spasticity. Very few studies have evaluated the effect of ESWT at each session on spasticity in chronic stroke patients. To our knowledge, this is the first study to evaluate the effect of ESWT for treating the stroke-induced spasticity in the upper and lower extremities evaluated after each session during the intervention period.
This study has certain limitations. First, subjects with stroke were at a chronic stage; for most, it had been more than 60 months since the onset. Hence, spasticity in acute or subacute stroke patients was not evaluated. Second, there were not enough participants for us to compare patients in the knee flexor group and elbow flexor group. There may be different results for the upper and lower limbs, depending on the application sites, as well as different muscle features. Third, the follow-up interval was only a week. According to other studies [
1622], the effect of ESWT is maintained for at least 4 and up to 12 weeks after treatment; hence, it is essential to assess how long the effect of ESWT persists for patients whose stroke occurred more than 5 years ago. Fourth, although our study was prospective, most of the patients enrolled were men. Hence, there is a need to evaluate whether the effect of ESWT for spasticity in women will show results similar to those for men.
However, this study also has strengths. First, it focused on the application site of ESWT on spastic muscles in upper and lower limbs. Although there have been many studies about the effect of ESWT on spasticity, few studies have evaluated the specific application sites. Second, this study attempted to compare the muscle belly and myotendinous junction sites with a control therapy group, which made this study more reliable than previous ones. Third, this study evaluated the effect of ESWT after each session. As a result, the serial effects of ESWT on spasticity were observed throughout the intervention period.
In this study, we compared the effects of ESWT, applied at the belly or myotendinous junction, on the spasticity induced after stroke at the elbow and knee flexors in chronic patients. The current study suggests that ESWT could be effective for treating spasticity after stroke, no matter which application site (muscle belly or myotendinous junction) is used. However, further studies are needed to establish how long the effect of ESWT on chronic stroke patients is maintained.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download