1. Bach JR. Paradigm paralysis in the management of neuromuscular disease. J Med Pers. 2013; 11:24–29.

2. Bach JR. Amyotrophic lateral sclerosis. Communication status and survival with ventilatory support. Am J Phys Med Rehabil. 1993; 72:343–349. PMID:
8260126.
3. Bach JR, Chiou M. Limitations of evidence-based medicine. Rev Port Pneumol. 2016; 22:4–5. PMID:
26850653.

4. Lisboa C, Diaz O, Fadic R. Noninvasive mechanical ventilation in patients with neuromuscular diseases and in patients with chest restriction. Arch Bronconeumol. 2003; 39:314–320. PMID:
12846961.
5. Bach JR, Alba A, Mosher R, Delaubier A. Intermittent positive pressure ventilation via nasal access in the management of respiratory insufficiency. Chest. 1987; 92:168–170. PMID:
3297517.

6. Mahajan KR, Bach JR, Saporito L, Perez N. Diaphragm pacing and noninvasive respiratory management of amyotrophic lateral sclerosis/motor neuron disease. Muscle Nerve. 2012; 46:851–855. PMID:
23042087.

7. Bach JR. Noninvasive respiratory management of high level spinal cord injury. J Spinal Cord Med. 2012; 35:72–80. PMID:
22525322.

8. Bolikal P, Bach JR, Goncalves M. Electrophrenic pacing and decannulation for high-level spinal cord injury: a case series. J Spinal Cord Med. 2012; 35:170–174. PMID:
22333657.

9. Bach JR, Takyi SL. Physical medicine interventions to avoid acute respiratory failure and invasive airway tubes. PM R. 2015; 7:871–877. PMID:
25772719.

10. Bach JR, Upadhyaya N. Association of need for tracheotomy with decreasing mechanical in-exsufflation flows in amyotrophic lateral sclerosis. Am J Phys Med Rehabil. 2017; 4. 13. [Epub]. DOI:
10.1097/PHM.0000000000000755.

11. Andersen T, Sandnes A, Brekka AK, Hilland M, Clemm H, Fondenes O, et al. Laryngeal response patterns influence the efficacy of mechanical assisted cough in amyotrophic lateral sclerosis. Thorax. 2017; 72:221–229. PMID:
27174631.

12. Bach JR, Bianchi C, Aufiero E. Oximetry and indications for tracheotomy for amyotrophic lateral sclerosis. Chest. 2004; 126:1502–1507. PMID:
15539719.

13. Wade OL, Gilson JC. The effect of posture on diaphragmatic movement and vital capacity in normal subjects with a note on spirometry as an aid in determining radiological chest volumes. Thorax. 1951; 6:103–126. PMID:
14846056.
14. Bach JR, Kang SW. Disorders of ventilation : weakness, stiffness, and mobilization. Chest. 2000; 117:301–303. PMID:
10669664.
15. Gay PC, Edmonds LC. Severe hypercapnia after low-flow oxygen therapy in patients with neuromuscular disease and diaphragmatic dysfunction. Mayo Clin Proc. 1995; 70:327–330. PMID:
7898136.

16. Chiou M, Bach JR, Saporito LR, Albert O. Quantitation of oxygen-induced hypercapnia in respiratory pump failure. Rev Port Pneumol. 2016; 22:262–265. PMID:
27118611.

17. Gomez-Merino E, Bach JR. Duchenne muscular dystrophy: prolongation of life by noninvasive ventilation and mechanically assisted coughing. Am J Phys Med Rehabil. 2002; 81:411–415. PMID:
12023596.
18. Bach JR, Alba AS. Management of chronic alveolar hypoventilation by nasal ventilation. Chest. 1990; 97:52–57. PMID:
2104793.

19. Bach JR, Alba AS, Bodofsky E, Curran FJ, Schultheiss M. Glossopharyngeal breathing and noninvasive aids in the management of post-polio respiratory insufficiency. Birth Defects Orig Artic Ser. 1987; 23:99–113.
20. Won YH, Choi WA, Lee JW, Bach JR, Park J, Kang SW. Sleep transcutaneous vs. end-tidal CO
2 monitoring for patients with neuromuscular disease. Am J Phys Med Rehabil. 2016; 95:91–95. PMID:
26135371.
21. Cinel D, Markwell K, Lee R, Szidon P. Variability of the respiratory gas exchange ratio during arterial puncture. Am Rev Respir Dis. 1991; 143:217–218. PMID:
1990930.

22. Bach JR, Bianchi C, Vidigal-Lopes M, Turi S, Felisari G. Lung inflation by glossopharyngeal breathing and “air stacking” in Duchenne muscular dystrophy. Am J Phys Med Rehabil. 2007; 86:295–300. PMID:
17413542.

23. Dail C, Rodgers M, Guess V, Adkins HV. Glossopharyngeal breathing. Downey: Rancho Los Amigos Hospital, Department of Physical Therapy;1979.
24. Dail CW, Affeldt JE. Glossopharyngeal breathing [Video]. Los Angeles: College of Medical Evangelists, Department of Visual Education;1954.
25. Webber B, Higgens J. Glossopharyngeal breathing what, when and how? [Video]. West Sussex: Aslan Studios Ltd;1999.
26. Chiou M, Bach JR, Jethani L, Gallagher MF. Active lung volume recruitment to preserve vital capacity in Duchenne muscular dystrophy. J Rehabil Med. 2017; 49:49–53. PMID:
27630091.

27. Kang SW, Bach JR. Maximum insufflation capacity. Chest. 2000; 118:61–65. PMID:
10893360.

28. Bach JR, Alba AS. Noninvasive options for ventilatory support of the traumatic high level quadriplegic patient. Chest. 1990; 98:613–619. PMID:
2203616.

29. Bach JR, Bianchi C. Prevention of pectus excavatum for children with spinal muscular atrophy type 1. Am J Phys Med Rehabil. 2003; 82:815–819. PMID:
14508413.

30. McKim DA, Griller N, LeBlanc C, Woolnough A, King J. Twenty-four hour noninvasive ventilation in Duchenne muscular dystrophy: a safe alternative to tracheostomy. Can Respir J. 2013; 20:e5–e9. PMID:
23457679.

31. Suri P, Burns SP, Bach JR. Pneumothorax associated with mechanical insufflation-exsufflation and related factors. Am J Phys Med Rehabil. 2008; 87:951–955. PMID:
18617862.

32. Bach JR, Mahajan K, Lipa B, Saporito L, Goncalves M, Komaroff E. Lung insufflation capacity in neuromuscular disease. Am J Phys Med Rehabil. 2008; 87:720–725. PMID:
18716483.

33. Ishikawa Y. Manual for the care of patients using noninvasive ventilation. Matsudo: Japan Planning Center;2005.
34. Bach JR, Alba AS, Shin D. Management alternatives for post-polio respiratory insufficiency. Assisted ventilation by nasal or oral-nasal interface. Am J Phys Med Rehabil. 1989; 68:264–271. PMID:
2686715.
35. Bach JR, Alba AS. Intermittent abdominal pressure ventilator in a regimen of noninvasive ventilatory support. Chest. 1991; 99:630–636. PMID:
1899821.

36. Bach JR, Radbourne M. A mechanical intermittent abdominal pressure ventilator. Am J Phys Med Rehabil. Forthcoming 2017.

37. Allen J. Pulmonary complications of neuromuscular disease: a respiratory mechanics perspective. Paediatr Respir Rev. 2010; 11:18–23. PMID:
20113987.

38. Bach JR, Robert D, Leger P, Langevin B. Sleep fragmentation in kyphoscoliotic individuals with alveolar hypoventilation treated by NIPPV. Chest. 1995; 107:1552–1558. PMID:
7781345.

39. Bach JR, Alba AS, Saporito LR. Intermittent positive pressure ventilation via the mouth as an alternative to tracheostomy for 257 ventilator users. Chest. 1993; 103:174–182. PMID:
8417874.

40. Richards GN, Cistulli PA, Ungar RG, Berthon-Jones M, Sullivan CE. Mouth leak with nasal continuous positive airway pressure increases nasal airway resistance. Am J Respir Crit Care Med. 1996; 154:182–186. PMID:
8680678.

41. Morelot-Panzini C, Le Pimpec-Barthes F, Menegaux F, Gonzalez-Bermejo J, Similowski T. Referred shoulder pain (C4 dermatome) can adversely impact diaphragm pacing with intramuscular electrodes. Eur Respir J. 2015; 45:1751–1754. PMID:
25900376.

42. DiPALS Writing Committee. Safety and efficacy of diaphragm pacing in patients with respiratory insufficiency due to amyotrophic lateral sclerosis (DiPALS): a multicentre, open-label, randomised controlled trial. Lancet Neurol. 2015; 14:883–892. PMID:
26234554.
43. DeLisa JA, Bach JR. Overview of rehabilitation, general evaluation principles and the rehabilitation team. In : Bach JR, editor. Pulmonary rehabilitation: the obstructive and paralytic conditions. Philadelphia: Hanley & Belfus;1996. p. 13–25.
44. Guerin C, Bourdin G, Leray V, Delannoy B, Bayle F, Germain M, et al. Performance of the coughassist insufflation-exsufflation device in the presence of an endotracheal tube or tracheostomy tube: a bench study. Respir Care. 2011; 56:1108–1114. PMID:
21801577.

45. Bach JR, Goncalves MR, Hamdani I, Winck JC. Extubation of patients with neuromuscular weakness: a new management paradigm. Chest. 2010; 137:1033–1039. PMID:
20040608.
46. Bach JR, Sinquee DM, Saporito LR, Botticello AL. Efficacy of mechanical insufflation-exsufflation in extubating unweanable subjects with restrictive pulmonary disorders. Respir Care. 2015; 60:477–483. PMID:
25492956.

47. Fishburn MJ, Marino RJ, Ditunno JF Jr. Atelectasis and pneumonia in acute spinal cord injury. Arch Phys Med Rehabil. 1990; 71:197–200. PMID:
2317137.
48. Garstang SV, Kirshblum SC, Wood KE. Patient preference for in-exsufflation for secretion management with spinal cord injury. J Spinal Cord Med. 2000; 23:80–85. PMID:
10914345.
49. Bach JR, Smith WH, Michaels J, Saporito L, Alba AS, Dayal R, et al. Airway secretion clearance by mechanical exsufflation for post-poliomyelitis ventilator-assisted individuals. Arch Phys Med Rehabil. 1993; 74:170–177. PMID:
8431102.
50. Barach AL, Beck GJ. Exsufflation with negative pressure; physiologic and clinical studies in poliomyelitis, bronchial asthma, pulmonary emphysema, and bronchiectasis. AMA Arch Intern Med. 1954; 93:825–841. PMID:
13157670.
51. Bach JR. Mechanical insufflation-exsufflation: comparison of peak expiratory flows with manually assisted and unassisted coughing techniques. Chest. 1993; 104:1553–1562. PMID:
8222823.
52. Bach JR. Conventional approaches to managing neuromuscular ventilation failure. In : Bach JR, editor. Pulmonary rehabilitation: the obstructive and paralytic conditions. Philadelphia: Hanley & Belfus;1996. p. 285–301.
53. Bach JR, Rajaraman R, Ballanger F, Tzeng AC, Ishikawa Y, Kulessa R, et al. Neuromuscular ventilatory insufficiency: effect of home mechanical ventilator use v oxygen therapy on pneumonia and hospitalization rates. Am J Phys Med Rehabil. 1998; 77:8–19. PMID:
9482374.

54. Toussaint M, Steens M, Wasteels G, Soudon P. Diurnal ventilation via mouthpiece: survival in end-stage Duchenne patients. Eur Respir J. 2006; 28:549–555. PMID:
16870671.

55. Bach JR, Goncalves MR, Hon A, Ishikawa Y, De Vito EL, Prado F, et al. Changing trends in the management of end-stage neuromuscular respiratory muscle failure: recommendations of an international consensus. Am J Phys Med Rehabil. 2013; 92:267–277. PMID:
23051760.

56. Goncalves MR, Bach JR, Ishikawa Y, Saporito , Winck JC. Continuous noninvasive ventilatory support outcomes for neuromuscular disease: a multicenter collaboration and literature review. Rev Port Pneumol. Forthcoming 2017.
57. Ishikawa Y, Miura T, Ishikawa Y, Aoyagi T, Ogata H, Hamada S, et al. Duchenne muscular dystrophy: survival by cardio-respiratory interventions. Neuromuscul Disord. 2011; 21:47–51. PMID:
21144751.

58. Bach JR. A comparison of long-term ventilatory support alternatives from the perspective of the patient and care giver. Chest. 1993; 104:1702–1706. PMID:
8252946.

59. Villanova M, Kazibwe S. New survival target for Duchenne muscular dystrophy. Am J Phys Med Rehabil. 2017; 96:e28–e30. PMID:
28099279.

60. Kohler M, Clarenbach CF, Boni L, Brack T, Russi EW, Bloch KE. Quality of life, physical disability, and respiratory impairment in Duchenne muscular dystrophy. Am J Respir Crit Care Med. 2005; 172:1032–1036. PMID:
15961695.

61. Villanova M, Brancalion B, Mehta AD. Duchenne muscular dystrophy: life prolongation by noninvasive ventilatory support. Am J Phys Med Rehabil. 2014; 93:595–599. PMID:
24743468.
62. Mills B, Bach JR, Zhao C, Saporito L, Sabharwal S. Posterior spinal fusion in children with flaccid neuromuscular scoliosis: the role of noninvasive positive pressure ventilatory support. J Pediatr Orthop. 2013; 33:488–493. PMID:
23752144.
63. Bach JR, Tuccio MC, Khan U, Saporito LR. Vital capacity in spinal muscular atrophy. Am J Phys Med Rehabil. 2012; 91:487–493. PMID:
22469873.

64. Bach JR, Gupta K, Reyna M, Hon A. Spinal muscular atrophy type 1: prolongation of survival by noninvasive respiratory aids. Pediatr Asthma Allergy Immunol. 2009; 22:151–162.

65. Schroth MK. Special considerations in the respiratory management of spinal muscular atrophy. Pediatrics. 2009; 123(Suppl 4):S245–S249. PMID:
19420154.

66. Bach JR. Case studies of respiratory management. Pulmonary rehabilitation: the obstructive and paralytic conditions. Philadelphia: Hanley & Belfus;1996. p. 331–346.
67. Bach JR, Penek J. Obstructive sleep apnea complicating negative-pressure ventilatory support in patients with chronic paralytic/restrictive ventilatory dysfunction. Chest. 1991; 99:1386–1393. PMID:
2036820.

68. Bach JR. New approaches in the rehabilitation of the traumatic high level quadriplegic. Am J Phys Med Rehabil. 1991; 70:13–19. PMID:
1994965.

69. McDermott I, Bach JR, Parker C, Sortor S. Customfabricated interfaces for intermittent positive pressure ventilation. Int J Prosthodont. 1989; 2:224–233. PMID:
2699419.
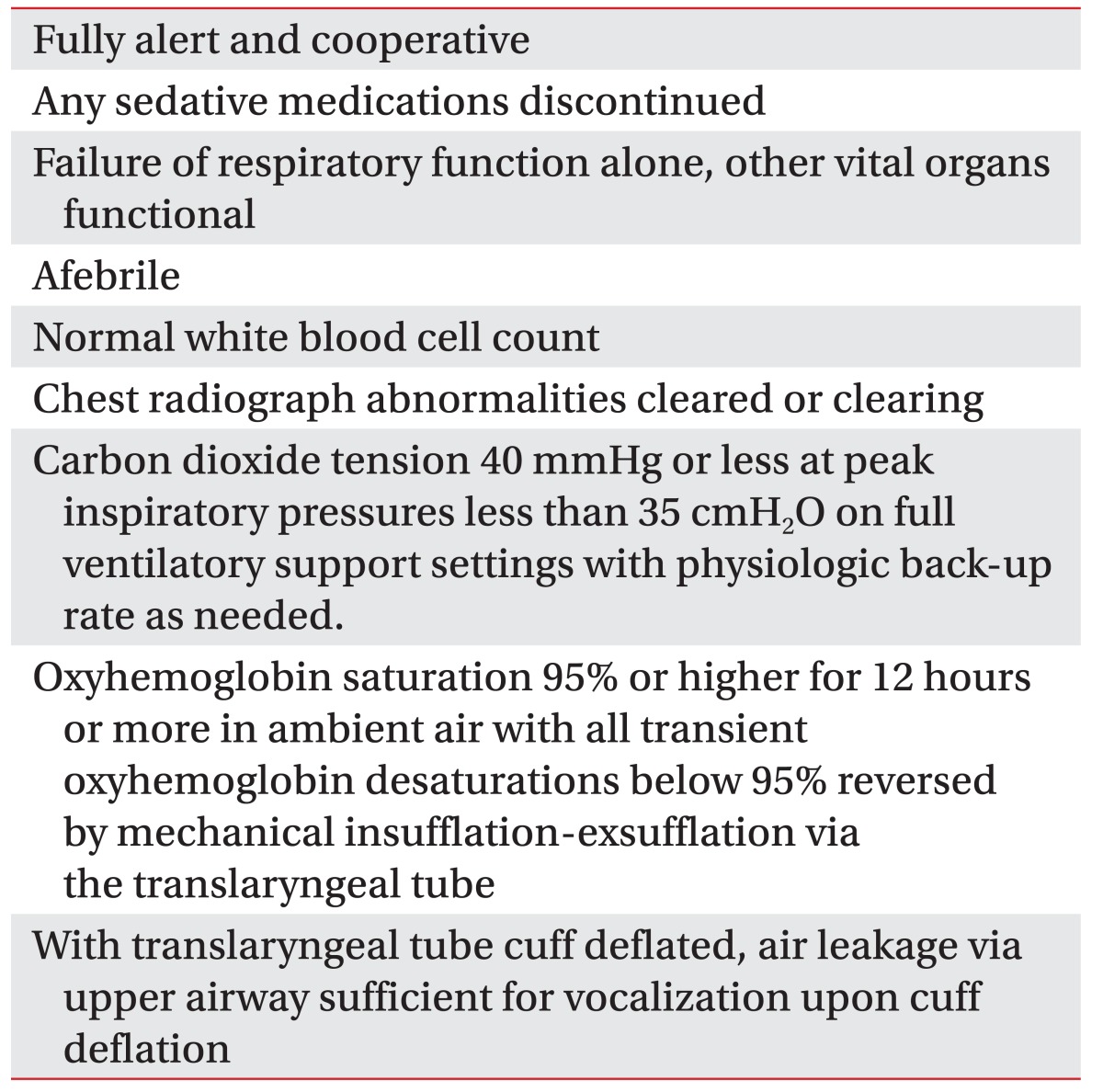
70. Bach JR, Saporito LR. Criteria for extubation and tracheostomy tube removal for patients with ventilatory failure: a different approach to weaning. Chest. 1996; 110:1566–1571. PMID:
8989078.
71. Bach JR, Saporito LR, Shah HR, Sinquee D. Decanulation of patients with severe respiratory muscle insufficiency: efficacy of mechanical insufflation-exsufflation. J Rehabil Med. 2014; 46:1037–1041. PMID:
25096928.

72. Chesoni SA, Bach JR, Okamura EM. Massive reflux and aspiration after radiographically inserted gastrostomy tube placement. Am J Phys Med Rehabil. 2015; 94:e6–e9. PMID:
25415397.

73. Bach JR, Gonzalez M, Sharma A, Swan K, Patel A. Open gastrostomy for noninvasive ventilation users with neuromuscular disease. Am J Phys Med Rehabil. 2010; 89:1–6. PMID:
20026942.

74. Banfi P, Volpato E, Valota C, D'Ascenzo S, Bani Alunno C. Noninvasive ventilation during feeding tube placement. Respir Care. Forthcoming 2017.
75. Ramalho RM, Coelho R, Bach JR. Gastrointestinal complications and enteral nutrition. In : Bach JR, editor. Physical medicine and rehabilitation interventions for skeletal and respiratory muscle dysfunction. [place unknown]: VentilaMed BreatheNVS;Forthcoming 2017.
76. Swan K, Kazanjian MS, Gulyas A. Swallowing and gastrointestinal concerns. In : Bach JR, editor. Management of patients with neuromuscular disease. Philadelphia: Hanley & Belfus;2004. p. 51–74.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download