Abstract
Objective
To report successful cases of extubation from invasive mechanical ventilation at our institution using pulmonary rehabilitation consisting of noninvasive ventilation (NIV) in neuromuscular patients with experience of reintubation.
Methods
Patients who experienced extubation failure via the conventional weaning strategy but afterwards had extubation success via NIV were studied retrospectively. Continuous end-tidal CO2 (ETCO2) and pulse oxyhemoglobin saturation (SpO2) monitoring were performed. Extubation success was defined as a state not requiring invasive mechanical ventilation via endotracheal tube or tracheotomy during a period of at least 5 days.
Go to : 
There is growing evidence that noninvasive ventilation (NIV) helps wean patients with chronic respiratory disease, mainly chronic obstructive pulmonary disease, off mechanical ventilation [123]. A recent meta-analysis found that NIV could be superior to the conventional weaning strategy, particularly in selected patients who exhibit an exacerbation of chronic obstructive pulmonary disease [4].
However, the efficacy of NIV in patients with weaning failure has not been formally assessed in a large case study, particularly for patients with ventilatory failure. Weaning often fails for mechanically ventilated patients who have chronic ventilatory failure from various causes. These include neuromuscular diseases (NMD), which can cause respiratory muscle weakness and result in gradual hypercapnia [56]. Acute illnesses, such as pneumonia or pulmonary embolus, may increase the respiratory workload, which can induce decompensation of the respiratory muscle in patients with chronic ventilatory failure. Such complications eventually require endotracheal intubation and invasive mechanical ventilation. The decision to extubate patients and wean them from mechanical ventilation is much more challenging when patients have advanced respiratory muscle weakness not bearable whole respiration already or develop repeated respiratory muscle fatigue. In some cases, extubation fails repeatedly, requiring the patients to undergo tracheotomy and prolonged invasive mechanical ventilation. A previous study demonstrated that when NIV is used on invasively mechanically ventilated NMD patients who cannot breathe autonomously and have low vital capacity (VC), it prevents reintubation, and eventually most such patients become dependent on NIV [7].
The purpose of this study was to ascertain whether NIV promotes successful weaning in neuromuscular patients with ventilatory failure. We focused on patients with experience of reintubation.
Go to : 
All patients who were admitted to Gangnam Severance Hospital from March 1, 2001, through December 30, 2013, and who experienced extubation failure by the conventional weaning strategy and reintubation, were identified by a retrospective chart review. Included patients were those who had been extubated in conjunction with NIV support and could maintain normal ventilation by routine daily use of NIV for 7–16 hours (part-time non-invasive aid) for at least 5 days after extubation without progressing to tracheotomy [89].
Weaning failure from invasive mechanical ventilation was defined as post-extubation respiratory failure in the 5-day period after discontinuation of invasive mechanical ventilation through endotracheal intubation. Respiratory failure was defined as follows: (1) respiratory acidosis (arterial pH of 7.35 or less with PaCO2 of 45 mmHg or more); (2) arterial O2 saturation by pulse oximetry less than 90% or PaO2 less than 60 mmHg at an inspired O2 fraction of 0.5 or more; (3) respiratory frequency exceeding 35/min; (4) decreased consciousness, agitation, or diaphoresis; and (5) clinical signs suggestive of respiratory muscle fatigue and/or increased work of breathing, such as the use of respiratory accessory muscles, paradoxic motion of the abdomen, or retraction of the intercostal spaces [2].
If at least two of these occurred, the patients were returned to invasive mechanical ventilation with reintubation.
After complications that significantly worsened the respiratory function of the patients (e.g., pneumonia) were solved, the patients were extubated directly to NIV support. They also had to be clinically stable at the time of extubation. NIV was provided via a combination of nasal or oronasal interfaces. The correct mask size was chosen for each patient on initiation of NIV. Initially, NIV was adjusted to maintain SpO2 greater than or equal to 95% and ETCO2 less than 40 mmHg in ambient air [710]. These initial settings and the type of mask were secondarily adjusted to assure the comfort and tolerance of the patient and to compensate for any air leaks. Thereafter, the NIV settings were adjusted to the gas analysis data and the continuously monitored SpO2 and ETCO2 levels, which were measured by Dash (Dash 400 Patient Monitor; GE Healthcare, Milwaukee, WI, USA). NIV therapy was considered to be successful if reintubation was avoided for at least 5 consecutive days after extubation [910].
The following data were collected from the case records: the duration of intubation and hospital stay, number of extubation failures, underlying condition(s), cause of respiratory failure that led to intubation, and complications during NIV. If available, the VCs and unassisted and assisted peak cough flows during hospitalization were recorded. All patients were followed up until hospital discharge. Our local Ethics Committee approved the study protocol (No. 3-2012-0022).
Go to : 
The sample in this study consisted of all 18 patients in the study period who required invasive mechanical ventilation, underwent extubation according to the conventional weaning strategy, had to be reintubated at least once, and were then successfully weaned from the invasive mechanical ventilator by NIV.
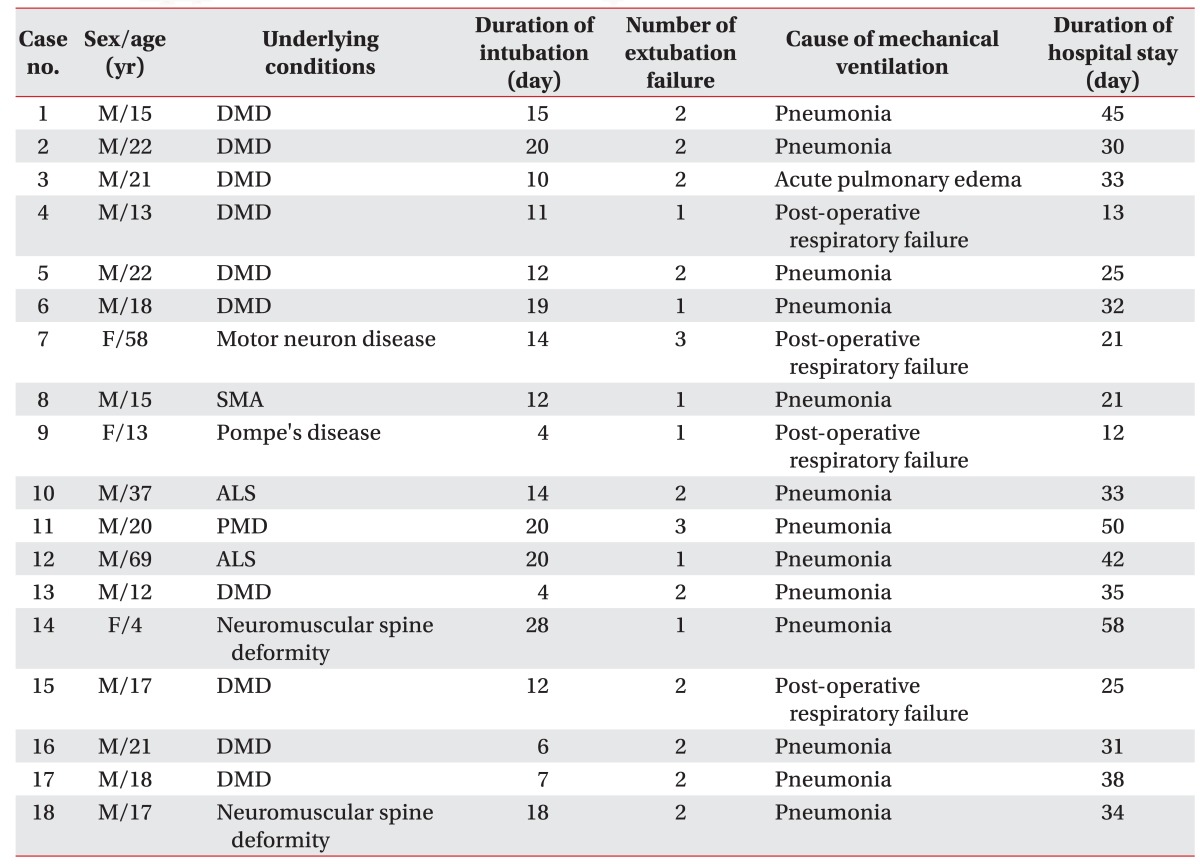
The 18 patients with NMD continued to have lower ventilator-free breathing ability and, consequently, had to use NIV on a part-time basis. None of the patients had undergone NIV before the intubation. None exhibited any serious or long-term NIV-related adverse effects. All patients left the hospital alive. The average duration of hospital stay, i.e., the follow-up period, was 32.1 days. The major cause of respiratory failure was pneumonia. Table 1 presents the demographic characteristics of the 18 subjects.
In eight cases (cases #1, #3, #10, #11, #13, and #16–18), NIV was also used as a rescue therapy for impending respiratory failure immediately after the second extubation, but these patients exhibited NIV intolerance: anxiety and consciousness deterioration. Thus, the first NIV trial failed, and the patients were reintubated. Thereafter, NIV was attempted again, and this time it succeeded after the extubation.
Case #2 failed the first NIV trial 2 days after the second extubation because of hemodynamic instability with cardiac arrest resulting from active upper gastrointestinal bleeding. Case #7 had motor neuron disease and, when in another hospital, had failed extubation supported by NIV in the bi-level positive airway pressure (biPAP) mode and the conventional weaning strategy. The subject showed hypercapnia and hypoxemia despite the NIV trial in the biPAP mode. Thereafter, the patient was transferred in an intubated state to our institution, where NIV was initiated in the ACV mode, which is the preferred ventilatory mode for NMD patients [8]. In addition, ventilator-free breathing tolerance was assessed by continuous monitoring to find out whether the daytime SpO2 and ETCO2 levels were within the normal ventilation status, and the patient eventually succeeded extubation.
The conditions of the remaining eight patients (cases #4–6, #8, #9, #12, #14, and #15) were worsened by respiratory complications such as pneumonia and post-operative respiratory failure. This caused the conventional weaning strategy to fail once or twice. However, all eight patients were successfully extubated to NIV at the first trial.
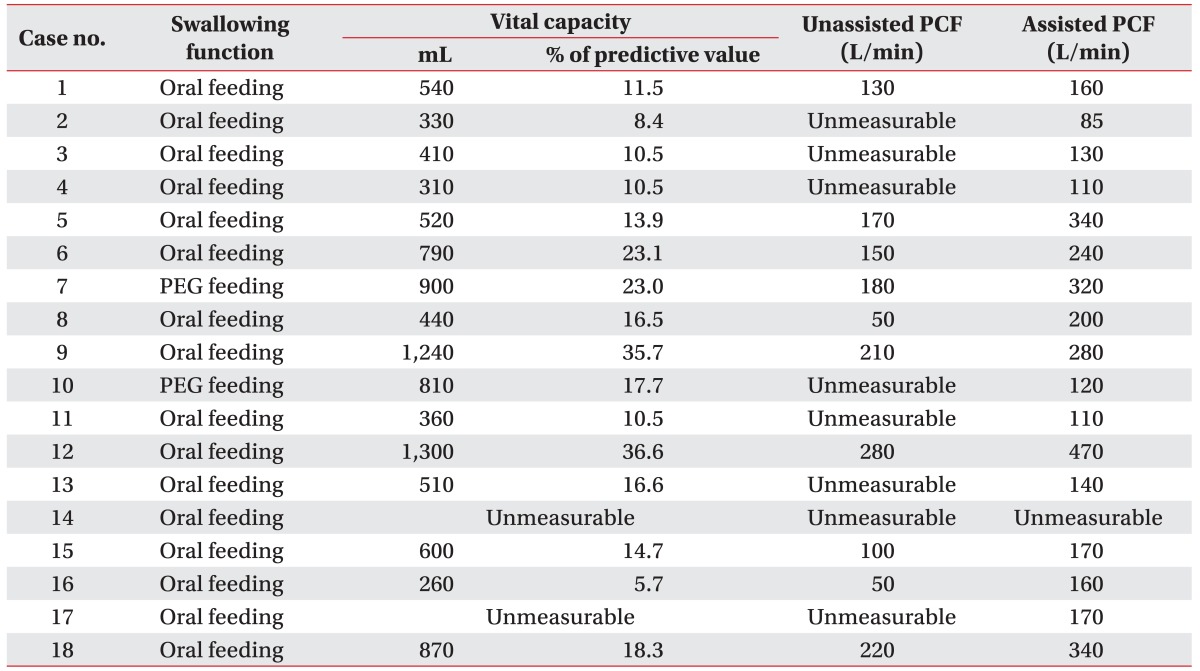
All of the patients maintained a normal ventilatory status (SpO2 and ETCO2) after successful extubation and remained stable until hospital discharge. The data on VC and peak cough flow as a variable of breathing ability are shown in Table 2.
Go to : 
The present study assessed whether NIV could help wean patients who had ventilatory failure, and who had already failed extubation at least once, off of invasive mechanical ventilation. Indeed, all such patients were discharged.
The reason for our patients' chronic ventilatory failure was NMD, which often induces weakness of the respiratory muscles and results in ventilatory insufficiency [1112]. Indeed, patients with NMD are highly likely to progress to invasive mechanical ventilation. In addition, atelectasis and pneumonia can complicate the course of NMD in these patients and promote their progression to acute respiratory failure and invasive mechanical ventilation. Bach et al. [7] reported that all 155 patients with NMD, respiratory muscle weakness, and low VCs could be successfully extubated by using NIV. However, it should be noted that their study included patients who had no ventilator-free breathing tolerance, whereas our study included patients who had already experienced extubation failure via the conventional weaning strategy.
NMDs are the most important cause of prolonged ventilator dependency, because they result in chronic ventilatory failure [13]. Since these patients inevitably develop neuromuscular ventilatory insufficiency, complete weaning from mechanical ventilation (i.e., the conventional concept of weaning) is usually not possible, especially in those who are severely disabled and breathe autonomously [7]. A previous study showed that all NMD patients can continue with noninvasive ventilation after the resolution of acute respiratory failure [14]. Daily NIV use is also currently recommended for NMD patients, as it was shown to prevent intubation and eventual tracheotomy [15]. Part-time NIV also facilitates the resumption of normal eating by creating ventilator-free time.
In the current study, all patients with ventilatory failure were successfully ventilated and discharged from the hospital. Although the first NIV attempt failed in 10 of the 18 patients, the second NIV led to subsequent extubation in all cases. Failed extubation with NIV can result from several factors, including the patient's inability to manage respiratory tract secretions, impaired mental status, and ineffective cough, with mucus plugging of the large airways [7]. In addition, Bach et al. [7] showed that a pre-intubation NIV experience was a good predictor of extubation success with NIV, probably because the patients are able to cooperate with NIV, which is an important factor. Indeed, Meduri et al. [16] suggested that personnel should undergo some training to optimize the routine daily use of NIV. Most of the NIV-intolerant cases in our study showed anxiety despite wanting to facilitate the use of NIV, probably because of lack of experience with NIV prior to the intubation.
Several other studies also suggested that NIV improves weaning success by reducing the risk of post-extubation respiratory failure [123]. However, our study has several design advantages. First, unlike the previous studies, our study involved only patients with ventilatory failure who had already experienced extubation failure. Second, NIV-induced weaning was considered successful only if reintubation did not occur within the 5-day period after extubation, a longer period than that of previous studies. Third, all patients in the present study were treated with NIV in an individualized manner, with a progressive method that was fine-tuned to the patient's condition and with continuously measured clinical variables, including SpO2 and ETCO2. By contrast, the previous studies applied NIV with a somewhat uniform fixed protocol.
Our study has some limitations, including the fact that it was an uncontrolled study. Second, the sample size was small. Third, there was a relatively short follow-up; therefore, the long-term effects of NIV after discharge remain unclear.
To our knowledge, this study is the first to review a series of NMD patients with extubation failure in terms of NIV-related extubation success. The present report highlights the effectiveness of the NIV strategy, which involves continuous monitoring that guides the NIV settings in an individualized and progressive manner. This suggests that NIV may be useful for NMD patients with ventilatory failure.
Go to : 
ACKNOWLEDGMENTS
This work was supported by a research grant from MEDILAB KOREA Co., Ltd. We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated.
Go to : 
References
1. Ferrer M, Sellares J, Valencia M, Carrillo A, Gonzalez G, Badia JR, et al. Non-invasive ventilation after extubation in hypercapnic patients with chronic respiratory disorders: randomised controlled trial. Lancet. 2009; 374:1082–1088. PMID: 19682735.

2. Esteban A, Frutos-Vivar F, Ferguson ND, Arabi Y, Apezteguia C, Gonzalez M, et al. Noninvasive positive-pressure ventilation for respiratory failure after extubation. N Engl J Med. 2004; 350:2452–2460. PMID: 15190137.

3. Nava S, Gregoretti C, Fanfulla F, Squadrone E, Grassi M, Carlucci A, et al. Noninvasive ventilation to prevent respiratory failure after extubation in high-risk patients. Crit Care Med. 2005; 33:2465–2470. PMID: 16276167.

4. Burns KE, Adhikari NK, Keenan SP, Meade M. Use of non-invasive ventilation to wean critically ill adults off invasive ventilation: meta-analysis and systematic review. BMJ. 2009; 338:b1574. PMID: 19460803.

5. Panitch HB. The pathophysiology of respiratory impairment in pediatric neuromuscular diseases. Pediatrics. 2009; 123(Suppl 4):S215–S218. PMID: 19420146.

6. Mehta S. Neuromuscular disease causing acute respiratory failure. Respir Care. 2006; 51:1016–1021. PMID: 16934165.
7. Bach JR, Goncalves MR, Hamdani I, Winck JC. Extubation of patients with neuromuscular weakness: a new management paradigm. Chest. 2010; 137:1033–1039. PMID: 20040608.
8. Bach JR, Rajaraman R, Ballanger F, Tzeng AC, Ishikawa Y, Kulessa R, et al. Neuromuscular ventilatory insufficiency: effect of home mechanical ventilator use v oxygen therapy on pneumonia and hospitalization rates. Am J Phys Med Rehabil. 1998; 77:8–19. PMID: 9482374.

9. Girault C, Daudenthun I, Chevron V, Tamion F, Leroy J, Bonmarchand G. Noninvasive ventilation as a systematic extubation and weaning technique in acute-on-chronic respiratory failure: a prospective, randomized controlled study. Am J Respir Crit Care Med. 1999; 160:86–92. PMID: 10390384.
10. Bach JR, Gonzalez M, Sharma A, Swan K, Patel A. Open gastrostomy for noninvasive ventilation users with neuromuscular disease. Am J Phys Med Rehabil. 2010; 89:1–6. PMID: 20026942.

11. Kilger E, Briegel J, Haller M, Frey L, Schelling G, Stoll C, et al. Effects of noninvasive positive pressure ventilatory support in non-COPD patients with acute respiratory insufficiency after early extubation. Intensive Care Med. 1999; 25:1374–1380. PMID: 10660844.

12. Rabinstein AA. Update on respiratory management of critically ill neurologic patients. Curr Neurol Neurosci Rep. 2005; 5:476–482. PMID: 16263060.

13. Spitzer AR, Giancarlo T, Maher L, Awerbuch G, Bowles A. Neuromuscular causes of prolonged ventilator dependency. Muscle Nerve. 1992; 15:682–686. PMID: 1508233.

14. Bach JR, Niranjan V, Weaver B. Spinal muscular atrophy type 1: a noninvasive respiratory management approach. Chest. 2000; 117:1100–1105. PMID: 10767247.
15. Bach JR, Martinez D. Duchenne muscular dystrophy: continuous noninvasive ventilatory support prolongs survival. Respir Care. 2011; 56:744–750. PMID: 21333078.

16. Meduri GU, Turner RE, Abou-Shala N, Wunderink R, Tolley E. Noninvasive positive pressure ventilation via face mask: first-line intervention in patients with acute hypercapnic and hypoxemic respiratory failure. Chest. 1996; 109:179–193. PMID: 8549183.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download