Abstract
Precise measurement of postvoid residual (PVR) urine volume is a key factor in assessing patients with voiding dysfunction, including those with lower urinary tract problems. The safe and noninvasive ultrasound bladder scan is the preferred mode to measure PVR volume. However, this procedure has a false-positive rate up to 9%, in the presence of ovarian cysts, renal cysts, ascites, or uterine myoma with cystic degeneration. Until now, cystic lesions are known to cause false positivity in ultrasound bladder scanner. However, we encountered falsely-elevated PVR in two cases of non-cystic uterine myomas. We present these cases with detailed radiologic images and volume measurement data.
Accurate measurement of postvoid residual (PVR) volume is important when assessing patients with voiding dysfunction, particularly patients with neurogenic bladder caused by cerebral infarction or spinal cord injury, or in patients with iatrogenic bladder injury [12]. Bladder scanning and urinary catheterization are the two main procedures for assessing PVR [3]. Urinary catheterization is the gold standard for measuring PVR, but has some limitations such as discomfort, low compliance, and risk of urinary tract infection or injury.
Ultrasonography has been widely used to measure PVR for the past 40 years due to its simplicity, safety, non-invasiveness, and painlessness [45]. However, false PVR results have been reported in cases with ovarian cysts, renal cysts, ascites, or uterine myoma with cystic degeneration [67]. Fluid collections may be misinterpreted as urinary retention, resulting in a false-positively elevated PVR.
However, no study has reported false-positive results from bladder scanners due to less cystic lesions such as uterine myoma. We report 2 cases of uterine myoma which dose not include fluid collections caused falsely-elevated PVR errors on ultrasound bladder scanner measurements.
A 47-year-old woman with gait disturbance was admitted to the Spine Center. Cervical spine magnetic resonance imaging showed C1 spinal cord atrophy. Ten days after admission, C1 laminectomy and occipito-cervical fusion (occiput to C6) were performed for spinal cord decompression and occipito-cervical stabilization. After surgery, the patient was transferred to Department of Rehabilitation Medicine for rehabilitation of gait disturbance and voiding difficulty.
A portable ultrasound bladder scanner (BioCon-500; Mcube Technology, Seoul, Korea) measured the PVR volume within 30 minutes of voiding. Complete emptying of the bladder with urethral catheterization was recommended when the PVR volume was over 100 mL. For patients with PVR volumes between 300–450 mL measured by the bladder scanner on initial several days, urethral catheterizations for emptying the bladder were performed immediately after the measurement. Medications such as cholinergic agents and alpha-blocker were administered. However, although the dosage was increased, PVR volume was constantly elevated, with no indications of any decrease. Interestingly, only 30–100 mL of PVR was consistently drained by catheterization, while the bladder scanner measured up to 300–450 mL. On the other hand, the portable ultrasound bladder scanner volumetry did not show discrepancies in other patients. We suspected some structural abnormality might be hindering complete catheter drainage of the residual urine, or that there might be some other underlying implication for the consistent error in the bladder scanner measurements for this patient.
An urodynamic study (UDS), intravenous pyelography (IVP), and voiding cystourethrogram (VCUG) were performed to assess the urinary tract; no significant abnormality was found in the voiding pattern, bladder shape, or urinary tract.
Further evaluation was performed by simultaneous modified VCUG examination and bladder scanner measurement, in order to find the reason for discrepancy observed between PVR measurement by bladder scanner and catheterization. Before the VCUG, the patient's bladder was completely emptied by catheterization. However, the bladder scanner showed 222 mL of PVR. Infusion of 200 mL of radiocontrast media into the bladder gave a readout of 460 mL of urine volume, when measured by the bladder scanner. After infusing 450 mL of radiocontrast media, 410 mL of urine was voided, but the PVR volume measured by the bladder scanner was 270 mL instead of 40 mL (Table 1, Fig. 1).
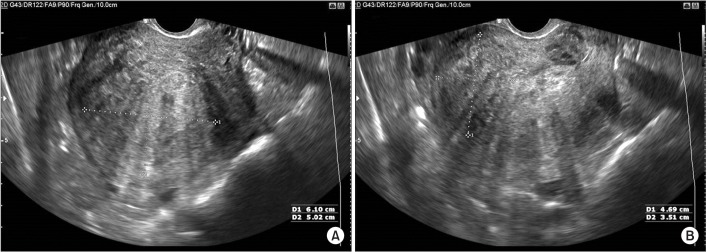
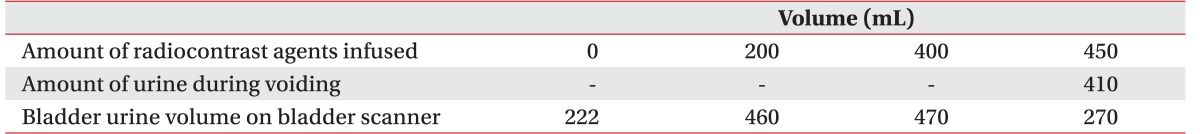
An X-ray image showed filling defect in the upper portion of the bladder after 200 mL radiocontrast agent infusion. We suspected mass lesions around the bladder (Fig. 1A). Abdominopelvic computed tomography was performed for further investigation, and several mass-like lesions were detected in the uterus. Endovaginal ultrasonography confirmed variable sized uterine myoma without secondary cystic changes (Fig. 2). The patient was hence referred to the Obstetrics & Gynecology Clinic for treatment of the myoma.
A 44-year old woman visited the Emergency Department with headache, and was diagnosed with subarachnoid hemorrhage due to ruptured anterior communicating artery aneurysm. The day she was admitted to the Department of Neurosurgery, the patient underwent a right frontal lobe craniotomy and aneurysm clipping.
The patient was transferred to the Department of Rehabilitation Medicine to receive rehabilitation therapy, 48 days after surgery. Upon transfer, the residual urine was 200–300 mL when measured by a portable bladder scanner, but 20–30 mL when measured by urethral catheterization, showing a considerable discrepancy. Considering that this patient's history included symptoms of frequency, incontinence, and severe menstrual pain, a gynecological cause was immediately suspected.
Endovaginal ultrasonography was performed 3 days after transfer to the Department of Rehabilitation Medicine. Two non-cystic uterine myoma masses were seen: one was 6.4 cm×5.8 cm size with 113 mL volume, and the other was 2.8 cm×2.6 cm size with 10 mL volume, as calculated by three-dimensional (3D) endovaginal ultrasonography [8]. The total 3D volume of the two myoma mass was 123 mL, which was the difference observed in PVR measurement by urethral catheterization and the bladder scanner. It can therefore be considered that myoma without cystic degeneration was recognized as residual urine.
In Case 2, the cause of falsely-elevated bladder scanner measurements was ascertained quickly, and a treatment plan was determined based on the previous case (Case 1).
Previous studies have shown that portable ultrasound bladder scanners are moderately sensitive, but less specific, for detecting urinary retention, showing a false-positive rate up to 9% [2]. The low specificity is probably because bladder scanners have difficulty differentiating between fluid collection in the pelvis and lower abdomen, and residual urine [2]. In other studies, lesions of cystic pathology in the abdomen and pelvis affected the bladder scanner results, and they were predominantly echo-free [3]. The bladder scanner falsely perceives the echogenicity to be similar to urine, leading to a false-positive PVR. In this study, it is notable that non-cystic uterine myomas resulted in false-positive elevated PVR on the bladder scanner. Since bladder scanning has a widespread use in assessing urine collection, bladder volume, and to avoid unnecessary catheterization, the possibility of false-positive PVR values must be kept in mind in clinical settings [9].
One study has proven that the BioCon-500 ultrasound machine used in this study shows good accuracy, with no significant difference in PVR measured between BioCon-500 and urinary catheterization [10]. However, in our study, the increasing urine volume was not proportional with the PVR volumes measured by the bladder scanner. As shown in Case 1 VCUG test results, when urine volume in the bladder is zero, the PVR volume measured by the bladder scanner was 222 mL, suggesting the possibility that uterine myoma was recognized as urine volume. In addition, after infusing 450 mL of radiocontrast agent to the bladder, 410 mL of urine was voided, but the bladder scanner measured 270 mL PVR volume. This indicates that the 270 mL myoma mass-related volume was measured in addition to 40 mL of real residual urine volume, and confirms the possibility that the 222 mL of the PVR volume measured when bladder urine volume was zero, was the myoma volume. However, after infusing 200 mL and 400 mL of radiocontrast agent, the PVR volumes measured by the ultrasound bladder scanner were 460 mL and 470 mL, respectively. This pattern indicates that as real urine volume increased, the myoma volume was ignored by the bladder scanner. In other words, we interpret the pattern that when residual urine volume in the bladder is small, myoma volume seemed to affect the volumes measured by the bladder scanner, but as the residual urine increased in volume, the impact of the myoma volume decreased. This led us to consider new characteristics of measurement error of bladder scanners, and further studies on this are considered necessary.
These two cases indicate the importance to note that myoma without cystic change can cause false-positives on bladder scanner measurements. We consider that bladder scanners calculate the urinary bladder volume based on true residual volume and additive effect of the mass with/without the cystic lesion, especially in lesser bladder volumes. In conclusion, a significant discrepancy between PVR measurement by a bladder scanner and urinary catheterization implies a possible abdominopelvic pathology, and further evaluation is recommended.
References
1. Park YH, Ku JH, Oh SJ. Accuracy of post-void residual urine volume measurement using a portable ultrasound bladder scanner with real-time pre-scan imaging. Neurourol Urodyn. 2011; 30:335–338. PMID: 20658544.

2. Cho KH, Song JH, Kim WB, Yang WJ, Song YS. Ovarian cystadenoma mistaken as postvoid residual urine by portable ultrasound scanning. J Korean Continence Soc. 2009; 13:166–168.

3. Alagiakrishnan K, Valpreda M. Ultrasound bladder scanner presents falsely elevated postvoid residual volumes. Can Fam Physician. 2009; 55:163–164. PMID: 19221075.
4. Al-Shaikh G, Larochelle A, Campbell CE, Schachter J, Baker K, Pascali D. Accuracy of bladder scanning in the assessment of postvoid residual volume. J Obstet Gynaecol Can. 2009; 31:526–532. PMID: 19646318.

5. Byun SS, Kim HH, Lee E, Paick JS, Kamg W, Oh SJ. Accuracy of bladder volume determinations by ultrasonography: are they accurate over entire bladder volume range? Urology. 2003; 62:656–660. PMID: 14550437.

6. Morrell GA. False reading of retained urine from a bladder scan. Urol Nurs. 2010; 30:147–148. PMID: 20469574.

7. Choe JH, Lee JY, Lee KS. Accuracy and precision of a new portable ultrasound scanner, the BME-150A, in residual urine volume measurement: a comparison with the BladderScan BVI 3000. Int Urogynecol J Pelvic Floor Dysfunct. 2007; 18:641–644. PMID: 17115233.

8. Alcazar JL, Pineda L, Martinez-Astorquiza Corral T, Orozco R, Utrilla-Layna J, Juez L, et al. Transvaginal/transrectal ultrasound for assessing myometrial invasion in endometrial cancer: a comparison of six different approaches. J Gynecol Oncol. 2015; 26:201–207. PMID: 26197857.

9. Palese A, Buchini S, Deroma L, Barbone F. The effectiveness of the ultrasound bladder scanner in reducing urinary tract infections: a meta-analysis. J Clin Nurs. 2010; 19:2970–2979. PMID: 21040003.

Fig. 1
Voiding cystourethrogram images after infusion of radiocontrast media in varying amounts. After infusion of 200 mL of radiocontrast media, the postvoid residual (PVR) volume measured by bladder scanner was 460 mL, and filing defects (arrow) to be estimated as myoma mass were observed (A). After infusion of 400 mL of radiocontrast media, the PVR volume measured by the bladder scanner was 470 mL, and no filing defect was observed as the bladder urine volume increased (B). After infusion of 450 mL of radiocontrast media, 410 mL of urine was voided, but the PVR volume measured by the bladder scanner was 270 mL (C).





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download