INTRODUCTION
The public expected that the introduction of vaccines would reduce the burden of coronavirus disease 2019 (COVID-19). However, breakthrough infections in fully vaccinated individuals are increasing globally.
12345 A faster decrease in protection against infection and severe disease by COVID-19 has been observed among fully vaccinated recipients.
5 In addition, acquired immunity through vaccination or natural infection is less protective against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) delta variant infection.
67
Psychiatric closed wards play an important role in supporting patients with mental illnesses. The influx of SARS-CoV-2 could cause extremely high attack rates; therefore, psychiatric wards may be more vulnerable to COVID-19.
8 Here, we report an outbreak of COVID-19 breakthrough infections that occurred among residents in a closed ward wherein most residents were fully vaccinated with the ChAdOx1 nCoV-19 vaccine from Oxford/AstraZeneca (ChAdOx1 nCoV-19).
METHODS
Study setting
On October 28, 2021, the Gyeongsangnam-do Rapid Response Team recognized COVID-19 outbreak that occurred in a closed psychiatric ward on the third floor of a five-story hospital. Before the outbreak, vaccinated healthcare workers (HCWs) underwent weekly nasal swab testing using reverse transcriptase polymerase chain reaction (RT-PCR) technique for SARS-CoV-2, while unvaccinated HCWs were tested at least once every 3 days. All patients were hospitalized after testing negative for SARS-CoV-2 and visitor restrictions were maintained in accordance with the national regulations. Epidemiological surveillance data from epidemic intelligence service officers were utilized to obtain demographic, vaccination history, and clinical data along with SARS-CoV-2 PCR test results. All patients with confirmed COVID-19 were isolated for at least 10 days. The remaining residents testing negative for SARS-CoV-2 were tested once every 3 days during quarantine. Prolonged hospitalization was defined as a case having an isolation period lasting more than 14 days.
Statistical analysis
Discrete data are presented as frequencies and percentages, and continuous variables are summarized as the mean ± standard deviation or the median and interquartile range according to the distribution. Characteristics were compared between subgroups of vaccinated residents and unvaccinated using the χ2 test, Fisher’s exact test, two-sample t-test, or Mann–Whitney U-test as appropriate. The proportion of patients in each arm with prolonged hospitalization within 90 days of vaccination, 90 days after vaccination, and unvaccinated groups were compared using one-way ANOVA. Variables with P < 0.05 in univariate analyses were candidates for multivariate analysis. All analyses were conducted using IBM SPSS Statistics for Windows, version 23.0 (IBM Corp, Armonk, NY, USA).
Ethics statement
The Samsung Changwon Hospital Institutional Review Board approved this study with an authorization agreement from Yekyung Hospital (SCMC 2022-01-009). Informed consent was waived due to the nature of public data.
RESULTS
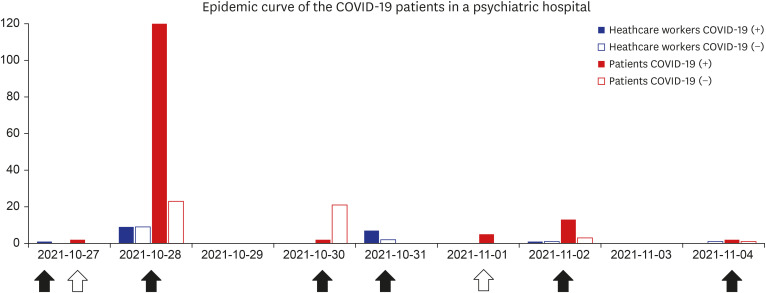
On October 27, 2021, one HCW tested positive during a weekly routine screening test for COVID-19. On the same day, two symptomatic patients were detected and tested positive based on RT-PCR. On October 28, all residents, including patients and HCWs, underwent RT-PCRs testing for SARS-CoV-2. SARS-CoV-2 spread rapidly throughout the ward in just 10 days, infecting 162 of 164 residents (
Fig. 1). One patient and one HCW (both of whom had received two doses of ChAdOx1 nCoV-19) were free of COVID-19 infection during the quarantine period. As of November 28, 2021, 17 (10.5%) patients showed prolonged hospitalization and two (1.2%) confirmed patients died.
Fig. 1
An epidemic curve of the COVID-19 patients in a psychiatric hospital. The solid arrows indicate routine testing of PCR, while the empty arrows indicate testing in symptomatic patients. The horizontal axis indicated the date on which the test was performed, while the vertical axis is the number of confirmed patients.
COVID-19 = coronavirus disease 2019.

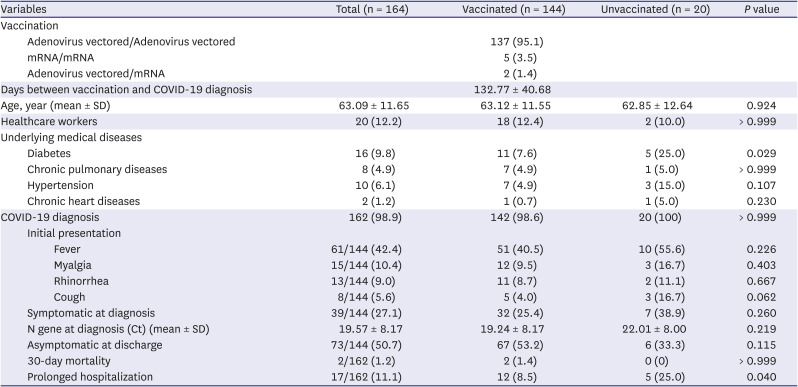
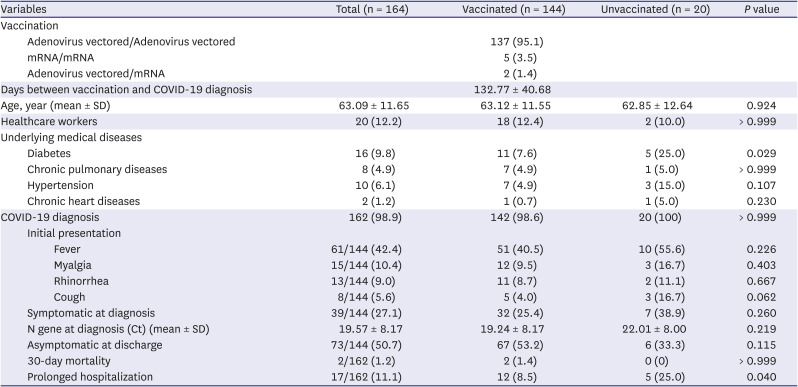
The characteristics of the vaccinated residents are described in
Table 1. A total of 144 (87.8%) residents received two doses of vaccines, of which 137 (95.1%) received two doses of the ChAdOx1 nCoV-19 vaccine. The mean interval between the second vaccination and COVID-19 diagnosis was 132.77 ± 40.68 days and the mean cycle threshold (Ct) for the gene encoding the nucleocapsid protein (N gene) was 19.57 ± 8.17. Prolonged hospitalization occurred in 17 patients (11.1%), and was more prevalent in the unvaccinated group than in the vaccinated group (25.0% vs. 8.5%,
P = 0.040). The symptoms and Ct value at diagnosis did not differ between the two groups.
Table 1
Characteristics of residents of a psychiatric hospital according to vaccination status
|
Variables |
Total (n = 164) |
Vaccinated (n = 144) |
Unvaccinated (n = 20) |
P value |
|
Vaccination |
|
|
|
|
|
Adenovirus vectored/Adenovirus vectored |
|
137 (95.1) |
|
|
|
mRNA/mRNA |
|
5 (3.5) |
|
|
|
Adenovirus vectored/mRNA |
|
2 (1.4) |
|
|
|
Days between vaccination and COVID-19 diagnosis |
|
132.77 ± 40.68 |
|
|
|
Age, year (mean ± SD) |
63.09 ± 11.65 |
63.12 ± 11.55 |
62.85 ± 12.64 |
0.924 |
|
Healthcare workers |
20 (12.2) |
18 (12.4) |
2 (10.0) |
> 0.999 |
|
Underlying medical diseases |
|
|
|
|
|
Diabetes |
16 (9.8) |
11 (7.6) |
5 (25.0) |
0.029 |
|
Chronic pulmonary diseases |
8 (4.9) |
7 (4.9) |
1 (5.0) |
> 0.999 |
|
Hypertension |
10 (6.1) |
7 (4.9) |
3 (15.0) |
0.107 |
|
Chronic heart diseases |
2 (1.2) |
1 (0.7) |
1 (5.0) |
0.230 |
|
COVID-19 diagnosis |
162 (98.9) |
142 (98.6) |
20 (100) |
> 0.999 |
|
Initial presentation |
|
|
|
|
|
|
Fever |
61/144 (42.4) |
51 (40.5) |
10 (55.6) |
0.226 |
|
|
Myalgia |
15/144 (10.4) |
12 (9.5) |
3 (16.7) |
0.403 |
|
|
Rhinorrhea |
13/144 (9.0) |
11 (8.7) |
2 (11.1) |
0.667 |
|
|
Cough |
8/144 (5.6) |
5 (4.0) |
3 (16.7) |
0.062 |
|
Symptomatic at diagnosis |
39/144 (27.1) |
32 (25.4) |
7 (38.9) |
0.260 |
|
N gene at diagnosis (Ct) (mean ± SD) |
19.57 ± 8.17 |
19.24 ± 8.17 |
22.01 ± 8.00 |
0.219 |
|
Asymptomatic at discharge |
73/144 (50.7) |
67 (53.2) |
6 (33.3) |
0.115 |
|
30-day mortality |
2/162 (1.2) |
2 (1.4) |
0 (0) |
> 0.999 |
|
Prolonged hospitalization |
17/162 (11.1) |
12 (8.5) |
5 (25.0) |
0.040 |

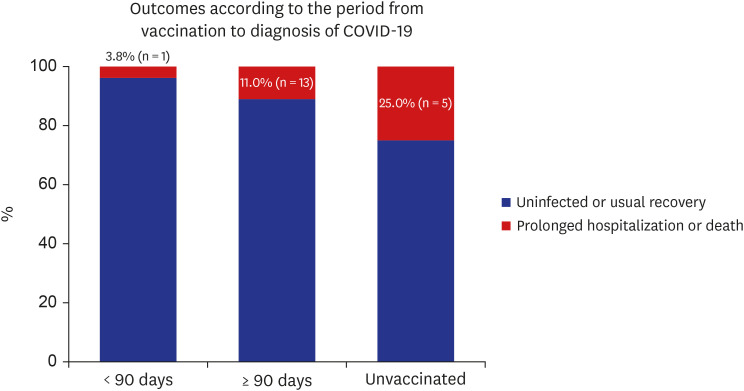
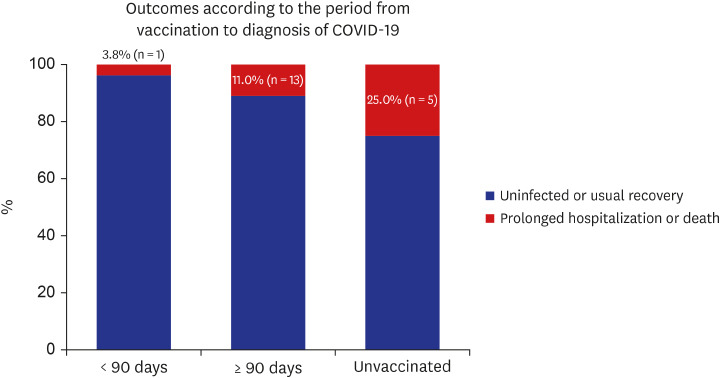
When divided into three groups (within 90 days of vaccination, 90 days after vaccination, and unvaccinated groups), there were 3.8% (1/26), 11.0% (13/118), and 25.0% (5/20) of prolonged hospitalization or death in each group (
P = 0.099) (
Fig. 2,
Supplementary Table 1).
Fig. 2
Outcomes according to the period from vaccination to COVID-19 diagnosis. The horizontal axis is the period from vaccination to diagnosis of COVID-19, while the vertical axis is the number of vaccinated residents (Total number = 164).
COVID-19 = coronavirus disease 2019.

DISCUSSION
This study describes an outbreak of COVID-19 breakthrough infections by SARS-CoV-2 in a psychiatric closed ward in a delta variant dominant setting. COVID-19 spread rapidly throughout the ward shortly after the index case detection, infecting 98.8% of the residents. Prolonged hospitalization was more prevalent in the unvaccinated group than in the vaccinated group. The case-fatality rate was lower than that in the previous outbreak when vaccines were not available.
8
A recent study investigated 197 breakthrough infections in 5,549 individuals who received a second dose of the ChAdOx1 vaccine and 3,205 who received a second dose of BNT162b2 vaccine.
5 The authors reported that after the second dose, individuals with anti-S levels < 500 U/mL were nearly twice as likely to develop a breakthrough infection as those with higher levels. The mean antibody levels declined to this threshold of 500 U/mL after approximately 3 months for the ChAdOx1 nCoV-19 vaccine and 7 months for the BNT162b2 vaccine.
5 Our results showed that most residents had received their second dose of ChAdOx1 vaccine 4 months prior to the breakthrough infection. Thus, most residents likely had low neutralizing antibody levels, which resulted in the rapid spread in the entire ward despite the high vaccination coverage rate. A Vietnamese study also reported 69 breakthrough infections associated with the SARS-CoV-2 delta variant among staff recipients of the ChAdOx1 in a 550-bed infectious disease hospital.
1 Infection occurred 7–8 weeks after most staff had received their second dose.
1
A UK study assessed vaccine-induced neutralizing antibody escape by the SARS-CoV-2 delta variant.
6 In the study, neutralizing antibody titers were 5.8 fold reduced against the SARS-CoV-2 delta variant relative to the wild-type (95% CI, 5.0–6.9).
6 Both old age and time, since the second dose of the BNT162b2 vaccine, were significantly correlated with decreased neutralizing antibody activity against the SARS-CoV-2 delta variant.
6 Our study results showed that a COVID-19 outbreak could occur if the SARS-CoV-2 delta variant was introduced into a psychiatric ward, with an average age of 63 years and an average duration of 133 days after the second dose of ChAdOx1 vaccine. The case-fatality ratio in this study was lower than that in the previous outbreak in a psychiatric closed ward (1.2% vs. 6.9%, Fisher’s exact test,
P = 0.030), however, the attack rate was similar (98.8% vs. 98.1%, Fisher’s exact test,
P = 0.643).
8 While vaccination reduced mortality, it was not sufficient to prevent an outbreak of the SARS-CoV-2 delta variant in the current psychiatric hospital setting.
Maintaining non-pharmaceutical interventions (NPIs) such as wearing mask, sanitizing hands, and social distancing is essential for reducing the COVID-19 burden despite differences in vaccination coverage rates.
9 Patients with mental illness have limited cognitive ability to comprehend rules and follow sterilization procedures.
10 Therefore, psychiatric hospitals may have difficulty in adhering to NPIs. Infection prevention and control is one of the mandatory areas of accreditation for psychiatric hospitals in Korea.
11 To receive accreditation, there should be an infection control committee and staff with appropriate continuing education. However, the requirements are not as strict as the infection control standards for general hospitals.
11 Crowded and shared spaces, inadequate supply of disinfection equipment, and no structural ventilating system contributed to previous outbreaks in psychiatric hospitals.
8 For preventing infections in closed psychiatric wards, our findings further suggest that the need to consider 1) a proper supply of personal protection equipment, 2) a contingency plan at each institution regarding an infection outbreak, 3) continuous surveillance and staff education, 4) appropriate non-psychiatric medical intervention, and 5) further vaccination plans for patients with reduced neutralizing antibody titers. In addition, every individual should be thoroughly classified with the consideration of the possibility of asymptomatic carriers while maintaining the restrictions on visitors.
The findings of the present study in the current epidemic highlight the potential for an outbreak of the SARS-CoV-2 delta variant in a psychiatric hospital even among fully vaccinated patients, whose protection against SARS-CoV-2 infection weakens more quickly. Owing to the characteristics of poor adherence to NPIs, patients with psychiatric disorders may have facilitated the transmission of the delta variant among vaccinated patients. These findings underscore the importance of NPIs in reducing the transmission of SARS-CoV-2 delta variant, even when vaccination rates are high. Furthermore, these results also suggested the importance of the third dose of COVID-19 vaccine,
12 considering the expected barrier for NPI adherence among patients in psychiatric hospitals.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download