INTRODUCTION
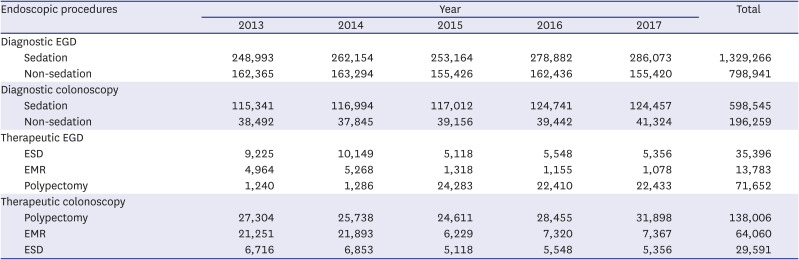
Esophagogastroduodenoscopy (EGD) and colonoscopy are relatively safe procedures, but can sometimes lead to serious, life-threatening complications. As the indications for therapeutic endoscopic procedures continue to expand, the risk for complications is expected to increase. Based on the Korean National Health Insurance Service database from 2002 to 2013, the overall colonoscopy volume increased eightfold over 12 years, and the colon polypectomy rate is also continuously increasing every year.
1 Based on the claims data of endoscopic submucosal dissection (ESD) for early gastric cancer in Korea between November 2011 and December 2014, although the number of gastric ESD trials increased every year, most of them were carried out in tertiary care hospitals in Korea.
2
As safety-related issues of endoscopy are closely related to the quality of endoscopists and endoscopy units,
3 many countries have emphasized and enhanced endoscopy quality management and have made efforts to improve quality at the national level. In the USA, the American Society for Gastrointestinal Endoscopy (ASGE)/American College of Gastroenterology (ACG) Task Force has been working to improve endoscopic quality with the establishment of the first set of quality indicators for gastrointestinal (GI) tract endoscopic procedures in 2006.
456 In Korea, the National Cancer Screening Program has included nationwide screening for gastric and colorectal cancer since 1999. The Korean Society of Gastrointestinal Endoscopy (KSGE) has established the National Endoscopy Quality Improvement Program to improve and manage the quality of endoscopic procedures. This program consists of qualification of endoscopists, quality improvement for instruments available at the endoscopy unit and endoscopic procedures, and measurement of outcomes of endoscopy screening.
789 Furthermore, KSGE implemented the Accredited Endoscopy Unit Program in 2012 to certify and encourage high-quality endoscopy practices.
10 Specifically, the Accredited Endoscopy Unit Program is obligated to document the incidence and types of complications, such as bleeding and perforation. Despite these efforts, quality control assessment programs still assess the documentation of endoscopic complications, but do not assess the actual incidence and management of complications.
Recently, ASGE/ACG has established a performance target associated with colonoscopy related to post-process quality indicators, which recommends that the perforation rate should be < 1/500 overall and < 1/1,000 in screening. It also recommends a bleeding rate < 1% after polypectomy.
11 However, there have been few studies on complications related to diagnostic and therapeutic EGD and colonoscopy in Korea, with neither a uniform definition nor standardized reporting system, so there seems to be discrepancies between real clinical practice and research results. Nonetheless, the accredited Endoscopic Unit Program’s assessment of high-quality endoscopic practices has a mandatory requirement for documentation of complication rates, which is expected to better reflect data from real practices.
This study assessed the current status of complications associated with diagnostic and therapeutic endoscopy in Korea, to utilize this information to develop safety management indicators and improve quality of care in the endoscopy unit in Korea.
Go to :

DISCUSSION
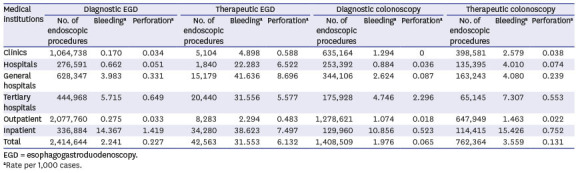
Safety is one of the most important issues in quality management of endoscopy. However, the status of complications related to endoscopy is not well known. This is the first study in Korea to simultaneously analyze population-based data through insurance claims accounting for about 98% of the population and real-world data from 50 institutions certified by KSGE for high-quality endoscopic practices. The HIRA claims data were intended to be used to analyze the overall incidence of complications that occurred over a certain period for all volumes of hospitals in Korea and to analyze the incidence of complications according to the volume of the hospitals. The 50-hospital survey data were collected by tertiary or general hospitals that had performed certain procedures, such as gastric or colonic ESD, and had been certified by the Accredited Endoscopy Unit Program reviewed by KSGE for high-quality endoscopy practices.
Bleeding is a complication that occurs rarely in diagnostic EGD and is primarily associated with mechanical irritation generated by the tip of the endoscope during passage. The incidence of bleeding is approximately 0.15%.
15 The risk for bleeding is higher in patients who have previously undergone gastrectomy and after multiple cold biopsies (8–15 biopsies) of the anastomotic site in Billroth I and Billroth II patients.
16 A Mallory-Weiss tear may also occur due to excessive belching or retching during EGD.
17 The incidences of bleeding associated with therapeutic EGD are 4% after EMR and 4.5% after ESD.
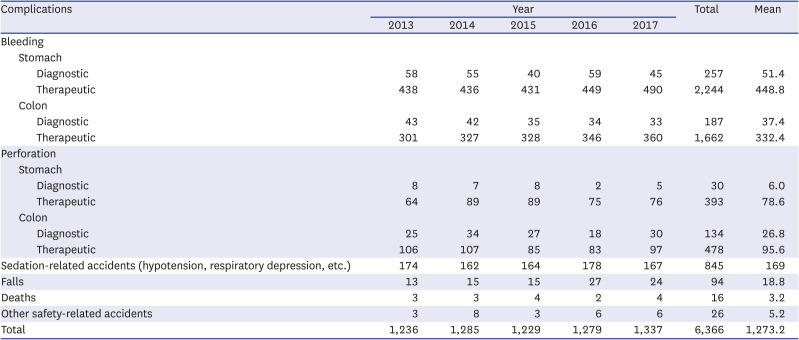
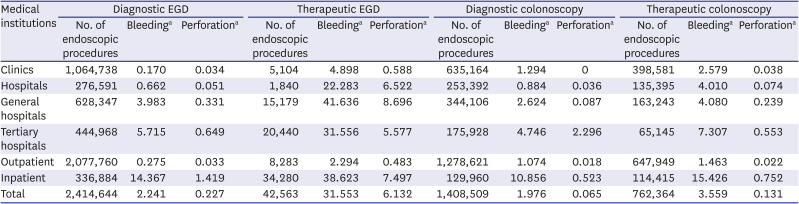
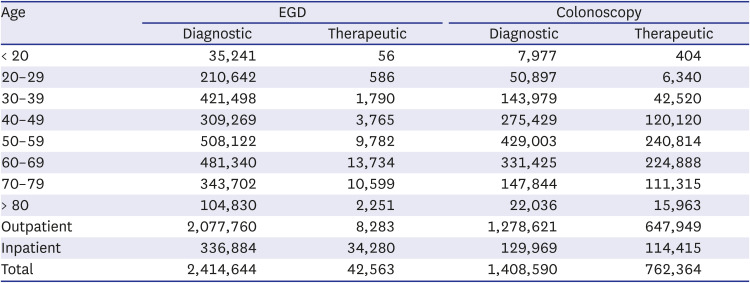
18 In this study, the incidences of bleeding associated with diagnostic and therapeutic EGD were 0.224% and 3.155% in the 2017 HIRA claims data, and 0.012% and 1.857% in the 50 hospitals surveyed, respectively. Diagnostic and therapeutic EGD procedures were performed most frequently in clinics and tertiary hospitals, and the rates of bleeding associated with both procedures were relatively low compared to previous studies. The complications associated with EGD tended to increase as the hospital volume increased, probably due to the larger number of high-risk patients or higher rate of difficult procedures in general or tertiary hospitals.
Bleeding after polypectomy is one of the most common complications associated with colonoscopy. A recent meta-analysis showed that the incidence of bleeding in diagnostic colonoscopy without polypectomy was 0.06%, with rates of 0.98% after polypectomy,
19 0.82% for immediate bleeding after colorectal ESD, and 1.7% for delayed bleeding.
19 Another meta-analysis of the risk factors for bleeding associated with polypectomy showed that factors such as old age, high blood pressure, cardiovascular disease, right colon position, and polyp size > 1 cm were significantly associated with the occurrence of bleeding after polypectomy.
20 In this study, the incidences of bleeding associated with diagnostic and therapeutic colonoscopy were 0.198% and 0.356% in the 2017 HIRA claims data, and 0.024% and 0.717% in the 50 hospitals surveyed, respectively. Both diagnostic and therapeutic colonoscopy procedures were most frequently performed in clinics. Similar to EGD-related bleeding, the diagnostic and therapeutic bleeding rates related to colonoscopy were relatively low compared to previous studies and tended to increase as the hospital volume increased, which was also probably due to the larger numbers of high-risk patients, such as those taking anticoagulant or antiplatelet drugs and with comorbidities, and the higher rate of difficult procedures, such as polypectomy for difficult location and large polyps, in general or tertiary hospitals.
Perforation during diagnostic EGD is extremely rare. A large prospective study reported that the incidence of perforation in diagnostic EGD was 0.05% and the associated mortality rate was 0.008%.
21 The risk for perforation during diagnostic EGD was reported to be associated with Zenker’s diverticulum, esophageal stenosis, malignant tumors, duodenal diverticulitis, and the experience level of the endoscopist.
2122 Esophageal perforation can also occur during therapeutic procedures, such as balloon dilation with esophageal stenosis or achalasia and removal of sharp foreign bodies.
22 In a meta-analysis, the incidences of esophageal perforation were 1.3% and 4.0% for EMR and ESD, respectively,
23 and those for stomach perforation were 1.2% and 3.2%.
23 In this study, the incidence rates of perforation associated with diagnostic and therapeutic EGD were 0.023% and 0.613% in the 2017 HIRA claims data, and 0.001% and 0.325% in the 50 hospitals surveyed. The incidences of diagnostic and therapeutic perforation associated with EGD were relatively low compared to previous studies, and the incidence of perforation in therapeutic EGD was lower in tertiary hospitals than in general hospitals.
The incidence of perforation associated with diagnostic colonoscopy was reported to be 0.05% with a mortality rate of 0.0029%, and that of perforation after colorectal polypectomy was 0.08% in a previous meta-analysis.
19 The incidences of perforation related to colorectal ESD were reported to be 4.2% for immediate perforation and 0.22% for delayed perforation.
24 During therapeutic colonoscopy, polyp location in the right colon or cecum, lateral spreading or nonpolypoid morphology, non-lifting polyp after submucosal injection due to submucosal fibrosis or deep layer involvement, polyps > 1 cm in size, and multiple polyps are risk factors for perforation.
25262728 Diagnostic colonoscopy-associated perforations are relatively large and have a greater likelihood of requiring surgery than therapeutic colonoscopy-associated perforations.
29 In this study, the incidences of perforation associated with diagnostic and therapeutic colonoscopy were 0.007% and 0.013% in the 2017 HIRA claims data, and 0.017% and 0.206% in the 50 hospitals surveyed, respectively. The incidences of diagnostic and therapeutic perforation associated with colonoscopy were also relatively low compared to previous studies and increased as the hospital volume increased, probably because most cases where perforation occurred in the clinic were transferred to tertiary hospitals for endoscopic management or surgery, and therefore the number of perforations in tertiary hospitals might be overestimated in analyses of HIRA data. The complication rates were higher in hospital survey data than HIRA claim data. This was because the hospital survey data were collected by general or tertiary hospitals that performed more in the way of high-level or high-risk procedures, hospital survey data included complications related to colorectal ESD, and a significant number of procedures might have been performed by GI fellows undergoing training. Also, because the occurrence of complications must be recorded to be certified by the Accredited Endoscopy Unit Program, it was likely that the hospital survey data reflected the occurrence of complications more accurately than the HIRA claim data.
This study had some limitations. We could not completely exclude cases who underwent therapeutic endoscopy due to bleeding rather than as an endoscopy-related complication due to limitations of use of claim data.
It might be impossible to define perforation accurately as a claim code because the clinical course of perforation differs among individuals, from conservative healing to endoscopic treatment to surgery, and coding for complications differs depending on the endoscopist or hospital. The amount of data was very large; therefore, we could not accurately evaluate the causal relationships, because we could not analyze the individual circumstances of each case. In the case of 2017 HIRA claims data, there were limitations with regard to the possible occurrence of complication code entry errors and unclaimed items after a complication had occurred. In the case of survey data, there were limitations with regard to the possible occurrence of missing records or varying definitions of a complication between institutions. Moreover, the investigation and recording of endoscopy-related complications may have been avoided in many cases because of the fear of legal issues arising with the reporting of complications. Thus, many cases of endoscopy-related complications may have been missing from the records.
Analyzing the results of this study, the largest numbers of diagnostic and therapeutic endoscopy procedures were performed in clinics, and the rate of complications was almost negligible. These results may be mistakenly taken to indicate the high degree of safety of endoscopy in clinics. The statistics in this study were not interpreted as absolute numbers because large numbers of complications in clinics were counted as occurring in general or tertiary hospitals because the patients were transferred to these hospitals for treatment and claims were made there. In addition, most procedures performed in clinics were simple, while tertiary hospitals had higher rates of more technically difficult procedures, which could lead to higher rates of complications. These factors may diminish the reliability of statistical analyses, and we cannot exclude the possible occurrence of large statistical errors in this study.
However, despite these limitations, the present study makes a significant contribution, as it is one of very few large-scale studies in Korea to investigate the incidence of endoscopy-related complications using data from HIRA claims and surveys over 5 years in 50 hospitals. Future research should consider various factors, such as diagnostic and therapeutic endoscopy indications, comorbidities, antithrombotic drug use, and experience of endoscopists related to complications according to the type of endoscopic procedure.
In conclusion, the incidences of diagnostic and therapeutic complications associated with EGD or colonoscopy tended to increase with the hospital volume in Korea. To obtain more reliable statistics, a system is needed to effectively report and manage complications at all types of hospital, from clinics to tertiary hospitals, in Korea.
Key message: 1) Diagnostic EGD was performed most often in clinics, while therapeutic EGD (EMR or ESD) was performed most often in tertiary hospitals in Korea. 2) Diagnostic colonoscopy and therapeutic colonoscopy (polypectomy, EMR, or ESD) were performed most often in clinics. 3) The incidences of complications associated with diagnostic and therapeutic EGD, or colonoscopy tended to increase with the hospital volume.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download