INTRODUCTION
With an increase in the life expectancy for spinal cord injury (SCI) groups, interest in quality of life is also rising [
1]. The ultimate goal of rehabilitation is achievement of an independent and healthy life. Promoting physical activity is assumed to reduce secondary impairment and chronic health problems, and it is also helpful for the psychological well-being [
2]. Participation in sports activities means success of community-based rehabilitation, and this may help in the reduction of social cost such as medical care and loss of productivity [
3].
Although there are expectations of several benefits, persons having SCI face many barriers to participate in physical activity. Loss of complex body functions, such as motor and sensory functions, autonomic regulations, bladder and bowel control, circulatory regulation and skin protection, restrict their sports participation [
4]. Besides, there are systemic and environmental barriers such as accessibility, financial cost and information [
5]. In Korea, environmental barriers such as lack of information and poor accessibility for the disabled add to the difficulties.
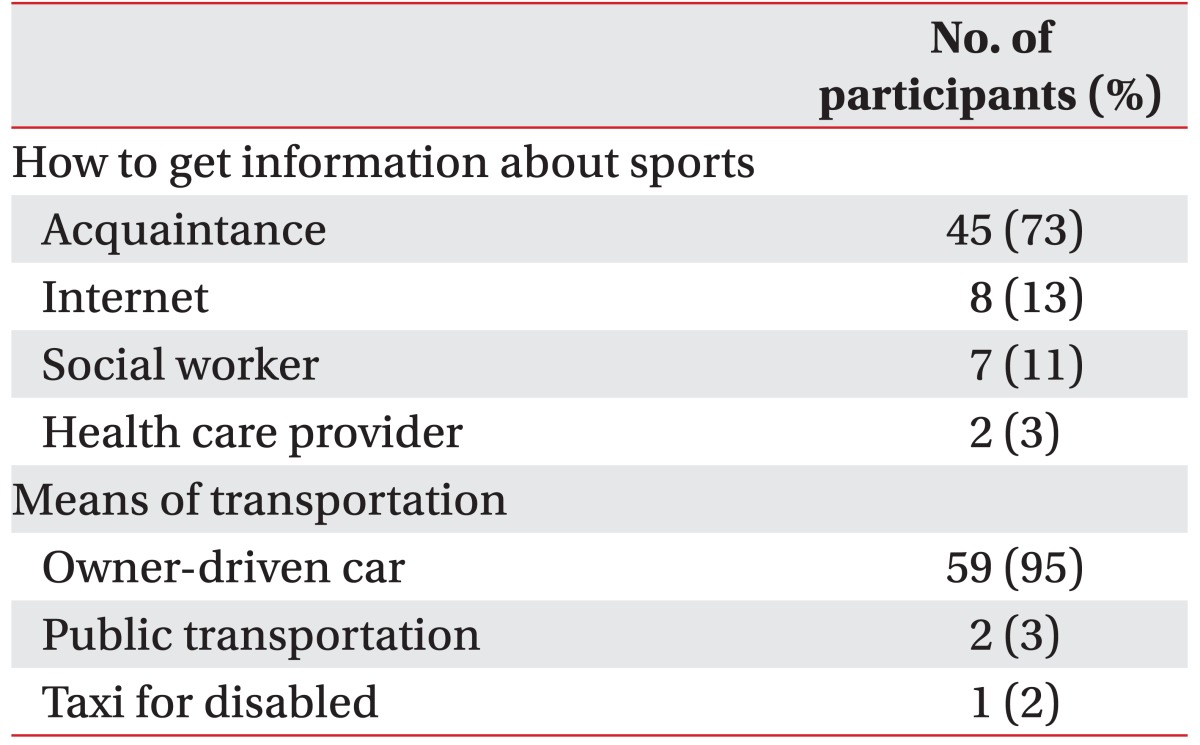
According to the results of research on needs of people with SCI in Korea 2012, over 50% of respondents answered their willingness to use disability welfare facilities and disability gyms. Nearly 70% of respondents used private automobiles and about 30% of respondents got welfare service information from fellow people with SCI, as their primary methods of transportation [
6]. Also, according to a 2015 survey on the participation of the disabled in physical activity in South Korea, only 4.3% of respondents used facilities for the disabled, and approximately half of the respondents (47%) used a nearby park. This meant that systemic and environmental support level was lower than the needs.
In Korea, as part of an effort to enhance sports participation, we tried to identify barriers at the individual and the societal level for persons with SCI. We assessed functioning and disability in persons with SCI who are physically active, as per the International Classification of Functioning, Disability and Health (ICF) Core Set for SCI for long-term care [
7].
MATERIALS AND METHODS
Subjects
This study involved questionnaire surveys of 62 community-dwelling SCI athletes participating in sports activities. We visited sports clubs and distributed the questionnaire through a structured interview process that typically lasted 30 minutes. To be included in the interview, following criteria were required in the SCI patients: (1) living in a South Korean community, (2) having adequate communication function, and (3) regularly participating in sports activities at sports club for disabled. All participants provided their formal consent. The study was approved by the local Institutional Review Board and was carried out in accordance with the Declaration of Helsinki.
Instrument development and measure
We conducted qualitative interviews with 15 SCI persons regarding their sports activity experience after affliction with SCI, based on comprehensive ICF Core Set. The participants were asked to freely describe any limitations in participation. The presence of the barriers was noted for each of the following categories: 'Body functions', 'Body structures', 'Activity and participation', and 'Environmental factors'. The dichotomous scale was used to indicate the presence or absence of a problem. The interview was conducted, and the data were analyzed by two physiatrists. We selected categories frequently answered in sample interviews for 'Body functions', and a questionnaire was made about specific problems using sublevel categories of each issue. For example, the category b735 'muscle tone functions' was assessed using additional question such as "Which body structures are the common barriers with muscle tone functions?". Responders were allowed to choose multiple answers in each question regarding sports activity, except for demographic purposes.
For the questionnaire on 'Body functions and structures', we referred to 7 chapters and 32 second level ICF categories regarding the core set of barriers. We also investigated the unmet medical care problems. In sample interviews, problems frequently answered were pain, urination, defecation, muscle tone, mobility of joint, and skin protection. Our questionnaire asked to identify the specific structures or functions about these problems using third or fourth level ICF categories.
In 'Activity and participation components', the questionnaire was made using 9 chapters and 39 second level ICF categories. Sample interviews revealed a high prevalence with respect to mobility and self care.
In 'Environmental factors', the questionnaire was comprised from 5 chapters and 41 second level ICF categories. The sources of information such as type of sports and how to join the team were addressed. We also questioned the means of transportation used to get to sports clubs.
Statistical analysis
All analyses were performed using SPSS ver. 21.0 for Windows (IBM, Armonk, NY, USA). Data analysis included the use of descriptive statistics to examine the frequency and magnitude of reported barriers. All surveys were done in personal interview. There was no missing data.
DISCUSSION
In America or Europe, many studies have reported barriers of sports participation in people with SCI [
89]. These studies were reported in developed countries [
10], where there may be cultural differences and thus might not be relevant for the Korean environment. Compared to other concerns with SCI groups, studies related to sports participation with SCI patients are relatively limited in South Korea. Based on our best knowledge, there have been some studies that assessed effects of sports participation, such as quality of life or disability acceptance [
1112]. But suggestions on how to promote sports participation was lacking.
In our studies, we obtained a more comprehensive understanding of the current issues of sports participation with SCI athletes in South Korea, by using the ICF Core Set for SCI for long-term care; we presented the data suitable for the current situation in South Korea. Previous studies have been very diverse in terms of study outcomes and data reporting. Comparing other health status measures, the ICF as a part of the World Health Organization's international family of classifications, is a contemporary framework to harmonize the assessment of functioning and disability at the individual and the societal level. Also, there has been confusion on the definition of participation; many health literatures have used varied terms such as participation, social participation and community participation. The ICF domains of 'Activity and participation' considered to clarify these definitions of social and community participation are 'Interpersonal interactions and relationships', 'Major life areas', and 'Community, social, and civic life' [
13]. However, sports are only a part of the broader definition of physical activity or community participation. They can be defined in many ways, from social connectedness with other individuals to intensive sports activity. Therefore, we focused more on sports participation, including community-dwelling SCI athletes groups.
The frequently addressed impairments in component 'Body functions' were movement related functions, bladder and bowel functions, pain sense and pressure ulcer. These problems are well-known complication of SCI and supported by previous studies [
14].
Movement related functions such as muscle power and tone function, are important factors for sports performance. Most SCI persons answered the major issues were muscle strengthening rather than motor recovery. They also thought the muscle tone functions such as control of spasticity were important factors in participating for sports activity. Regarding muscle tone and joint mobility dysfunctions, problems of the lower extremity were frequently addressed. The change of skeletal muscle fiber types in SCI can affect aerobic capacity [
15], but in this study, few respondents checked 'b455 exercise tolerance functions'. These findings may be related to the higher number of people with paraplegia and a fewer with tetraplegia in this study.
Bladder and bowel dysfunctions were reported to be common problems. We identified these problems with third level ICF categories. Lack of bladder and bowel autonomy was more addressed than incontinence. These problems are associated with low levels of physical quality of life domains and high mortality [
16]. Several studies reported an increasing prevalence of cardiovascular and thermoregulatory problems with time after SCI [
1718]. Some quadriplegia participants reported being challenged by managing this problem during sports activities. These problems were not highly checked, because almost all participants were paraplegics in this study.
Skin problems were frequently mentioned by the participants. Prevalence of pressure sore for persons with chronic SCI varied between 15% and 30% [
19].
In our study, about 70% of responders reported experiencing pressure sore since sports participation. This finding may be related to direct soft tissue trauma of lower extremity and longer duration of wheelchair seating time during sports activities.
The participants needed maximum medical care for 'urination functions' (b620) and 'sensation of pain' (b280). These findings showed discrepancy between barrier factors and needs for care, when related with sports participation. Most of the SCI responders were on medication for the management of bladder, bowel, pain and spasticity issues. However, they still had unmet problems such as urinary incontinence and musculoskeletal pain. We also addressed the 'sensation of pain' (b280) with fourth level categories. Frequently addressed body structures were upper limb, lower limb and back. Taylor and Williams [
20] reported the prevalence of sports related injury among the wheelchair racing athletes was 72% during a 12-month period, with upper extremity injuries being the maximum. Our study did not cover the reason of pain or mechanism of injury; overuse injuries have also been identified as important mechanisms. For preventing sports injuries, injury risk factors and mechanisms could be established. Along with preventive strategies, training programs should be provided with medical support. Physicians should be aware of this need and consider a specialized care related with activity and participation during the treatment of SCI.
The most often mentioned barriers of activity and participation were 'mobility' (d4) and 'self care' (d5). Regarding mobility issues, maintaining and changing body positions, transfer and hand and arm use were frequently reported problems. In dynamic situations like sport activities, balance and stabilization capability are major concern. For preparing sports participation, balance and hand use training under dynamic stress should be considered during rehabilitation therapy [
21].
A large number of 'Environmental factors' were included in the comprehensive ICF Core Set. 'Environmental factors' are important for assessing problems and planning the transition from hospital to the community in people with SCI. The frequently addressed barriers were sports facilities, financial cost, transportation problems and lack of information.
Limited sports facility was one of the problems. There are few sports club for disabled in Korea, and accessibility to public fitness facilities is limited because of barriers such as lack of ramp, stairs, narrow doorway, narrow toilet and inaccessible shower rooms. In case of team sports, finding inexpensive accommodation having a facility for the disabled and situated near the stadium is difficult during the competition season.
Exercise cost was identified frequently as barrier and facilitator. Purchasing and repairing wheelchair for sports is expensive, and there is not enough funding to support disabled sports activity. Using public transportation to get to exercise facilities is hard, therefore having own car is absolutely essential to access facilities and to carry sports equipment. Almost all of our participants had their own car and sports equipment, which they mentioned as a facilitator. But for overall disabled groups, economic issues could be a barrier to engage in physical activity. Public transportation with reasonable wheelchair lift, accessible doors and curbs should be considered in a public health policy especially in the developing countries. Improving accessibility to sports facilities will encourage individuals with SCI to engage in community programs.
According to a survey on physical activity of people with disability in Korea, over half the respondents reported they needed professional support for sports activity, and around 20% of respondents had help from professional physical coach at the public sports facility [
22]. There are few specialized supports for disability sport in Korea. In some advanced countries, there are national organizations to provide individualized information and develop guidelines about disability sports, such as Active Living Alliance for Canadians with a Disability, and the National Center on Health, Physical Activity and Disability of America. They also refer people with disability to community transformation programs through a network.
Although there is a lack of professional support, the relationship with peer, family and friends were reported as a facilitator. One purpose of participating in sports was to make social contacts. Several SCI participants relied on interacting with their peers with disabilities. They also got the information from the peers about accessible facilities, sports skills and even managing medical problems such as overuse injury. Before returning to the community, SCI patients have to be supported to find the type of sports they could enjoy. As a part of health and social services, community based rehabilitation programs have to provide information, financial support and health counseling about sports activities. Health professionals have to consider how to promote the physical activity of SCI patients, and inform them where and how to exercise.
This study had some limitations. First, the study was conducted on SCI athletes in sports clubs such as basketball, lawn bowling and rugby team. The findings may not be generalized to all types of sports activity. Our participants are likely to be physically more active and in higher level of economic status among disabled groups. Second, the subjects were small in number. Besides, almost all subjects were paraplegics. There might be limitations in applying our research findings to all SCI patients. Third, the ICF was applied in a restricted way in this study. Respondents answered the questions in dichotomous scale indicating only the presence or absence of a problem, instead of in a five step scale. Fourth, although we did not evaluate the personal factor separately, we thought these included the body function categories such as health problem, lack of energy and fatigue. However, regarding pre-injury exercise experiences, some participants addressed this issue as a facilitator. This is known as one of predictor active post-injury sports participation. We could not link that to appropriate ICF categories of the Core Set.
We explored the experiences of athletes with SCI in South Korea with respect to dilemmas of sports participation, especially regarding the facilitators and barriers to sports participations using the ICF Core Set. The results showed that the ICF language in general covers a broad range of the individual experiences of persons with SCI. Identified function, disability and environmental issues showed some differences compared with common problems with SCI. Thus, we suggest considering in making an ICF Core Set for specific participation such as sports activity. Rehabilitation professionals can use this core set as a guideline to meet the needs of individuals with SCI. Also, it will be useful to promote community integration for SCI through a multidisciplinary approach.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download