Abstract
Objective
To examine the relation between the presence of penetration or aspiration and the occurrence of the clinical indicators of dysphagia. The presence of penetration or aspiration is closely related to the clinical indicators of dysphagia. It is essential to understand these relationships in order to implement proper diagnosis and treatment of dysphagia.
Methods
Fifty-eight poststroke survivors were divided into two groups: patients with or without penetration or aspiration. Medical records and videofluoroscopic swallowing examinations were reviewed. The occurrence of clinical indicators of dysphagia between two groups was analyzed with Cross Tabulation and the Pearson chi-square test (p<0.05).
Results
Poststroke survivors with penetration or aspiration had significantly high occurrences of delayed initiation of the swallow (p=0.04) and reduced hyolaryngeal elevation (p<0.01) than those without penetration or aspiration.
Conclusion
The results of this study indicate that delayed initiation of the swallow is a strong physiological indicator of penetration or aspiration during the oral stage of swallowing in poststroke survivors. For the pharyngeal stage of swallowing, hyoid and laryngeal elevation is a key event related to occurrence of penetration or aspiration. Clinical indicators should be investigated further to allow appropriate implementation of treatment strategies for stroke survivors.
Dysphagia is a disorder of swallowing. In adults, it usually involves structural damage to the oropharynx or damage to the neuro-pathways, both of which affect oropharyngeal swallowing functions. Stroke and neurological diseases are common causes of dysphagia between the oral cavity and the lower esophageal sphincter. Between 30% and 50% of individuals who had a stroke have swallowing problems [12]. Dysphagia resulting from a stroke is considered to be a major cause of medical complications such as aspiration pneumonia, dehydration, and malnutrition. Even though a degree of aspiration may occur in normal healthy adults without medical complications [3], aspiration in poststroke survivors can lead to serious medical consequences such as bacterial pneumonia, chemical pneumonitis, or death [4]. With this in mind, it is essential to find ways to prevent and treat aspiration in stroke survivors.
After a stroke, survivors go through a series of clinical and videofluoroscopic examinations of swallowing. At the beginning of evaluation, the clinician's main concern is the presence of aspiration or penetration. Aspiration is defined as the passing of the bolus below the true vocal folds, and penetration is when the bolus enters the airway but not below the true vocal folds. In addition, the clinical indicators of oropharyngeal dysphagia are observed in order to figure out the source of dysphagia. According to the available literature, several physiological indicators were reported as being related to the occurrence of aspiration and penetration. Researchers [5678] have demonstrated that delayed initiation of the pharyngeal swallow is an important indicator of aspiration in stroke survivors. Aspiration also has been associated with incomplete laryngeal closure as well as reduced hyoid and laryngeal excursion [9]. Laryngeal closure involves approximation of the arytenoid cartilages and the epiglottis to protect the airway. Reduced hyoid excursion has been reported to be an independent indicator of aspiration. Hyoid and laryngeal excursion leads to vertical and anterior displacement of the hyoid bone during the pharyngeal swallow. As the bolus passes into the pharynx, the tongue base, on which the hyoid bone rests, pulls the hyoid bone and larynx vertically and anteriorly. It contributes to airway protection by making the epiglottis cartilage descend over the top of the larynx, and pulling the upper esophageal sphincter (UES) to allow the bolus to be directed toward the esophagus [10]. Perlman et al. [11] reported that, out of 330 dysphagic patients with various neurogenic disorders, 22% were observed to have reduced hyoid excursion, which was significantly associated with epiglottic immobility and subsequent penetration and aspiration.
It is necessary to investigate the relation between the presence of penetration or aspiration and the clinical indicators of dysphagia. Understanding of this relationship is essential for clinicians to implement proper diagnosis and treatment of dysphagia. The purpose of this study was to examine the relation between the presence of penetration or aspiration and the occurrence of the clinical indicators in dysphagia. The clinical indicators were classified based on the stages of swallowing. The occurrence of clinical indicators among stroke survivors with and without penetration or aspiration will be compared. The findings of this study will provide clinicians and patients with information useful in understanding the characteristics of dysphagia in poststroke survivors.
This was a retrospective study that reviewed medical records and the results of a fluoroscopic swallowing study for stroke survivors who were referred for swallowing evaluation between July 1, 2010 and June 30, 2011. This study was approved by the Institutional Review Board of Hallym University Medical Center, Chuncheon, South Korea. Among 136 patients who were referred to the fluoroscopic swallowing study, 58 stroke survivors were included. Exclusion criteria of subjects were as follows: 1) insufficient medical records, 2) previous history of a stroke, and 3) incomplete fluoroscopic swallowing study.
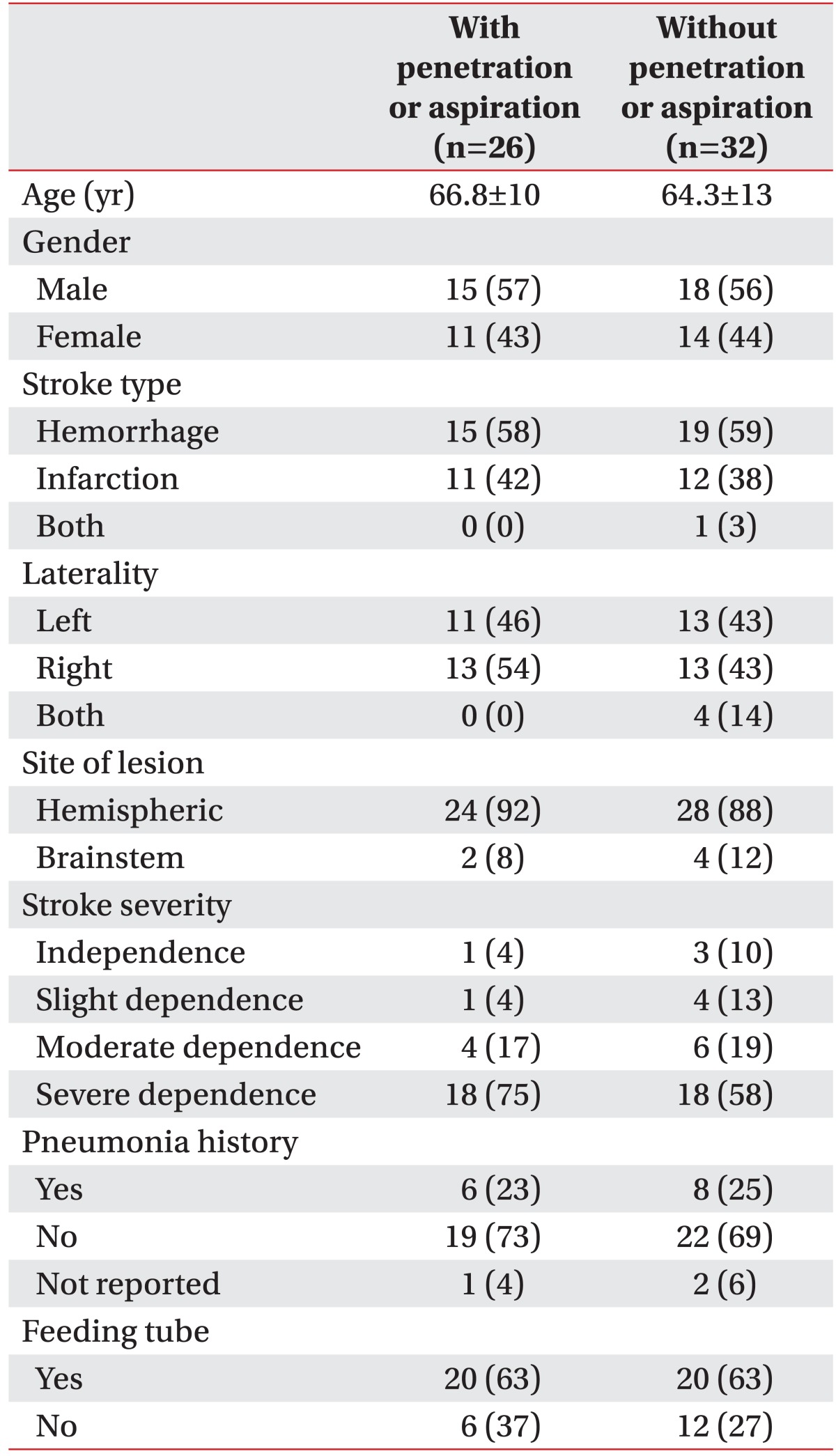
Stroke survivors were divided into two groups according to the presence of penetration or aspiration: stroke survivors with penetration or aspiration and stroke survivors without penetration or aspiration. Each patient's medical record was assessed according to five categories: demographic items (i.e., age and gender), stroke information (i.e., type, laterality, and site of lesion, and stroke severity using Barthel scale), pneumonia history, and feeding tube status. Table 1 presents demographic and clinical information for the 58 stroke survivors.
From the analysis of fluoroscopic swallowing studies on 58 stroke survivors, the clinical indicators of dysphagia were analyzed based on swallowing stages. In the oral stage, poor lip closure, poor oral control of bolus, delayed initiation of the swallow, and oral residue were observed. Delayed initiation of the swallow was classified at the oral stage because the triggering point of the pharyngeal swallow is the anterior faucial pillar in the oral cavity [12]. In fluoroscopic swallowing studies, delayed initiation of the swallow was defined as when the bolus reaches the vallecula but hyolaryngeal elevation is not triggered [13].
In the pharyngeal stage, penetration or aspiration was observed at first to classify subjects into two groups. Patients that presented with penetration or aspiration with any consistency at least once were classified as stroke survivors with penetration or aspiration. In addition, vallecular residue, pyriform sinus residue, and reduced hyolaryngeal elevation were recorded. During swallowing in the fluoroscopic swallowing study, reduced hyolaryngeal elevation was defined according to absence or reduction of elevation of the hyoid and larynx.
Two experienced physicians performed and analyzed the fluoroscopic swallowing study on site. Together they recorded the presence and absence of penetration or aspiration, as well as the clinical indicators for each swallow. The first physician had more than three years of experience in swallowing assessment and treatment. The second physician was a supervisor and had more than five years of experience. Both participated in swallowing assessment training regularly and performed fluoroscopic swallowing evaluation weekly for at least 5 patients with various etiologies.
Interpretation of the fluoroscopic swallowing studies was made on site by the two clinicians together. Our hospital has the capacity to record swallowing studies with 7 frames per second. During the analysis, if there was a discrepancy, they reviewed the fluoroscopic swallowing study together and reached agreement in interpretation. The clinical indicators of oropharyngeal dysphagia were selected based on the hospital's standard fluoroscopic swallowing study protocol.
Stroke survivors were classified into two groups by the presence of penetration or aspiration. Cross Tabulation and the Pearson chi-square test were used to analyze the occurrences of physiological indicators of oropharyngeal dysphagia between the two groups with a significance level of p<0.05.
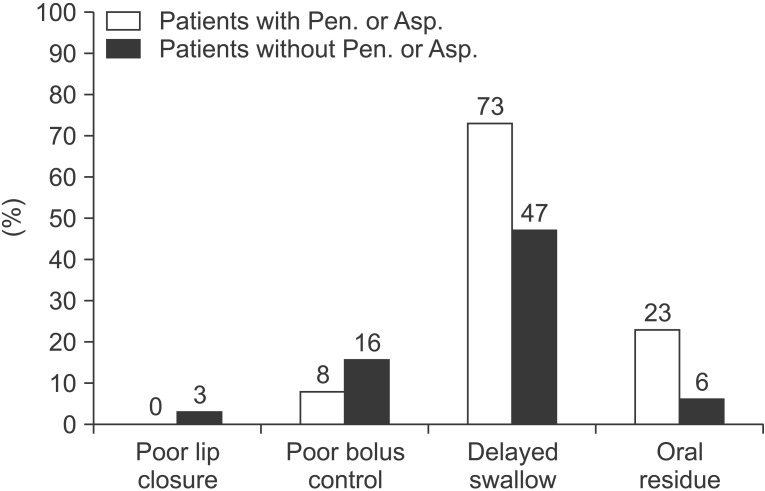
In the oral stage, there was no significant difference in the occurrence of lip closure, bolus control, and oral residue between the two groups. However, delayed initiation of the swallow was observed significantly more in stroke survivors with penetration or aspiration (p=0.04). For the stroke survivors with penetration or aspiration, 73% showed delayed initiation of the swallow, but for the stroke survivors without penetration or aspiration, just 47% showed delayed initiation of the swallow (see Fig. 1). This finding indicated that stroke survivors with penetration or aspiration initiated the swallowing response more slowly (i.e., delayed initiation of the swallow) when the bolus entered the pharynx during the oral stage of swallowing than those without penetration or aspiration.
In the pharyngeal stage, there was no significant difference in the occurrence of vallecular and pyriform sinus residues between the two groups. However, stroke survivors with penetration or aspiration showed reduced hyolaryngeal elevation when compared with those without penetration or aspiration (p<0.01). Among stroke survivors with penetration or aspiration, 88% showed reduced hyolaryngeal elevation, but for stroke survivors without penetration or aspiration, only 37% showed reduced hyolaryngeal elevation. This result indicates that stroke survivors with penetration or aspiration tend to have less airway protection or a reduced UES opening during the pharyngeal swallow (Fig. 2).
This study divided poststroke survivors into two groups according to the presence of penetration or aspiration. These two groups of stroke survivors were compared based on the occurrences of clinical indicators of dysphagia using videofluoroscopic examination of swallowing. The findings of the study showed that poststroke survivors with penetration or aspiration had significantly more occurrences of delayed initiation of the swallow and reduced hyolaryngeal elevation than those without penetration or aspiration.
Poststroke survivors showed reduced range and speed of oral and pharyngeal muscles. This may be because the swallowing of these survivors is weak due to impaired firing of muscle fibers caused by poststroke damage to neural (sensorimotor) pathways above the brainstem. It was shown that more than 30% of poststroke survivors showed weak sensory or motor control of the tongue and submental muscles during the oral stage of swallowing and subsequent penetration or aspiration [12].
Poor lip closure and bolus control had no direct relation with penetration or aspiration. These parameters of the oral stage of swallowing were related to sensory and motor skills of the lip and tongue. Lip and lingual control deficiencies after a stroke may be more related to anterior or lateral oral residues or swallowing apraxia. The results of this study are similar to those from previous literature [5]. On the other hand, poor lip closure and bolus control may be sole indicators of penetration or aspiration, but these may be related to other physiological indicators of dysphagia. For example, if a stroke survivor has difficulty in controlling the bolus in the oral cavity, the clinician could question the extent of tongue nerve and muscle damage and its association with delayed initiation of the swallow and reduced hyolaryngeal elevation. Tongue strength and coordination are critical in executing timely and appropriate hyolaryngeal elevation.
Stroke survivors showing penetration or aspiration had significantly more occurrences of delayed initiation of the swallow than those who did not. This significant difference indicated that stroke survivors with penetration or aspiration showed less sensory and motor control of the posterior tongue than those in the other group. These results were similar to previous studies of delayed initiation of the swallow [141516]. According to the fluoroscopic swallowing study, poststroke survivors with penetration or aspiration of the bolus experience delayed initiation of the swallow in conjunction with premature spillage. The function of the velum and base of the tongue may be impaired, and the sealing in the posterior oral cavity is not adequate. In addition, if the bolus enters the airway before the pharyngeal stage is triggered, stroke survivors can undergo penetration or aspiration before the swallow. Therefore, premature spillage and/or delayed initiation of the swallow can influence the presence of penetration or aspiration.
There was a significant difference between the two groups in relation to reduced hyolaryngeal elevation. Stroke survivors with penetration or aspiration had a more reduced hyolaryngeal excursion than the other group. According to Perlman et al. [9], aspirating patients showed limited and reduced elevation of the hyoid and larynx. Furthermore, the reduced movements of the hyoid and larynx could degrade protection of the airway and opening of the UES. Reduced laryngeal elevation could have a substantial effect on the presence of penetration or aspiration. On the other hand, residue in the vallecular and pyriform sinus did not show a significant difference between the two groups. However, stroke survivors with penetration or aspiration tended to have more vallecular and pyriform sinus residue than the other group, indicating a similar tendency found in previous studies that residue of food in the pharynx raised the risk of aspiration [131718]. Thus, it is necessary to study how residue of the vallecular and pyriform sinus may have an effect on penetration or aspiration.
In summary, this study confirmed previous findings relating to oral and pharyngeal indicators of penetration or aspiration in stroke survivors. The data of this study represented the ordinary fluoroscopic swallowing study setting in numerous hospitals of average clinical dysphagia caseloads, which can shed light on practical knowledge. It was our objective to ascertain whether or not clinical decision-making in ordinary fluoroscopic swallowing studies was related to physiological indicators, which has been reported previously numerous times. It was our finding that the experienced clinicians were able to develop skills to make a decision on the physiological causes of penetration and aspiration during fluoroscopic swallowing studies. However, there is a question over how many years of clinical experiences are necessary to make such a decision. It is necessary to develop a training program and monitor clinicians' knowledge and skills in each clinical setting in order to improve the accuracy of their decision-making.
During the normal swallow, the airway is protected and the esophagus opens before the transition of the bolus from oral cavity to the pharynx [1920]. Timely and appropriate hyoid and larynx elevation is critical in performing these physiological events in safe swallowing. However, a stroke can have negative effects on swallowing physiology through reduced activation of motor and sensory cranial nerves and subsequent weakening of muscles in the oropharynx. This damage may put stroke survivors at risk of penetration or aspiration due to lack of airway protection and reduced esophagus opening.
This study reported that stroke survivors experienced various medical symptoms and signs poststroke whether or not they showed penetration or aspiration. Do medical symptoms and signs that occur after a stroke have no effect on swallowing disorders? No. In fact, there have been several reports that medical symptoms and signs can contribute to penetration and aspiration after a stroke [18212223]. This may suggest that medical symptoms and signs should be counted differently for each patient. It is difficult to find a condition to determine the presence of dysphagia based merely on medical records. In addition, each medical symptom and sign may be related to individual physiological signs of dysphagia. Since this study included a small number of stroke survivors, it is necessary to conduct further studies in order to examine the relation between physiological measurements of swallowing and medical history.
This study has several limitations including a small number of subjects and a heterogeneous group of stroke survivors with respect to the site of lesion and stroke severity. In addition, more physiological indicators of swallowing disorders should be included to understand the nature of swallowing disorders. The effects of stroke on swallowing are multi-faceted and must be examined from different perspectives in future research. More reliable and valid physiological measurements will enhance the findings of this study.
Future studies should focus on the relation between more physiological indicators of swallowing and other clinical signs of dysphagia. For example, temporal and biomechanical measurements of swallowing have been shown to be reliable tools for describing disordered swallowing functions [122425]. The finding of reliable clinical indicators of penetration or aspiration will help clinicians establish valid treatment strategies and follow-up plans based on risk of aspiration or penetration. There are several rehabilitation exercises such as the Mendelsohn maneuver and hard swallowing that can improve delayed initiation of the swallow and reduce hyolaryngeal elevation. Moreover, new treatments are always emerging. Compensatory strategies such as the chin-tuck procedure (touching the chin to the neck) have been demonstrated to reduce aspiration in some patients. More research regarding compensation for and rehabilitation of swallowing function specific to the clinical indicators of penetration or aspiration are needed.
References
1. Kidd D, Lawson J, Nesbitt R, MacMahon J. Aspiration in acute stroke: a clinical study with videofluoroscopy. Q J Med. 1993; 86:825–829. PMID: 8108539.
2. Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999; 30:744–748. PMID: 10187872.
4. Crausaz FM, Favez G. Aspiration of solid food particles into lungs of patients with gastroesophageal reflux and chronic bronchial disease. Chest. 1988; 93:376–378. PMID: 3338306.

5. Mann G, Hankey GJ. Initial clinical and demographic predictors of swallowing impairment following acute stroke. Dysphagia. 2001; 16:208–215. PMID: 11453569.

6. Power ML, Hamdy S, Singh S, Tyrrell PJ, Turnbull I, Thompson DG. Deglutitive laryngeal closure in stroke patients. J Neurol Neurosurg Psychiatry. 2007; 78:141–146. PMID: 17012336.

7. Robbins J, Levin RL. Swallowing after unilateral stroke of the cerebral cortex: preliminary experience. Dysphagia. 1988; 3:11–17. PMID: 3248391.

8. Robbins J, Levine RL, Maser A, Rosenbek JC, Kempster GB. Swallowing after unilateral stroke of the cerebral cortex. Arch Phys Med Rehabil. 1993; 74:1295–1300. PMID: 8259895.

9. Perlman AL, VanDaele DJ, Otterbacher MS. Quantitative assessment of hyoid bone displacement from video images during swallowing. J Speech Hear Res. 1995; 38:579–585. PMID: 7674650.

10. Cook IJ, Dodds WJ, Dantas RO, Kern MK, Massey BT, Shaker R, et al. Timing of videofluoroscopic, manometric events, and bolus transit during the oral and pharyngeal phases of swallowing. Dysphagia. 1989; 4:8–15. PMID: 2640180.

11. Perlman AL, Grayhack JP, Booth BM. The relationship of vallecular residue to oral involvement, reduced hyoid elevation, and epiglottic function. J Speech Hear Res. 1992; 35:734–741. PMID: 1405528.

12. Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA, Kahrilas PJ, Smith CH. Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. J Speech Lang Hear Res. 2000; 43:1264–1274. PMID: 11063246.

13. Perlman AL, Booth BM, Grayhack JP. Videofluoroscopic predictors of aspiration in patients with oropharyngeal dysphagia. Dysphagia. 1994; 9:90–95. PMID: 8005013.

14. Daniels SK, Schroeder MF, McClain M, Corey DM, Rosenbek JC, Foundas AL. Dysphagia in stroke: development of a standard method to examine swallowing recovery. J Rehabil Res Dev. 2006; 43:347–356. PMID: 17041820.

15. Miller JL, Watkin KL. The influence of bolus volume and viscosity on anterior lingual force during the oral stage of swallowing. Dysphagia. 1996; 11:117–124. PMID: 8721070.

16. Reddy NP, Thomas R, Canilang EP, Casterline J. Toward classification of dysphagic patients using biomechanical measurements. J Rehabil Res Dev. 1994; 31:335–344. PMID: 7869281.
17. Terre R, Mearin F. Oropharyngeal dysphagia after the acute phase of stroke: predictors of aspiration. Neurogastroenterol Motil. 2006; 18:200–205. PMID: 16487410.

18. Langmore SE, Terpenning MS, Schork A, Chen Y, Murray JT, Lopatin D, et al. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia. 1998; 13:69–81. PMID: 9513300.

19. Logemann JA. Evaluation and treatment of swallowing disorders. Austin: Pro-Ed;1998.
20. Cichero JA, Murdoch BE. Dysphagia: foundation, theory, and practice. New York: John Wiley & Sons;2006.
21. Ickenstein GW, Stein J, Ambrosi D, Goldstein R, Horn M, Bogdahn U. Predictors of survival after severe dysphagic stroke. J Neurol. 2005; 252:1510–1516. PMID: 16136260.

22. Mari F, Matei M, Ceravolo MG, Pisani A, Montesi A, Provinciali L. Predictive value of clinical indices in detecting aspiration in patients with neurological disorders. J Neurol Neurosurg Psychiatry. 1997; 63:456–460. PMID: 9343123.

23. Masiero S, Pierobon R, Previato C, Gomiero E. Pneumonia in stroke patients with oropharyngeal dysphagia: a six-month follow-up study. Neurol Sci. 2008; 29:139–145. PMID: 18612760.

24. Robbins J, Hamilton JW, Lof GL, Kempster GB. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992; 103:823–829. PMID: 1499933.

25. Logemann JA, Pauloski BR, Rademaker AW, Kahrilas PJ. Oropharyngeal swallow in younger and older women: videofluoroscopic analysis. J Speech Lang Hear Res. 2002; 45:434–445. PMID: 12068997.
Fig. 1
The clinical indicators of dysphagia in the oral stage for two stroke survivor groups. Delayed swallow, delayed initiation of the swallow; Pen., penetration; Asp., aspiration.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download