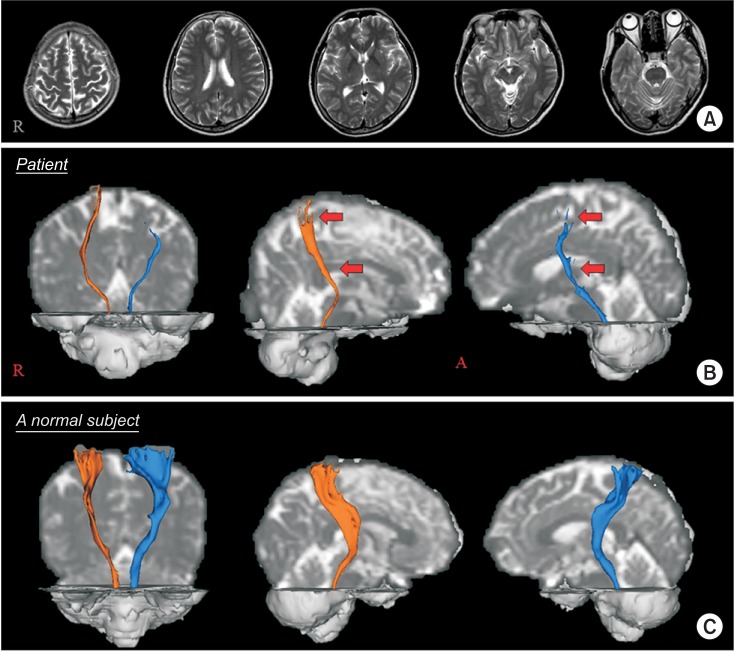
 | Fig. 1(A) T2-weighted brain magnetic resonance images at 10 months after head trauma show no abnormal lesion. (B) Diffusion tensor tractography for the spinothalamic tract show partial tearing and narrowing of the spinothalamic tracts in both hemispheres, as compared with those of a normal subject (53-year-old female). |
In this report, we described the case of a 54-year-old female who suffered trauma from a falling large box (100 cm×30 cm×30 cm) that hit the vertex of her head while seated in a subway car. The patient experienced loss of consciousness for several minutes, and post-traumatic amnesia for several minutes, with a Glasgow Coma Scale score of 15. She experienced severe bursting pain in her head, neck and upper back immediately after the head trauma; and approximately 3 hours later, she began to feel pricking pain in her left arm and leg. Despite visits to several hospitals to determine the cause of pain, no specific diagnosis was confirmed. Ten months post-injury, she visited the Department of Rehabilitation of a Yeunnam University Hospital with the chief complaint of constant pain with hyperalgesia in her head, left arm, and leg. The characteristics and severity of pain were as follows: head, pricking sensation (visual analogue scale [VAS], 5–7]; left arm, pricking and squeezing (VAS, 3–7); and left leg, bursting sensation (VAS, 6–7). The subscales of Nottingham Sensory Assessment indicated normal kinesthetic sensation score of the left extremities (24 out of a possible 24 points), but impaired tactile sensation score (10 out of a possible 20 points). Brain and spine magnetic resonance imaging revealed no specific focal lesion; additionally, an electromyography study showed no evidence of peripheral neuropathy or radiculopathy.
Diffusion tensor imaging data were acquired at 10 months post-injury using a 6-channel head coil on a 1.5T Philips Gyroscan Intera (Philips, Best, Netherlands). The Oxford Centre for Functional Magnetic Resonance Imaging of the Brain (FMRIB) Software Library (FSL; www.fmrib.ox.ac.uk/fsl) was used to analyze the diffusion-weighted imaging data. Fiber tracking was performed using a probabilistic tractography method based on a multifiber model. The spinothalamic tracts (STTs) were located by selection of fibers passing through regions of interest (ROIs). A seed ROI was placed on the posterolateral medulla on an axial slice and a target ROI was placed on the primary somatosensory cortex on an axial slice. The threshold of 1 streamline was applied for the results of fiber tracking [1]. Ten-month diffusion tensor tractography indicated partial tearing and narrowing of the STTs in both hemispheres (Fig. 1B). The patient was prescribed gabapentin (900 mg/day) for 1 month, which resulted in partial pain control to a tolerable level.
ACKNOWLEDGMENTS
This work was supported by the National Research Foundation (NRF) of Korea Grant funded by the Korean Government (MSIP) (2015R1A2A2A01004073).
Go to : 
References
1. Kim JH, Ahn SH, Cho YW, Kim SH, Jang SH. The relation between injury of the spinothalamocortical tract and central pain in chronic patients with mild traumatic brain injury. J Head Trauma Rehabil. 2015; 30:E40–E46.

2. Alexander MP. Mild traumatic brain injury: pathophysiology, natural history, and clinical management. Neurology. 1995; 45:1253–1260. PMID: 7617178.

3. Povlishock JT, Christman CW. The pathobiology of traumatically induced axonal injury in animals and humans: a review of current thoughts. J Neurotrauma. 1995; 12:555–564. PMID: 8683606.

4. Buki A, Povlishock JT. All roads lead to disconnection? Traumatic axonal injury revisited. Acta Neurochir (Wien). 2006; 148:181–194. PMID: 16362181.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download