Abstract
Objective
To determine whether there was a difference in balance, proprioception, and skeletal muscle mass among patients who undergo hip fracture surgery relative to and elective total hip replacement (THR).
Methods
Thirty-one THR patients were enrolled. The patients were categorized into two groups: fracture group (n=15) and non-fracture group (n=16). Berg Balance Scale (BBS) was used to balance the proprioception of the hip joint while a joint position sense (JPS) test was used to evaluate it. Skeletal muscle mass was measured by bioelectrical impedance analysis and expressed as a skeletal muscle mass index (SMI). Quality of life (QOL) was also assessed using a 36-item short form health survey (SF-36). All tests were assessed at 3 months after the surgery. An independent t-test was used to compare the fracture group and non-fracture group. Spearman correlation was used to identify the correlation of each variable.
Go to : 
Balance is achieved by not only proprioception, mentation, a vestibular system, vision and muscle strength but also through psychological factors [1]. Of these factors, proprioception has an important role in balance, postural and motor control. Proprioception is a conscious capacity to sense position, movement and force of body segments [2]. Joint capsules in the human body have numerous receptors to control posture. The cutaneous and musculoskeletal systems such as extra-capsular muscles and ligaments also have a lot of receptors [3456].
The hip joint is closely related to the postural stability and balance among these joints [7]. The hip joint affects degenerative diseases such as osteoarthritis (OA) and osteonecrosis, as well as autoimmune diseases like rheumatoid arthritis (RA) [8]. It also is easily fractured often from slipping or falling down. A total hip replacement (THR) is the preferred treatment for patients with hip problems. A THR reduces the pain effectively and provides reliable stability. It also increases the mobility and quality of life (QOL) [9]. Depending on the cause, THR patients can be divided into a fracture group and non-fracture (elective) group.
There are previous studies regarding the improvement of balance after THR for OA patients with hip diseases. Wykman and Goldie [1] reported that postural stability often improved 1 year after THR and one's sway pattern became normal. Majewski et al. [9] and Lugade et al. [10] also suggested that THR could help OA patients to regain an almost normal control of balance. In addition, others suggested that the balance of THR patients was affected by the strength of one's hip [1112], whereas this pilot study assessed skeletal muscle mass. To our knowledge, there is no report to compare balance, proprioception and skeletal muscle mass of THR patients between the fracture group and non-fracture group.
The purpose of this pilot study was to compare hip proprioception, balance and other variables (skeletal muscle mass, QOL) between the fracture group and non-fracture group after THR.
Go to : 
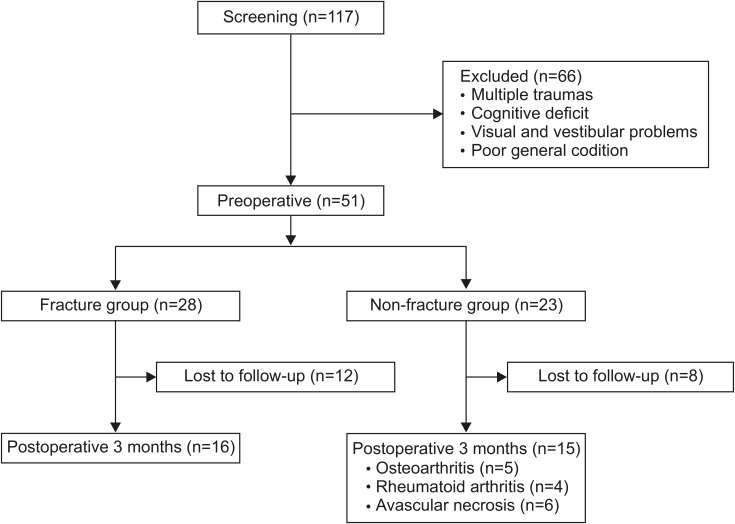
We collected information about patients who had THR from orthopedic surgery at Hanyang University Hospital in Seoul between January 2014 and April 2015. One hundred seventeen patients were hospitalized and referred to the Department of Physical Medicine and Rehabilitation during the study period. The patients had a unilateral THR regardless of the cause and all patients experienced the posterior approach method. Sixty-six were excluded because of multiple traumas other than the hip, poor general condition, cognitive deficit, or visual and vestibular system problems. The remaining 51 patients were willing to participate in the study. However, only 31 patients were included in the final analysis because 20 patients did not respond to any follow-up attempts (Fig. 1). The Institutional Review Board approved the research; all patients voluntarily agreed to the informed consent, and an evaluation was conducted 3 months after surgery.
A gait analysis and other complete specific gait and balance tasks are needed to measure the accurate functional outcome of balance [1314]. However, in this study BBS was used because it can be performed easily in clinical practice. The BBS is comprised of 14 tasks and is scored on a 5-point scale (0–4). The test takes about 20 minutes. The practitioner measures the time it takes to finish a task completely and ranks the performance quality. The maximum score is 56 [15].
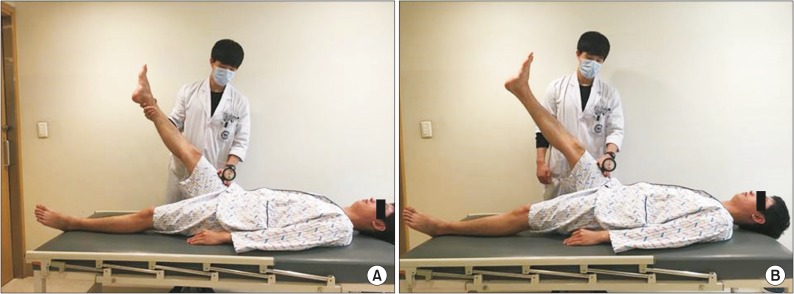
There are no standards to evaluate proprioception even though there have been various attempts. JPS test is a simple method to measure the accuracy of position replication, and that can be performed actively or passively in both open and closed kinetic chain positions [16]. We measured the hip flexion in a supine position. The inclinometer was put in a sagittal plane at the anterior portion of the thigh, and the knee was extended and moved to reproduce an angle (60°) passively (Fig. 2A). The patient was informed of the 60° position and asked to position again actively, which was then measured (Fig. 2B). The measured degree and difference with 60° were recorded. The tests were done 3 times and the average was recorded.
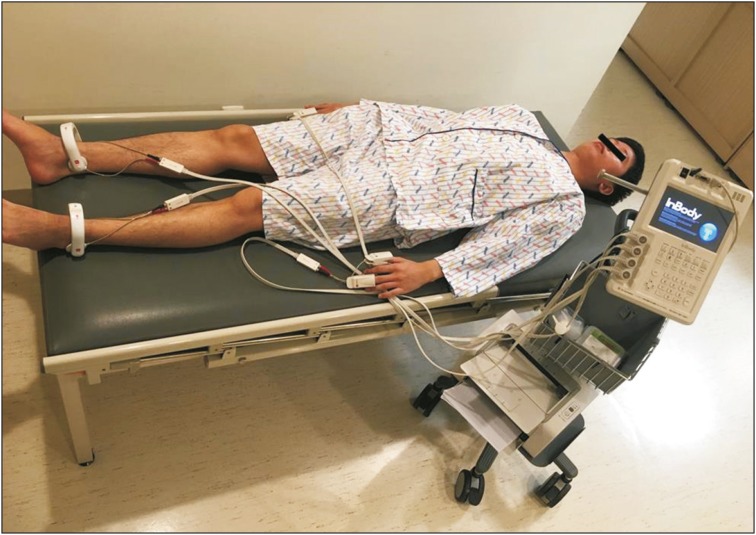
Skeletal muscle mass was measured using bioelectrical impedance analysis (InBody S10; Biospace, Seoul, Korea) (Fig. 3). After height and weight were measured, four electrodes were attached to both upper and lower extremities in the supine position. As an index of muscle mass, we used the skeletal muscle mass index (SMI) calculated as [17]:
The QOL was measured using the 36-item short form health survey (SF-36). The SF-36 is a questionnaire developed from the original lengthy battery of questions. It is a 36-item test and consists of 8 multi-item variables [18]. Each variable item score is coded and turned into a 0–100 scale (0, the worst; 100, the best possible health state).
The independent t-test was used to compare variables between the fracture group and non-fracture group after the surgery. The Spearman correlation was used to analyze the relation between balance, proprioception and skeletal muscle mass after the surgery. When the p-value is less than 0.05, it is considered to have statistical significance. The SPSS program for Windows ver. 20.0 (IBM, Armonk, NY, USA) was used for data analyses.
Go to : 
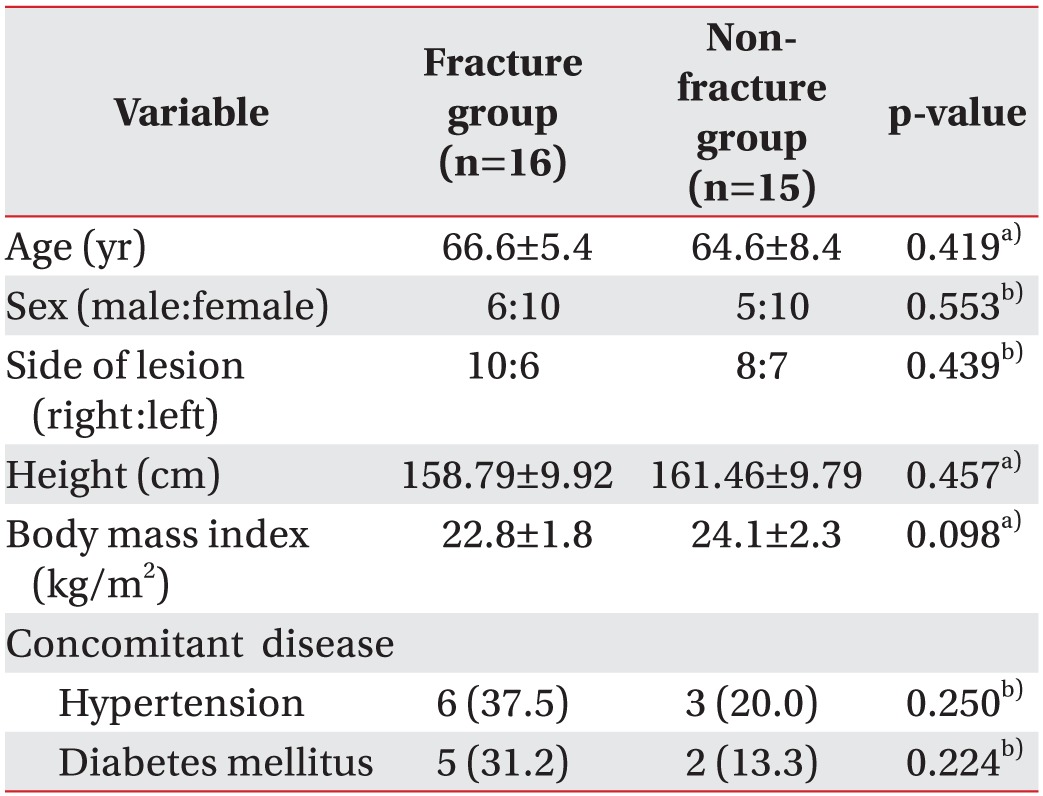
Characteristics of the study population are shown in Table 1. Thirty-one patients participated, 20 males and 11 females. The mean age of the patients was 65.35±13.44 years. Depending on the cause, they were divided into fracture group (n=16) and non-fracture group (n=15). Among the non-fracture group, 5 patients had OA, 6 patients had avascular necrosis and 4 patients had RA. All THR patients had postoperative tests after 3 months. There was no significant variable in demographic data between these two groups 3 months after the surgery.
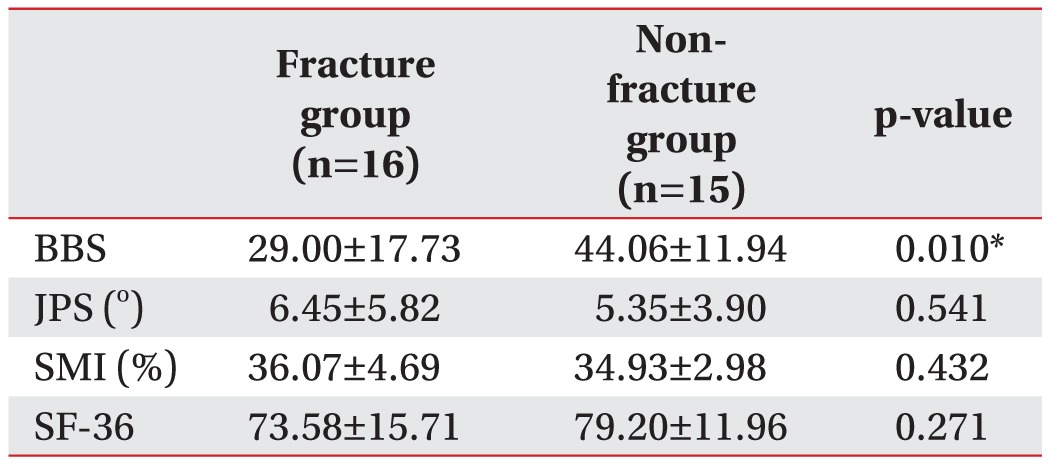
In the independent t-test result, 3 months after the surgery, BBS scores of the non-fracture group were 44.06±11.94 which was statistically higher than fracture group scores of 29.00±17.73 (p=0.010) (Table 2). However, there was no statistical significance in the JPS, SMI, and SF-36 between the two groups.
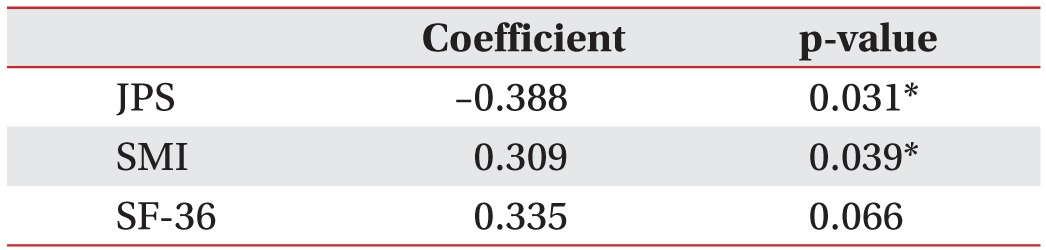
In the correlation between balance and other variables 3 months after the surgery, the BBS score and JPS were correlated (correlation coefficient=−0.388, p=0.031). The BBS score and SMI also showed a statistically significant correlation (correlation coefficient=0.360, p=0.047). The SF-36 was correlated with balance, but the correlation was not statistically significant (Table 3).
Go to : 
The primary finding of this pilot study was that the non-fracture group had a significantly better BBS scores than the fracture group 3 months after THR. We also found that BBS correlated with JPS, and BBS correlated with SMI. To our knowledge, this is the first study to evaluate balance, proprioception and skeletal muscle mass after THR.
Immediately after the THR surgery, the proprioceptor can be damaged due to a capsular excision. While removing a femoral head and reaming an acetabulum in the THR, it could damage a joint capsule and peripheral sensory system causing proprioception deterioration [19]. However, the proprioception can improve through restoring the mechanism for a joint position sense by removing deleterious factors after the surgery. Activities of daily living can be restored by reducing pain and chronic inflammation and reestablishing joint space and soft tissue tension after the surgery. This change modifies the response of the mechanoreceptor in capsuloligamentous and musculotendinous structure, and it increases the joint motion and perception of position [20].
The results of this pilot study indicated that balance of THR patients undergoing hip fracture surgery was better than those of elective THR patients. It might be that the patients who exhibited poor balance had a higher risk of falling or slipping down than patients who had good balance. Additionally, Le Manach et al. [21] reported the complications (myocardial infarction, pulmonary embolism, pneumonia, sepsis, stroke, major bleeding and disability) and mortality rate are higher in THR patients undergoing hip fracture surgery than elective THR patients. The proprioception and skeletal muscle mass did not have a significant difference between the two groups. The hip joint proprioception compromises the joint sensation due to joint capsule and sensory structure damage. Therefore, it would depend more on the surgery method than the cause. Further studies, including preoperative tests, would be needed to verify results found in this study.
The proprioception and balance were correlated 3 months after THR and is considered a contributing factor in the balance deficit for the patients who lost their joint sensation due to surgery or injury [22]. Therefore, it is important to re-establish joint sensation and the ability to balance for a positive outcome for the patients. Impaired balance after surgery was related to the frequency of falling, which increases mortality and reduces the QOL [21]. As a result of our result regarding the correlation between the JPS and BBS, a proprioception of the hip joint could be used to predict balance at an early stage of THR. Even if further studies are necessary in the future, these approaches might be used for early detection of decreased balance to minimize fall-related injury.
This study also showed the correlation between the skeletal muscle mass and balance of THR patients. After surgery it is difficult to anticipate balance because many patients are bedridden and immobilized. The muscle strength is also difficult to measure due to pain, limitation of motion and poor position, but the muscle mass can be simply measured using the bioelectrical impedance measurement. Therefore, balance deterioration might be predicted to some degree by measuring the skeletal muscle mass for THR patients whose muscle strength is difficult to measure.
This pilot study had several limitations. The first limitation of this study is the number of people included in the study. Secondly, findings of this pilot study were limited to postoperative data. We did not measure preoperative data of BBS, JPS, skeletal muscle mass, and other functional tests. To generalize the results of this study, additional studies including preoperative test may be needed. Thirdly, the study did not measure kinesthesia even if the human proprioception includes body segment position (JPS) and movement (kinesthesia) [23]; only flexion (60°) of the hip joint was measured. If the patients had had tightness in their hamstring muscles, measurement would not be accurate. In further studies measuring lower degrees (e.g., 30°) of the hip joint flexion is needed. Additionally, the proprioception findings in this study are limited to flexion of the hip joint. External rotation of the hip is also important proprioception performance. Forth, we did not measure the pain of THR patients. Fracture induces alterations in hemodynamic, metabolic, and immune responses, which are largely orchestrated by cytokines. The pain is generated from cytokines and C-reactive protein (CRP) like interleukin-6 (IL-6) from acute inflammation [2425]. It compromises the afferent joint sensation and interferes with reflexive motor coordination [23], and decreased joint function is a major risk factor for falling. Following this mechanism, the severe pain of THR patients undergoing hip fracture surgery would affect the balance for approximately 3 months. In further studies, investigation about the pain of THR, such as visual analogue scale (VAS) patients, is needed. The last limitation of this study is the short-term outcome. There needs to be a larger study with long-term follow-up including preoperative and postoperative tests.
In conclusion, THR patients undergoing hip fracture surgery might have more trouble balancing than elective THR patients. Although further studies including preoperative tests are necessary, THR patients undergoing hip fracture surgery might need more care during rehabilitation.
Go to : 
ACKNOWLEDGMENTS
This research is supported by Ministry of Culture, Sports and Tourism (MCST) and Korea Creative Content Agency (KOCCA) in the Culture Technology (CT) Research & Development Program 2016.
Go to : 
References
1. Wykman A, Goldie I. Postural stability after total hip replacement. Int Orthop. 1989; 13:235–238. PMID: 2599698.

2. Lephart SM, Pincivero DM, Rozzi SL. Proprioception of the ankle and knee. Sports Med. 1998; 25:149–155. PMID: 9554026.

3. Skinner HB, Wyatt MP, Hodgdon JA, Conard DW, Barrack RL. Effect of fatigue on joint position sense of the knee. J Orthop Res. 1986; 4:112–118. PMID: 3950803.

4. Swash M, Fox KP. The effect of age on human skeletal muscle: studies of the morphology and innervation of muscle spindles. J Neurol Sci. 1972; 16:417–432. PMID: 4261815.

5. Kim GH, Suzuki S, Kanda K. Age-related physiological and morphological changes of muscle spindles in rats. J Physiol. 2007; 582:525–538. PMID: 17495047.

6. Bruce MF. The relation of tactile thresholds to histology in the fingers of elderly people. J Neurol Neurosurg Psychiatry. 1980; 43:730–734. PMID: 7431035.

7. Wingert JR, Welder C, Foo P. Age-related hip proprioception declines: effects on postural sway and dynamic balance. Arch Phys Med Rehabil. 2014; 95:253–261. PMID: 23994251.

8. Thewlis D, Hillier S, Hobbs SJ, Richards J. Preoperative asymmetry in load distribution during quiet stance persists following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014; 22:609–614. PMID: 23881256.
9. Majewski M, Bischoff-Ferrari HA, Gruneberg C, Dick W, Allum JH. Improvements in balance after total hip replacement. J Bone Joint Surg Br. 2005; 87:1337–1343. PMID: 16189304.

10. Lugade V, Klausmeier V, Jewett B, Collis D, Chou LS. Short-term recovery of balance control after total hip arthroplasty. Clin Orthop Relat Res. 2008; 466:3051–3058. PMID: 18781366.

11. Rasch A, Dalen N, Berg HE. Muscle strength, gait, and balance in 20 patients with hip osteoarthritis followed for 2 years after THA. Acta Orthop. 2010; 81:183–188. PMID: 20367414.

12. Judd DL, Dennis DA, Thomas AC, Wolfe P, Dayton MR, Stevens-Lapsley JE. Muscle strength and functional recovery during the first year after THA. Clin Orthop Relat Res. 2014; 472:654–664. PMID: 23817756.

13. Shumway-Cook A, Horak FB. Assessing the influence of sensory interaction of balance: suggestion from the field. Phys Ther. 1986; 66:1548–1550. PMID: 3763708.
14. Arnold W, Schliebe G. Gait analysis in patients with total hip endoprosthesis. Part II: Pre- and postoperative gait analysis. Z Gesamte Inn Med. 1992; 47:15–20. PMID: 1570718.
15. Bogle Thorbahn LD, Newton RA. Use of the Berg Balance Test to predict falls in elderly persons. Phys Ther. 1996; 76:576–583. PMID: 8650273.

16. Riemann BL, Myers JB, Lephart SM. Sensorimotor system measurement techniques. J Athl Train. 2002; 37:85–98. PMID: 16558672.
17. Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002; 50:889–896. PMID: 12028177.

18. Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. BMJ. 1993; 306:1437–1440. PMID: 8518639.

19. Goldie PA, Bach TM, Evans OM. Force platform measures for evaluating postural control: reliability and validity. Arch Phys Med Rehabil. 1989; 70:510–517. PMID: 2742465.
20. Lephart SM, Perrin DH, Fu FH, Gieck JH, McCue FC, Irrgang JJ. Relationship between selected physical characteristics and functional capacity in the anterior cruciate ligament-insufficient athlete. J Orthop Sports Phys Ther. 1992; 16:174–181. PMID: 18796757.

21. Le Manach Y, Collins G, Bhandari M, Bessissow A, Boddaert J, Khiami F, et al. Outcomes after hip fracture surgery compared with elective total hip replacement. JAMA. 2015; 314:1159–1166. PMID: 26372585.

22. Lindemann U, Becker C, Unnewehr I, Muche R, Aminin K, Dejnabadi H, et al. Gait analysis and WOMAC are complementary in assessing functional outcome in total hip replacement. Clin Rehabil. 2006; 20:413–420. PMID: 16774092.

23. Swanik CB, Lephart SM, Rubash HE. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg Am. 2004; 86-A:328–334. PMID: 14960678.

24. Beloosesky Y, Hendel D, Weiss A, Hershkovitz A, Grinblat J, Pirotsky A, et al. Cytokines and C-reactive protein production in hip-fracture-operated elderly patients. J Gerontol A Biol Sci Med Sci. 2007; 62:420–426. PMID: 17452737.

25. Miller RR, Shardell MD, Hicks GE, Cappola AR, Hawkes WG, Yu-Yahiro JA, et al. Association between interleukin-6 and lower extremity function after hip fracture: the role of muscle mass and strength. J Am Geriatr Soc. 2008; 56:1050–1056. PMID: 18410321.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download