INTRODUCTION
In patients with spinal cord injury, impaired urinary bladder function is a major complication. Neurogenic bladder, especially the overactive type, causes bladder dysfunction such as urinary incontinence and reduced bladder capacity, and it lowers quality of life [
1]. Additionally, prolonged neurogenic bladder may cause ureterovesical reflux resulting in renal damage, which reduces lifespan [
2]. Patients with this symptom should take anticholinergic drugs to suppress detrusor muscle pressure and perform 5 times a day or so to avoid urinary incontinence. However, anticholinergics have side effects such as thirst, memory impairment, reduced sweating, emotional disturbance, constipation, pupil dilatation, visual disturbances, and tachycardia [
3], and clean intermittent catherization might cause urethral discomfort and possible urinary tract infections [
4]. For these reasons, alternative treatments have been introduced.
Previous studies have reported that selective sacral rhizotomy in patients with neurogenic bladder increased bladder capacity and improved urinary incontinence. The rationale for this procedure was to denervate sacral nerves that were innervating the detrusor muscle to attenuate the bladder spasm and hypertonicity in neurogenic bladder [
567]. However, this procedure is destructive and is difficult to perform repeatedly. Percutaneous radiofrequency (RF) sacral rhizotomy was first introduced for treating hyperreflexic bladder by Mulcahy and Young [
89]. They reported augmentation of bladder capacity and observed successful preservation of its effect over nine years later. Ferreira reported on the effects of sacral rhizotomy by percutaneous continuous radiofrequency (CRF), which uses high-frequency waves to ablate nerves in patients with hyperactive neurogenic bladder that results in increased maximal cystometric capacity and reduced detrusor pressure at maximal cystometric capacity [
10]. Cho and Lee [
11] reported that bilateral S2 or S3 monopolar CRF sacral rhizotomy improved bladder capacity and urinary incontinence in patients with spinal cord injury with intolerable neurogenic bladder. They reported that there were no complications such as pain, focal discomfort around the treated area, or sexual dysfunction. However, no reports have been issued regarding the effect of bipolar CRF on sacral nerves in patients with an overactive neurogenic bladder. Therefore, in the present study, which was conducted using a small number of subjects and a randomized controlled design, we investigated the short-term effect of bipolar RF ablation of sacral nerves because of neurogenic detrusor overactivity in spinal cord injury patients.
Go to :

MATERIALS AND METHODS
Subjects
We recruited patients with spinal cord injury (American Spinal Injury Association [ASIA] scale A & B) with neurogenic detrusor overactivity who had been treated for more than one year. Ten patients were recruited (male 7, female 3; mean age, 41.2±8.01 years). The exclusion criteria were as follows: 1) age <20 years or >70 years; 2) previous surgery for bladder or prostate; 3) presence of indwelling catheterization; 4) medical problems such as refractory hypertension or cardiovascular diseases; 5) coagulopathies; 6) pregnancy; and 7) ASIA scale C, D, or E. The Institutional Review Board of our hospital approved the study protocol. All involved subjects provided written, informed consent. Patients were allocated to two groups in a 1:1 ratio-the intervention group (n=5), members of which received percutaneous bipolar continuous RF on the S2 and S3 spinal nerves (male 3, female 2; mean age, 42±8.46 years; mean disease duration, 91±31 months), and the control group (n=5), members of which received conventional medical treatment (male 4, female 1; mean age, 40.4±8.4 years; mean disease duration of disease, 56±32 months).
Clinical evaluations
A three-day voiding diary was collected from patients in the intervention group before the procedure and at 2, 4, 8 and 12 weeks after intervention. The voiding diary consisted of frequency and volume of voiding and frequency and volume of urinary incontinence during one day. In addition, the International Consultation on Incontinence Questionnaire (ICIQ) and the urinary incontinence quality of life scale (IQOL) were administered before intervention and at 2, 4, 8, and 12 weeks after intervention. The ICIQ is a questionnaire that evaluates the symptoms of incontinence, and its reliability and validity have been well-established [
12]. The IQOL is a questionnaire that evaluates urinary incontinence and quality of life and is known to have excellent repeatability and validity for evaluating quality of life in patients with urinary incontinence [
1314]. Patients in the control group were evaluated in the same manner regarding the three-day voiding diary, ICIQ and IQOL.
An urodynamic study (UDS) was performed in the intervention group before and 12 weeks after intervention using Duet LOGIC G2 (Mediwatch Plc, West Palm Beach, FL, USA). UDS provides a useful means of assessing the physiological function and pathology of the lower urinary tract in patients with neurogenic bladder [
15]. It measures maximum cystometric capacity, maximum detrusor pressure during filling, volume at maximal detrusor pressure during filling, and reflex detrusor volume at first contraction. For the UDS, the bladder was filled with 24 mL/min of normal saline, and detrusor pressure was defined as the difference between intravesical and abdominal pressure. Patients in the control group underwent the urodynamic study at baseline and three months after baseline.
The bipolar continuous radiofrequency procedure
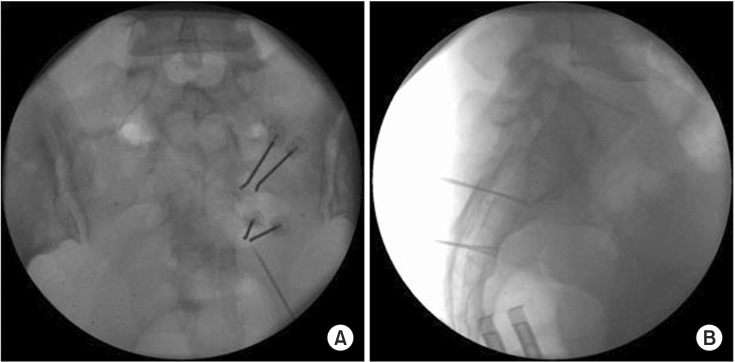
In a prone position, insertion sites were determined using two curved-tip 10-cm 18-gauge cannulae under fluoroscopic guidance. After these two cannulae were inserted, the tips were placed as close as possible to the S2 or S3 nerves under AP fluoroscopic guidance, and optimal electrode position was confirmed by lateral fluoroscopic imaging to be not beyond the ventral surface of the optimal electrode position or beyond the sacral ventral surface. Sensory nerve stimulation was then performed using an RF generator G4 (Cosman Medical Inc., Burlington, MA, USA). During sensory nerve stimulation, paresthesia, pain and muscle contraction around the sacrum should be observed at <0.7 V. After the cannulae had been placed in the required position, contrast was injected to confirm the absence of contrast material in the subarachnoid and intravascular spaces. RF was applied for 90 seconds at a tip temperature of <80℃. The procedure was performed in this manner at both the S2 and S3 nerve segments (
Fig. 1).
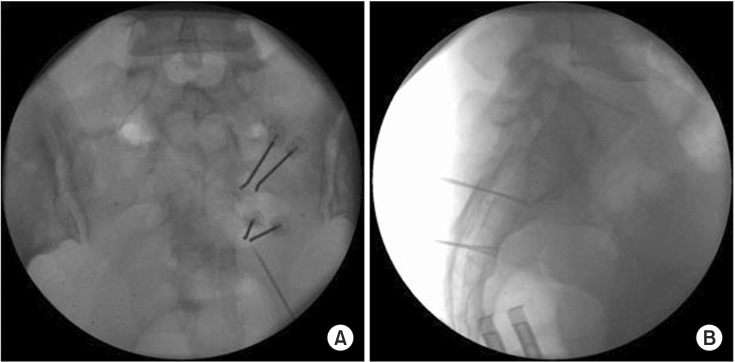 | Fig. 1(A) The anteroposterior view of bipolar radiofrequency on the right S2 and S3 nerve roots. (B) The lateral view of bipolar radiofrequency on the right S2 and S3 nerve roots.
|
Statistical analysis
SPSS ver. 19.0 software (SPSS Inc., Chicago, IL, USA) was used for the data analysis. To analyze daily mean frequency and volume of urinary incontinence and ICIQ and IQOL scores, we used repeated-measure two-factor analysis, and to analyze differences between baseline and follow-up UDS parameters (maximum cystometric capacity, maximum detrusor pressure during filling, volume at maximal detrusor pressure during filling, and reflex detrusor volume at first contraction), we calculated pre/post intervention differences. The Mann-Whitney U test was used to compare the patient and control groups with respect to the pre/post values of the UDS parameters. Statistical significance was accepted for p-values <0.05.
Go to :

RESULTS
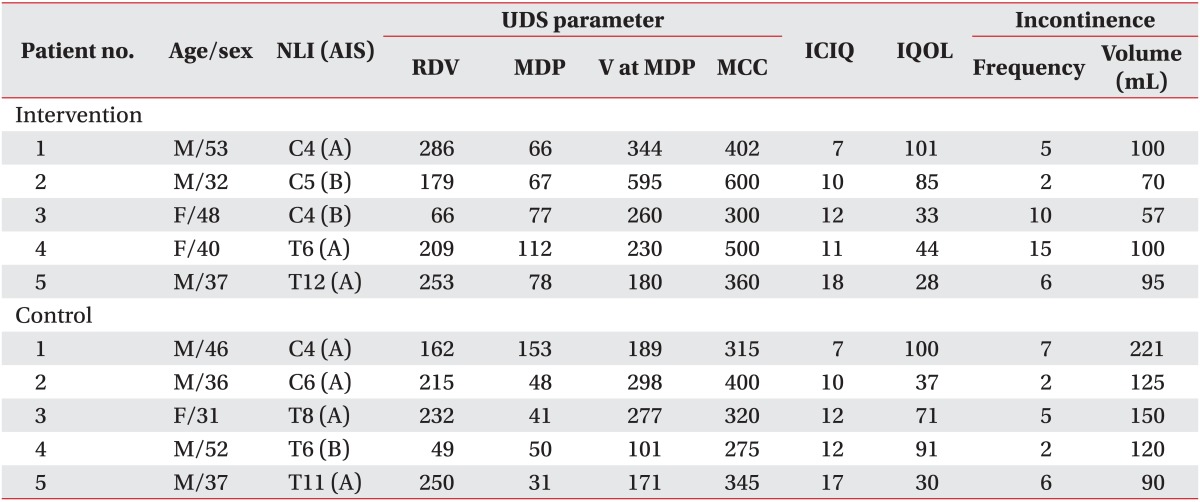
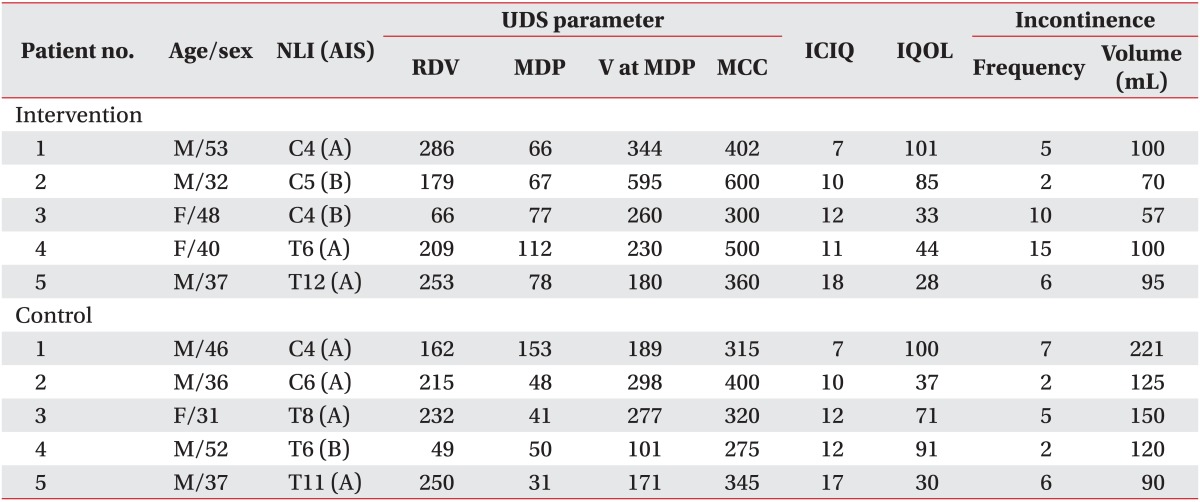
Table 1 shows the patients' demographic and clinical data including baseline values for UDS parameters, ICIQ and IQOL scores, and daily mean frequency and volume of urinary incontinence.
Table 1
Patients' demographic and clinical data

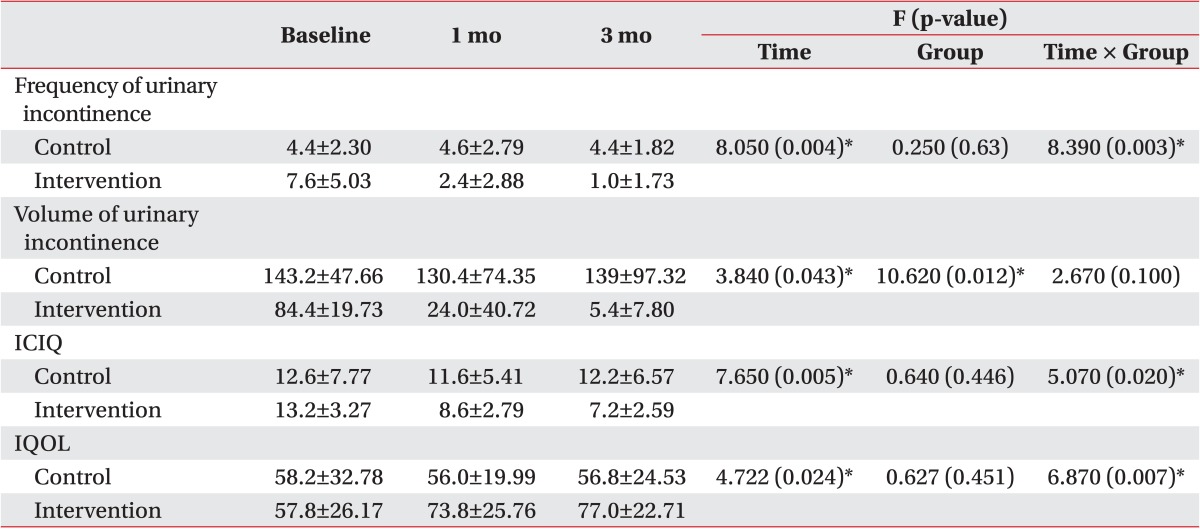
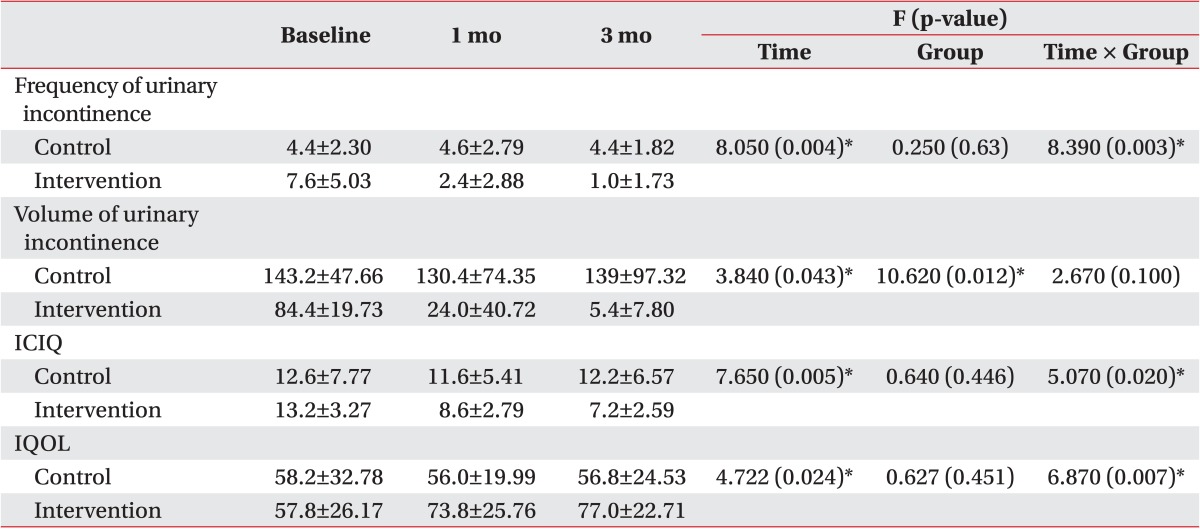
The comparisons by time, group, and time×group regarding daily mean frequency and volume of urinary incontinence and ICIQ and IQOL scores at baseline and at 1 and 3 months after intervention are shown in
Table 2. These variables achieved a significant effect for time (p<0.05), and for the group×time interaction, frequency of urinary incontinence and ICIQ and IQOL scores achieved statistical significance. Only daily mean volume of urinary incontinence showed a significant group effect (
Fig. 2).
 | Fig. 2A comparison of daily frequency and volume of urinary incontinence and ICIQ and IQOL scores at baseline and at 1 and 3 months after intervention. (A) Frequency of urinary incontinence, (B) volume of urinary incontinence, (C) ICIQ, and (D) IQOL. ICIQ, International Consultation on Incontinence Questionnaire; IQOL, urinary incontinence quality of life scale. Values are presented as mean (standard error).
|
Table 2
Daily mean frequency and volume of urinary incontinence and ICIQ and IQOL scores at baseline and 1 and 3 months after intervention in the two study groups

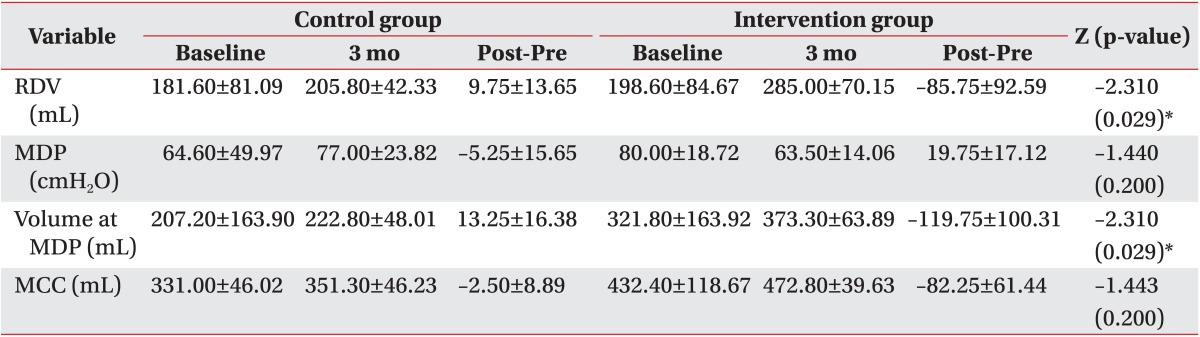
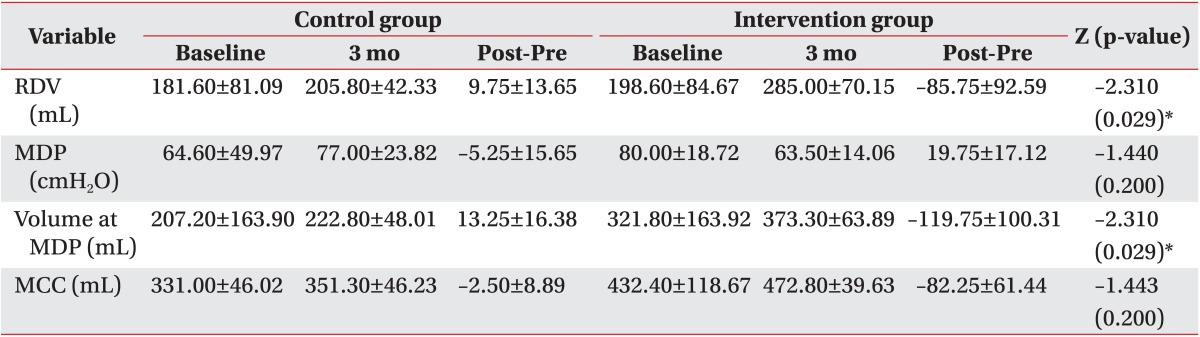
Values of UDS parameters at baseline and follow-up and pre/post differences in both groups are shown in
Table 3. Differences in volume at maximal detrusor pressure during filling and reflex detrusor volume at first contraction exhibited significant intergroup differences (p<0.05), whereas maximum cystometric capacity and maximum detrusor pressure during filling did not (p>0.05).
Table 3
Values of UDS parameters at baseline and follow-up and pre/post differences in the intervention and control groups

Go to :

DISCUSSION
Contraction of the urinary bladder that causes bladder emptying is controlled by parasympathetic segments that originate from the 2nd, 3rd, and 4th sacral cord segments, and the segments of this nerve innervate the visceral motor neurons in the parasympathetic ganglia around the bladder wall. In patients with spinal cord injury who have lost descending control of the sacral spinal cord, autonomic regulation of bladder continues, and the micturition is simulated reflexively at the level of the sacral cord. However, this reflex is ineffective when descending motor control is damaged and causes urinary dysfunction [
16]. It has been demonstrated that removing the sacral reflex arc might liberate the bladder from any possible stimulatory or inhibitory impulses from higher centers [
17]; as such, selective sacral rhizotomy has been performed to increase bladder capacity and preserve detrusor reflex and sphincter function in patients with neurogenic bladder.
RF ablation ablates nerves by generating heat via a high-frequency alternating current [
18]. In the present study, we used this technique to ablate both the S2 and S3 nerves using bipolar electrodes. In a previous study, monopolar CRF was performed on sacral nerves in spinal cord injury patients with neurogenic bladder [
9]. Monopolar RF has been widely used in neurosurgery and for pain management, but bipolar RF has not been used frequently and is less well understood. However, it is known that bipolar RF might be more effective than monopolar RF because whereas monopolar RF generates an RF current between an electrode's exposed tip and a distant ground pad, bipolar RF generates RF current between two closely positioned electrode tips, which allows for higher RF electrical fields to be generated, more rapid tissue heating, and the ability to generate larger lesions than is possible by monopolar RF [
192021].
In the current study, we investigated the effect of bipolar CRF on sacral nerves to treat neurogenic detrusor hyperactivity patients with spinal cord injury. We expected to find that intervention would increase bladder capacity and reduce uninhibited bladder contraction. Improvements in daily mean frequency and volume of urinary incontinence and in ICIQ and IQOL scores were observed in the intervention group compared with the control group with respect to time, which indicates that these variables showed significant changes regardless of a group effect. Additionally, in the group×time interaction, frequency of urinary incontinence and ICIQ and IQOL scores achieved statistical significance, indicating that these variables showed significant differences between the two groups according to time. In addition, there were significant intergroup differences in pre/post volume differences at maximal detrusor pressures during filling and in reflex detrusor volumes, but pre/post differences in maximal detrusor pressure during filling and maximal cystometric capacity were not significantly different. We believe that these results might be attributable to the small number of subjects we recruited. Nevertheless, bipolar CRF ablation of sacral nerves would appear to be effective in patients with spinal cord injury with hyperactive neurogenic bladder because it improves QOL by attenuating the frequency of urinary incontinence. In fact, all patients had used medications for neurogenic bladder, but medication use after intervention changed only in the intervention group; two patients reduced their use of anticholinergics from two medicines to one; one patient ceased to use any anticholinergics; one reduced anticholinergic use from four to two medicines; and one reduced anticholinergic use from three to two medicines.
Other favorable effects were found in the intervention group. First, three patients reported improvements in defecation. Before intervention, they had typically defecated every four or five days on laxatives and took more than 30 minutes per defecation, whereas after intervention, they defecated every one or two days and took within 30 minutes without laxatives. Although the pathogenetic mechanism that was responsible for this effect is not known, we suggest that RF applied to sacral nerves might have caused denervation of the pudendal nerve and reduce anal sphincter tone. Furthermore, reduced use of anticholinergics would have affected defecation in the intervention group. Second, one patient in the intervention group mentioned that neuropathic pain in the inguinal area was improved after intervention. He reported feeling an uncomfortable pain, described as a sharp tingling sensation in the inguinal area before intervention, which was nearly resolved after intervention. Third, another patient in the intervention group reported that symptoms of autonomic dysreflexia were resolved. He usually experienced symptoms described as a pounding headache, flushing, and sweating before intervention, but he found that the symptom of intervention autonomic dysreflexia completely resolved after intervention.
Percutaneous RF is more cost-effective and less invasive than other procedures that are used to treat neurogenic bladder, such as neuromodulation therapy. Neuromodulation, which requires that after successful sacral nerve stimulation, a generator and lead be implanted, is known to be an effective therapy in patients with hypertonic bladder that is responsive to conservative treatment. However, the cost of initial therapy is $1,800 to test sacral nerve stimulation, and for ongoing therapy, the cost of a sacral nerve stimulation surgical implant is in the area of $23,000 [
22]. In contrast, the cost of applying bipolar CRF to sacral nerves is $300-$400, and thus, bipolar CRF is most likely the most cost-effective therapy for spinal cord injury patients with neurogenic bladder.
In conclusion, this study shows that applying percutaneous bipolar CRF to sacral nerves offers an effective means for treating neurogenic overactive bladder and that it reduces urinary incontinence and improves quality of life. In addition, RF is relatively safe, cost-effective and repeatable. Furthermore, no serious side effects, such as intervention site infection or serious erectile dysfunction, were encountered after intervention. Although some members of the intervention group experienced discomfort around the intervention site after intervention, they reported that it had lasted only a few days. The major limitation of this study is the small number of subjects enrolled. Furthermore, we evaluated results at only three months after intervention. Accordingly, we suggest that additional larger-scale, longer follow-up studies be conducted.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download