Abstract
Objectives
To investigate cognition, social adaptive functioning, behavior, and emotional development in the preschool period and to determine the effects of the age of onset of walking on those developmental areas in children who were born preterm without major neurodevelopmental impairments (NDI) early in life.
Methods
Fifty-eight children who were born preterm without major NDI early in life participated in this study. The Korean versions of the Wechsler Preschool and Primary Scale of Intelligence or the Bayley Scales of Infant Development, the social maturity scale, the Korean version of the Child Behavior Checklist (CBCL), Conners' abbreviated parent/teacher rating scale, the Childhood Autism Rating Scale, and a speech developmental test were administered. The participants were divided into two groups: early walkers (group A) and late walkers (group B).
Results
The full-scale intelligence quotient (IQ) and performance IQ were significantly lower in group B than in group A, while the verbal IQ did not differ significantly between the groups. The children in group B had greater risks of cognitive deficits than did the children in group A, especially in performance skills. The social quotient (SQ) was significantly lower in group B than in group A (p<0.05). The rates of mild or significant deficits based on SQ and the CBCL did not differ significantly between the groups. Four children in group A and one child in group B had attention/hyperactivity problems. One child in group A had autistic behavior. Only one child in group B showed a significant speech developmental delay.
Infants born preterm are at greater risk of developing motor, cognitive, language, and behavioral impairments compared with infants born at term [12]. Thus, many previous studies have investigated neurodevelopmental outcomes in infants born preterm. In most cases, infants born preterm have follow-up care to detect developmental problems early in life. Most of these models of follow-up care are intended primarily for the early detection of major neurodevelopmental impairments (NDI) such as cerebral palsy (CP), intellectual disability, epilepsy, and severe visual/hearing problems, to allow for early intervention and therefore minimize future sequelae [3].
In recent years, the incidence of major NDI has remained consistent, but the incidence of mild dysfunctions such as learning disabilities, attention deficit/hyperactivity, borderline intelligence, and behavioral problems has increased [4]. According to previous studies, normal outcomes or mild deficits are more prevalent than major NDI in children who were born preterm [456], and 73% of extremely preterm and 64% of very preterm children have normal outcomes or only mild deficits.
It is well-known that premature infants with major NDI are more likely to be impaired in various developmental domains compared with full-term infants [57]. In the literature, preterm infants are at high risk for problems in adaptive function, behavior, socio-emotional development and academic performance compared with full-term infants [689]. However, there is still a paucity of published data that describe the cognitive or neuropsychological outcomes of children who were born preterm without major NDI. Both parents and clinicians are greatly concerned as to whether children who were born preterm and free of major NDI early in life can develop normally in these various developmental domains.
Therefore, the aim of this study is to investigate the cognition, social adaptive functioning, behavior, and emotional development of children who were born preterm without major NDI early in life and to determine the effects of the age of onset of independent walking (AOW) on those developmental domains in these children.
At our institute, the infants who were born preterm who are referred to our clinic for developmental checkups are examined every 3-6 months. At every visit, gross and fine motor skills, postural tone development, and neurologic functions such as primitive reflexes, ankle clonus, spasticity, and movement patterns are assessed. Among those children with normal muscle tone and no abnormal findings on regular neurological examinations, the children without epilepsy or severe visual or hearing impairments; the children who could walk independently without any assistance and pick up small objects with a normal pincer grasp; and the children without any delays on the Clinical Adaptive Test/Clinical Linguistic and Auditory Milestone Scale (CAT/CLAMS) (developmental quotient≥85) [10] at 2 years of age were selected for this study. Even if there were no identifiable physical or mental impairments at the chronological age of 2 years, neuropsychologic assessments including assessment of speech development were recommended for all children after 3 years of age to assess cognition, social adaptive functioning, behavior, and emotional development. However, 24 (29.3%) of 82 children without major NDI at 2 years of age were lost during follow-up, and thus the drop-out rates for the assessment were 19 (30.6%) children in group A and 5 (25%) children in group B. There were no significant differences in the drop-out rates between groups.
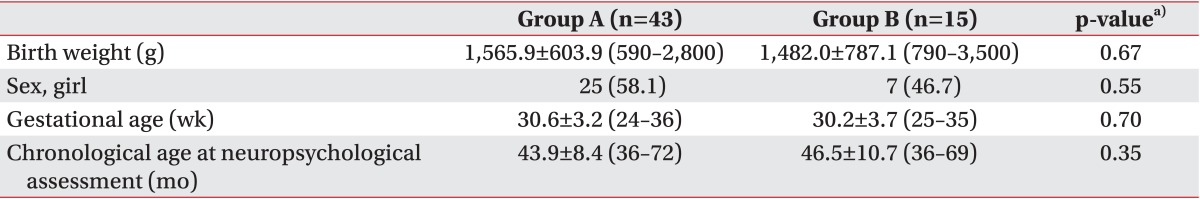
As a result, 58 children (26 boys, 32 girls) who had neuropsychological developmental assessments between 3 and 6 years of age (mean±standard deviation [SD], 3.7±0.7 years) participated in this study. The participants were divided into two groups based on the AOW, which is the age at which the infant can walk at least 10 steps independently without any assistance. Group A consisted of children with an AOW of 15 months or less, and group B consisted of children with an AOW between 15 and 24 months. There were no significant differences in birth weight, gestational age, age at assessment, or sex ratio between the two groups (Table 1).
This retrospective study was approved by the Institutional Review Board of Severance Hospital (No. 4-2013-0914).
The Korean versions of the Wechsler Preschool and Primary Scale of Intelligence, revised edition (K-WPPSI-R) is an intelligence test designed for children aged 3 years to 7 years 3 months. The K-WPPSI-R consists of subtests of verbal skills and performance skills. The verbal subtests include tests on information, comprehension, arithmetic, vocabulary, and similarities, and the performance subtests consist of tests on object assembly, geometric design, block design, mazes, and picture completion. The composite scores of K-WPPSI-R represent verbal intelligence quotient (IQ), performance IQ, and full-scale IQ. The Korean version of the Bayley Scales of Infant Development, second edition (K-BSID-II) is the most frequently used test in infant developmental assessment. This was replaced in 2006 by the Bayley scales of infant and toddler development, third edition (Bayley-III). The Bayley-III cognitive and language scores are up to 10 points higher than the mental developmental index (MDI) scores of K-BSID-II, and thus there is concern that the Bayley-III underestimates developmental delays [11]. Here, the K-BSID-II was administered in children who were not adequate for the K-WPPSI-R. The K-BSID-II comprises two scales: the MDI and the psychomotor developmental index (PDI). The MDI was designed to assess cognition by evaluating sensory perception, knowledge, memory, problem solving, and early language [12], whereas the PDI was designed to assess gross and fine motor skills. Based on the full-scale IQ determined using the K-WPPSI-R or the MDI determined using the K-BSID-II, the cognitive level of each child was classified as normal (IQ or MDI≥85), mild deficit (IQ or MDI≥70 but <85) or significant deficit (IQ or MDI<70).
The Korean version of the Social Maturity Scale (SMS), based on the fifth version of the Vineland Social Maturity Scale, was used to assess social adaptive functioning by measuring the personal and social skills needed for everyday living. This scale has been validated for the Korean population [13]. The 117-item scale can be used from birth until the age of thirty. It consists of 7 subscales that measure self-help general, self-help eating, self-help dressing, locomotion, occupation, communication, and socialization. Raw scores are converted to age-equivalent scores (expressed as social age [SA]), and then social maturity quotients (SQ=SA/chronological age×100) are calculated. For our study, social adaptive functioning was classified as normal (SQ≥85), mild deficit (70≤SQ<85) or significant deficit (SQ<70).
The Child Behavior Checklist (CBCL) was developed as a parent-completed questionnaire to assess a child's social competence and behavioral problems [14]. The Korean version of the CBCL has been validated in Korean children and adolescents [15]. The CBCL preschool version (CBCL/1.5-5) is used to assess behavioral problems in children aged 1.5 to 5 years [16]. Raw scores are converted to standardized T-scores, which have a normative group mean of 50 and standard deviation of 10. T-scores are compared with those of a Korean norm group. The CBCL/1.5-5 has seven subscales: emotionally reactive, anxious/depressed, aggressive behavior, attention problems, somatic complaints, withdrawn, and sleep problems. T-scores for total behavior problems, internalizing problems, and externalizing problems between 60 and 64 (60≤T<64) are considered borderline, and T-scores ≥64 are regarded as falling in the clinical range. T-scores on the 7 subscales between 65 and 70 (65≤T<70) are considered borderline, and T-scores≥70 are regarded as falling in the clinical range. Here, we classified children with T-scores≥60 for the broad-band scales and ≥65 for each syndrome as having behavioral problems.
The Conners' Abbreviated Parent/Teacher Rating Scale (CPRS) was developed to objectively assess behavioral symptoms related to attention deficit hyperactivity disorder (ADHD). An abbreviated questionnaire was also prepared by Conners [17] that consisted of 10 overlapping items drawn from the 93-item parent questionnaire [18] that were most frequently rated by both teachers and parents. It has been validated for the Korean population [19]. Each test item uses a four-point Likert scale that ranges from 'very unlikely (0)' to 'very likely (3)', where higher scores indicate more severe symptoms. The questionnaire was answered by parents and reviewed by an examiner. The cutoff value was 16 points, which is 2 standard deviations above the overall mean for the Korean population [19].
The Childhood Autism Rating Scale (CARS) is a caretaker-based interview rating scale that identifies autism features in children [20]. It has been validated for the Korean population [21]. The 15 CARS items are rated on a scale from 1 to 4 (none, mild, moderate, severe), for a maximum possible total score of 60. A score of 30 or above on the Korean version of the CARS was considered to be in the clinically significant range [21].
Language abilities were assessed with Sequenced Language Scale for Infants (SELSI) or Preschool Receptive-Expressive Language Scale (PRES); the former was used for children under the age of 3 years, and the latter for preschoolers above the age of 3 years. However, the SELSI was administered in some older children whose language levels were inadequate for the PRES. Both scales are validated in the Korean population [2223]. A significant speech development delay was defined as a developmental score two standard deviations away from the mean score of normally developed children, and a mild speech developmental delay was defined as a developmental score between 1 SD and 2 SD from the mean.
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) ver. 20 for Windows (IBM SPSS Inc., Armonk, NY, USA). An independent t-test was used to compare the means of the groups, and Fisher exact test was used to compare the differences in the distributions of normal or abnormal ranges in cognition, adaptive functioning, and behavior between the groups. A p-value less than 0.05 was considered statistically significant.
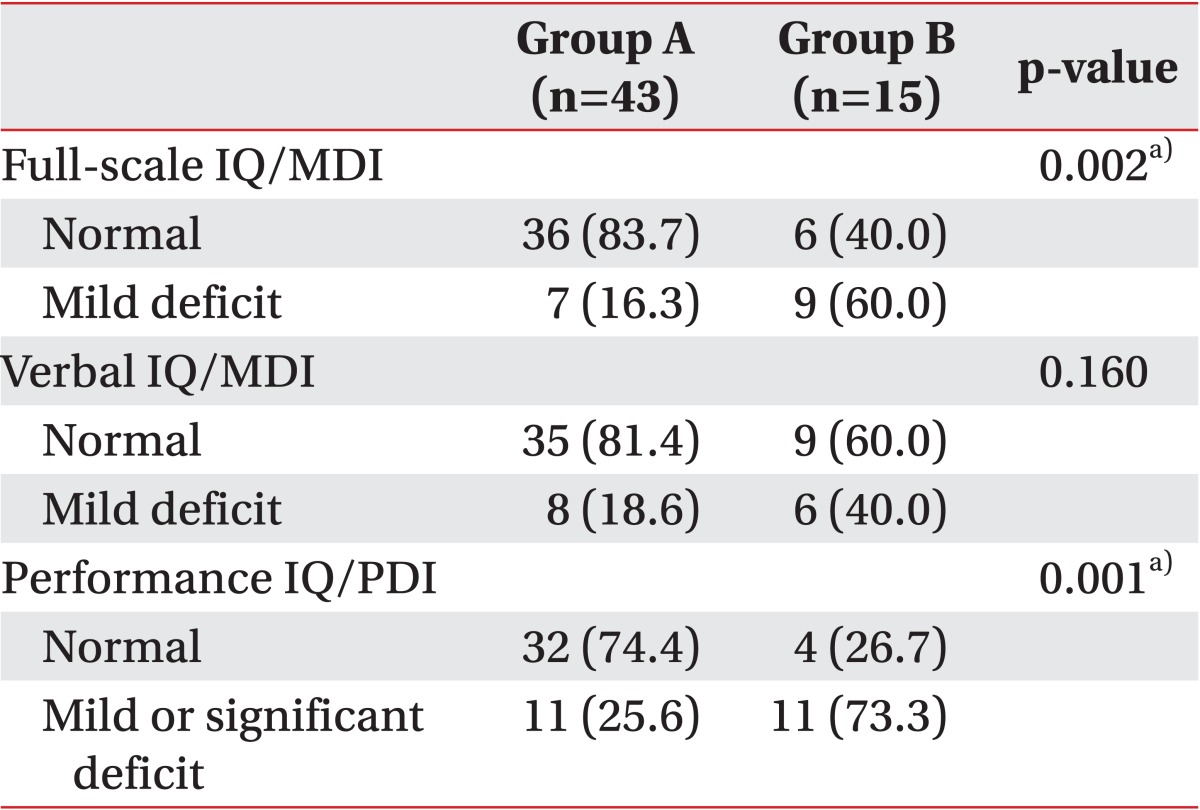
Thirty-six (83.7%) children in group A and six (40.0%) children in group B had normal cognition based on the full-scale IQ determined by K-WPPSI-R or K-BSID-II. The rate of cognitive deficits was significantly higher in group B than in group A (Table 2).
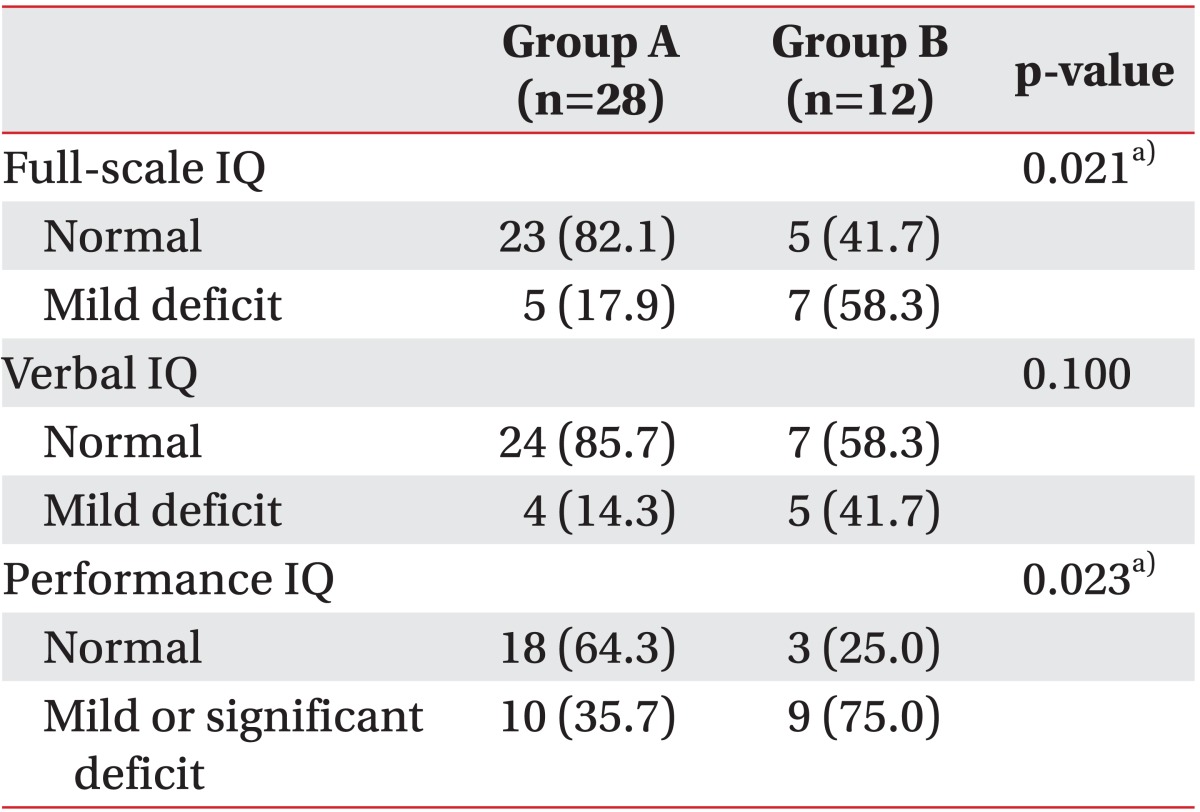
The K-WPPSI-R was administered to 28 children in group A and 12 children in group B. The full-scale IQ and performance IQ determined by the K-WPPSI-R were significantly higher in group A (96.4±12.8 and 89.9±12.0, respectively) than in group B (85.6±12.1 and 78.4±8.8, respectively), but there was no significant difference in verbal IQ between the groups (group A, 103.3±14.3; group B, 96.3±15.8). Significant deficits in performance skills (performance IQ<70) were noted in one child in group A and two children in group B, but no child in either group had a significant deficit in verbal skills (verbal IQ<70). Based on the full-scale IQ determined by the K-WPPSI-R, the rate of mild cognitive defects was higher in group B than in group A. The rates of mild or significant deficits in performance skills (performance IQ<85) were also significantly higher in group B than in group A (Table 3).
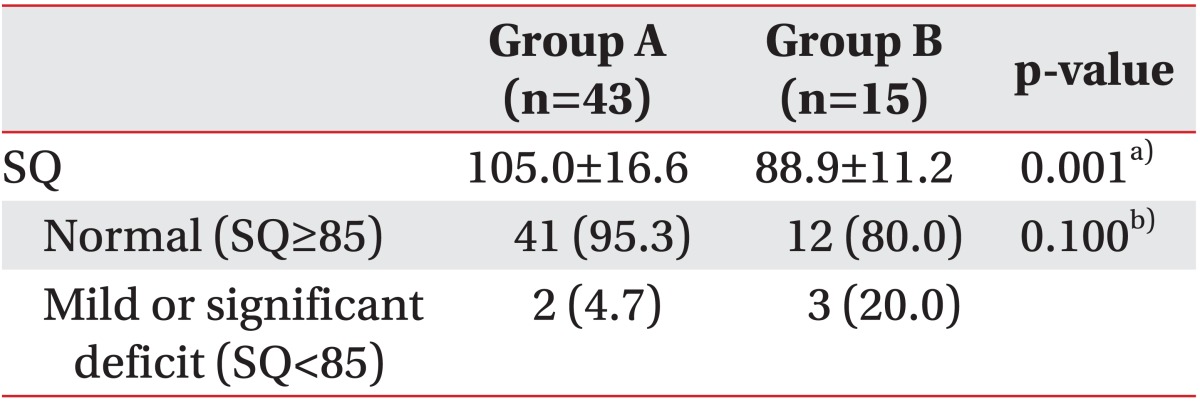
The total mean SQ was significantly higher in the children in group A (105.0±16.6) than in the children in group B (88.9±11.2). Significant deficits in social adaptive functioning (SQ<70) were noted in two children (4.7%) in group A and one child (6.7%) in group B. A mild deficit (70≤ SQ<85) was noted in two children (13.3%) in group B, but in no one from group A. The rates of mild or significant deficits in social adaptive functioning did not differ significantly between the two groups (Table 4).
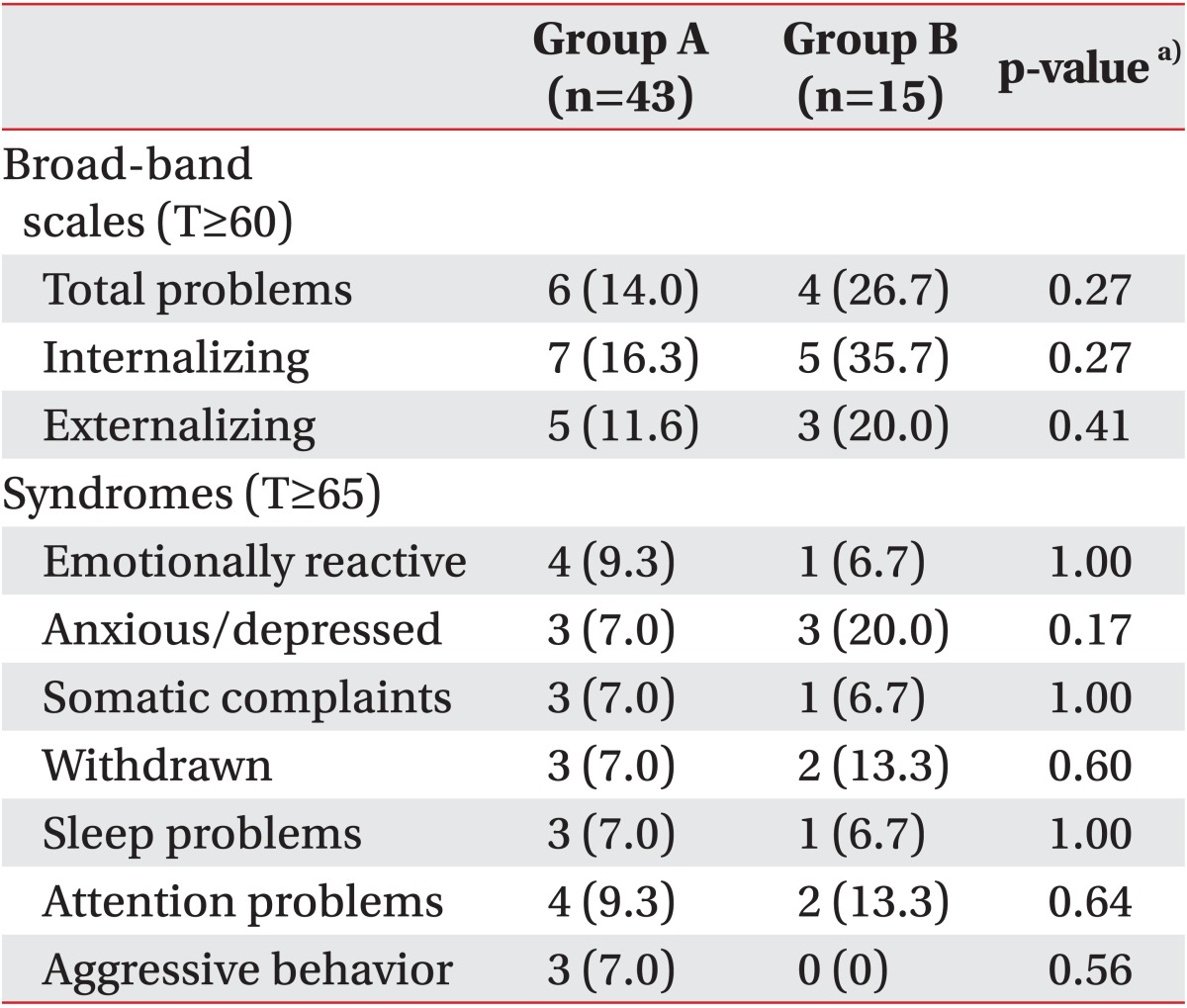
The total scores of the Korean version of the CBCL and the internalizing and externalizing behaviors did not differ significantly between the two groups. Abnormal behaviors based on the total score (T-score≥60) were noted in 6 children (14.0%) in group A and 4 children (26.7%) in group B. Abnormal internalization behavior problems were noted in 7 children (16.3%) in group A and 5 children (35.7%) in group B, and externalization behavior problems were noted in 5 children (11.6%) in group A and 3 children (20.0%) in group B.
Abnormal behaviors according to the seven subscales of CBCL 1.5-5 (T-score≥65) were noted in each group. The frequencies of these abnormal behaviors did not differ significantly between the two groups.
Emotionally reactive and attention problems were the most common abnormal behaviors in children in group A, whereas anxiety/depression was the most common abnormal behavior in children in group B (Table 5).
Four children in group A and one child in group B had CPRS scores above 16, suggesting attention and hyperactivity problems. One child in group A had a CARS score above 30, suggesting autistic behavior. Significant speech delays in both speech comprehension and expression were noted in only one child in group B. Mild speech developmental delays were noted in two children in group A but were not detected in group B. Speech development delay did not show significant differences between two groups.
The results of our study demonstrated that substantial number of the children without major NDI early in life had mild deficits in cognition when they were assessed later on. According to the study of Leversen et al. [24], of the extremely preterm children who had normal motor and mental development at 2 years of age, 31% had IQ <85 when assessed at age 5. In our study, 27.5% of our subjects had IQ or MDI <85, which are comparable with levels for children. In previous studies, the limited value of the predictive values of mental capacities in early childhood has been repeatedly demonstrated, especially preterm infants without major NDI [62425]. On the other hand, previous reports demonstrated lower mean scores than those for full-term children on various cognitive functions such as the Stanford-Binet intelligence scales, the visual perception test, visual motor integration tests, the sustained attention test, and the picture vocabulary test in preterm preschool children between 3 and 5 years of age with normal intellectual abilities and without other major NDI at 2 or 3 years of age [2627]. Another report demonstrated that the rates of problems in multiple domains such as motor skills, socio-emotional adjustment, learning skills and general cognition increased from 47% at the age of 4 years to 60% at the age between 6 and 9 years in very preterm children [7]. The results of previous studies provide evidence of the need for close follow-up for many years even in the children without major NDI in order to identify the children who are at risk and provide early intervention as they grow. The results of our study also support this point of view.
The evaluation of motor performance in preterm infants is important because motor development may affect the child's ability to explore his/her environment, which in turn may result in later cognitive developmental and behavioral problems [28]. AOW is frequently used as an indicator of the progress of motor development in early life. According to the literature [2930], the mean AOW ranges from 11 to 14.5 months. In our study, the children were divided into two groups based on whether their AOW was before or after 15 months to allow us to determine whether there were any differences in various domains of development between the groups.
The higher rates of these problems in children in the late walker group than in those in the early walker group support the previous notion that early motor performance plays an important role in the cognitive development of these children. Further study is needed to investigate whether late walking can be a good predictor of these problems, which can be identified early in children who are free of major NDI. In addition, our study revealed that performance skills were challenged more than verbal skills in these children. Luoma et al. [31] documented that preterm children tended to have lower performance IQ five times more often than did full-term children, and the tendency became even stronger when children with major neurological disabilities were excluded. In the literature, children who were born preterm and whose IQs are in the average range have repeatedly been found to have problems in visual perception, visual-motor skills, and visuospatial skills [2732]. The results of our study are consistent with these suggestions from previous studies. The lower performance IQ scores and the higher rates of mild or significant deficits in performance skills in group B suggest that performance skills are more problematic in late walkers, even among children who were free of major NDI early in life.
Adaptive behavior is defined as "the collection of conceptual, social and practical skills that have been learned in order to function in everyday life," and overall adaptive behavior is important for living [833]. It is now considered essential to measure the adaptive skills that present in early childhood during assessments of young children. Measuring adaptive skills, including SMS, allows for assessing a child's level of performance in everyday activities. What a child "does do" (performance) in his or her real life is influenced by the interplay between impairments and activity limitations, by personal factors, and by environmental factors. In a previous study, premature infants who were free of physical or mental impairments had significantly lower scores for overall adaptive behaviors than did full-term infants [8]. In that study, a measurable effect of preterm birth alone on adaptive functioning was demonstrated, and participation in everyday life and determining the limitations on a child's ability to perform the tasks of daily living were found to be important for children who were born preterm. However, the rates of mild or significant deficits in adaptive function were not described in that study. As far as we know, there is still a paucity of published data that describe the risks of mild or significant deficits in social adaptive functioning in children who were born preterm without major NDI in early life. Our study revealed mild or significant deficits in social adaptive functioning in both early and late walkers, although SQ scores were significantly lower in late walkers than in early walkers. These findings suggest that preterm infants without major NDI early in life should be assessed further regarding the development of social adaptive functioning. In addition, the social adaptive functional limitations of these children could lead to poorer educational attainments and reduced social functioning, so early interventions that allow these children to develop more complex skills are essential for successful adult living [8]. Additional studies about the rates and early predictors of social adaptive functional impairment are needed in order to minimize the untoward consequences of social adaptive functional impairments in children who were born preterm without major NDI.
It is well-known that preterm infants are more susceptible to behavioral problems than are full-term infants [6]. In a previous study, very-preterm-born children exhibited higher rates of behavioral problems early in development at the age of 2 years [9]. The CBCL is the most commonly used measure for assessing behavioral problems in childhood. The behavioral problems assessed by the CBCL are strongly associated with problems in school and social competence [34]. In a previous study [35], 23.3% of preterm infants in a brain-sparing group had behavioral problems according to the CBCL, and there were no significant differences in behavioral problems between the groups with and without brain sparing. In addition, attention problems were the most common behavioral problem in that study. Our study revealed rates of behavioral problems that were comparable with those of the previous study, and it also revealed that attention problems were the most common behavioral problem. In addition, 5 children had significant attention/hyperactivity problems suggesting ADHD, based on the CPRS. According to a previous study, cognitive impairment is a strong predictor of ADHD symptoms in children who were born extremely preterm with minor NDI such as freely ambulatory CP, mild motor problems, mild cognitive problems, mild visual impairments, and mild hearing impairments [36]. In our study, the relationship between mild cognitive deficits and ADHD symptoms was not investigated because of the small sample size. Further study is needed to delineate the relationship between cognition level and ADHD symptoms in children who were free of identifiable physical or mental impairments early in life.
In a recently published study [37], preterm children displayed more autistic behavior in early childhood than did the general population. In our study, one child in group A had autistic behavior. These findings suggest that it will be important to monitor behavioral problems, including autistic behavior, even in children who are free of major NDI early in life.
The data on the association between prematurity and speech disorders are not conclusive. Language is particularly susceptible to change depending on the child's socio-economic and environmental background, and thus, careful consideration of these factors is essential whenever this developmental domain is assessed [4]. Many language functions are reasonably normal in low-birth-weight children; however, more complex verbal processes such as understanding syntax, abstract verbal skills, and the mean length of utterance have been found to be deficient in preterm infants compared with their normal-birth-weight peers [4]. Even if the majority of our subjects seemed to be free of major speech disabilities, some children have subtle or significant delays in speech development. The rates of speech development problems were not different between the two groups in our study. The interplay of biological and environmental factors is critical for speech development, so long-term monitoring of speech development and more complex verbal processing problems is needed with controls for these environmental factors.
Children who were born preterm are at high risk for minor neurodevelopmental problems such as mild cognitive deficits and behavioral, academic performance, and adaptive functioning problems compared with full-term infants. These minor problems are more responsive to early interventions, and thus, the early detection of these problems is essential for minimizing future sequelae [38]. In contrast to the major NDI that can be identified easily early in life, minor or subtle impairments cannot be easily detected early; these subtle problems tend to become more obvious as the child grows older in response to increased performance demands [39]. A recently published study documented the importance of long-term monitoring beyond neuromotor and cognitive functioning to language and behavioral adjustment during the preschool period [7]. Another report highlighted the limited value of pediatric assessments at 2 years in predicting cognitive and motor function in later years and concluded that follow-up for many years for extremely preterm children is needed to reliably identify special needs [40]. Even in children who are free of identifiable physical or mental disabilities early in life, long-term monitoring for developmental problems in multiple domains such as cognition, behavior, adaptive functioning, and speech is considered essential in children born preterm [626]. The results of our study also support the importance of periodic assessment and long-term monitoring in preterm children, even if these children were free of identifiable physical or mental disabilities early in life.
The strength of our study is that we investigated developmental outcomes in various domains in children who were free of identifiable physical or mental disabilities early in life based on AOW, which is a parameter that can be monitored easily. Even in children without major NDI, motor performance is important for the development of cognition and social adaptive functioning. However, our results should be interpreted cautiously because of the small sample size in group B.
In addition, some of the children without major NDI at 2 years were lost during follow-up and thus did not receive a neuropsychological evaluation after 3 years of age. There may be various reasons for these dropouts. In general, we think that the children with good neuropsychological function may be more often lost for further assessment. Therefore, it may be likely that the results of our study overestimate the rate of neuropsychological impairments. However, we do not think that the dropouts had a large influence on the conclusion of our study because our study's aim was to determine whether there were any differences in those impairments between early and later walkers.
In addition, many factors affect cognition, social adaptive functioning, behavior, and speech development, such as socio-economic status, gestational age, neonatal morbidity, parental attitudes, etc. Until now, no good predictors have been found that can identify these subtle problems early. Therefore, additional efforts are needed to delineate a good predictor that can be identified early that considers or controls for many other confounding factors.
In conclusion, our study revealed that some of the children without major NDI at the age of 2 years had problems in cognition, social adaptive functioning, emotions, and behavior. The risks of cognitive deficits were greater in late walkers than in early walkers. The full-scale IQ and performance IQ were significantly lower in late walkers than in early walkers. SQs were significantly lower in late walkers than in early walkers, but there were no significant differences in the rates of mild or significant deficits in social adaptive functioning between the two groups. In addition, some children had significant behavioral problems including ADHD symptoms and autistic behavior; the abnormal behaviors were comparable in both groups. These findings support the importance of periodic assessments of multiple developmental domains in order to minimize future developmental sequelae by implementing early interventions for any developmental problems detected.
References
1. Delobel-Ayoub M, Arnaud C, White-Koning M, Casper C, Pierrat V, Garel M, et al. Behavioral problems and cognitive performance at 5 years of age after very preterm birth: the EPIPAGE Study. Pediatrics. 2009; 123:1485–1492. PMID: 19482758.

2. Stephens BE, Vohr BR. Neurodevelopmental outcome of the premature infant. Pediatr Clin North Am. 2009; 56:631–646. PMID: 19501696.

3. Moreira RS, Magalhaes LC, Alves CR. Effect of preterm birth on motor development, behavior, and school performance of school-age children: a systematic review. J Pediatr (Rio J). 2014; 90:119–134. PMID: 24370176.

4. Aylward GP. Cognitive and neuropsychological outcomes: more than IQ scores. Ment Retard Dev Disabil Res Rev. 2002; 8:234–240. PMID: 12454899.

5. van Baar AL, van Wassenaer AG, Briet JM, Dekker FW, Kok JH. Very preterm birth is associated with disabilities in multiple developmental domains. J Pediatr Psychol. 2005; 30:247–255. PMID: 15784921.

6. de Kleine MJ, den Ouden AL, Kollee LA, Nijhuis-van der Sanden MW, Sondaar M, van Kessel-Feddema BJ, et al. Development and evaluation of a follow up assessment of preterm infants at 5 years of age. Arch Dis Child. 2003; 88:870–875. PMID: 14500304.

7. Pritchard VE, Bora S, Austin NC, Levin KJ, Woodward LJ. Identifying very preterm children at educational risk using a school readiness framework. Pediatrics. 2014; 134:e825–e832. PMID: 25113296.

8. Killeen H, Shiel A, Law M, Segurado R, O'Donovan D. The impact of preterm birth on participation in childhood occupation. Eur J Pediatr. 2015; 174:299–306. PMID: 25119818.

9. Spittle AJ, Treyvaud K, Doyle LW, Roberts G, Lee KJ, Inder TE, et al. Early emergence of behavior and social-emotional problems in very preterm infants. J Am Acad Child Adolesc Psychiatry. 2009; 48:909–918. PMID: 19633579.

10. Vincer MJ, Cake H, Graven M, Dodds L, McHugh S, Fraboni T. A population-based study to determine the performance of the Cognitive Adaptive Test/Clinical Linguistic and Auditory Milestone Scale to Predict the Mental Developmental Index at 18 months on the Bayley Scales of Infant Development-II in very preterm infants. Pediatrics. 2005; 116:e864–e867. PMID: 16263973.

11. Johnson S, Moore T, Marlow N. Using the Bayley-III to assess neurodevelopmental delay: which cut-off should be used? Pediatr Res. 2014; 75:670–674. PMID: 24492622.

12. Lowe JR, Erickson SJ, Schrader R, Duncan AF. Comparison of the Bayley II Mental Developmental Index and the Bayley III Cognitive Scale: are we measuring the same thing? Acta Paediatr. 2012; 101:e55–e58. PMID: 22054168.

13. Kim SK, Kim OK. Social Maturity Scale manual. Seoul: Chunangjeokseong Publishing;1995.
14. Achenbach TM, Edelbrock C. Manual for the child behavior checklist and revised child behavior profiles. Burlington: University of Vermont;1983.
15. Oh KJ, Lee H, Hong KE, Ha EH. Korean version of Child Behavior Checklist (K-CBCL). Seoul: Chunangjeokseong Publishing;1997.
16. Kim YA, Lee J, Moon SJ, Kim YJ, Oh KJ. Standardization study for the Korean version of the child behavior checklist for ages 1.5-5. Korean J Clin Psychol. 2009; 28:117–136.
17. Conners CK. The Conners rating scales. In : Maruish M, editor. The use of psychological testing for treatment planning and outcome assessment. Hillsdale: Lawrence Erlbaum Associates;1994. p. 550–578.
18. Conners CK. Symptom patterns in hyperkinetic, neurotic, and normal children. Child Dev. 1970; 41:667–682.

19. Oh KJ, Lee HR. Assessment of ADHD with abbreviated Conners rating scale. Korean J Clin Psychol. 1989; 8:135–142.
20. Schopler E, Reichler RJ, Renner BR. The Childhood Autism Rating Scale (CARS): for diagnostic screening and classification of autism. New York: Irvington;1986.
21. Kim TR, Park RG. Korean version of Childhood Autism Rating Scale. Seoul: Special Education Publishing;1996.
22. Kim YT. Content and reliability analyses of the Sequenced Language Scale for Infants (SELSI). Korean J Commun Disord. 2002; 7:1–23.
23. Kim YT, Sung TJ, Lee YK. Preschool receptive-expressive language scale (PRES). Seoul: Special Education Publishing;2003.
24. Leversen KT, Sommerfelt K, Ronnestad A, Kaaresen PI, Farstad T, Skranes J, et al. Prediction of neurodevelopmental and sensory outcome at 5 years in Norwegian children born extremely preterm. Pediatrics. 2011; 127:e630–e638. PMID: 21321031.

25. Marlow N, Wolke D, Bracewell MA, Samara M. EPICure Study Group. Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med. 2005; 352:9–19. PMID: 15635108.

26. Caravale B, Tozzi C, Albino G, Vicari S. Cognitive development in low risk preterm infants at 3-4 years of life. Arch Dis Child Fetal Neonatal Ed. 2005; 90:F474–F479. PMID: 15956096.

27. Caravale B, Mirante N, Vagnoni C, Vicari S. Change in cognitive abilities over time during preschool age in low risk preterm children. Early Hum Dev. 2012; 88:363–367. PMID: 22051526.

28. Van Hus JW, Jeukens-Visser M, Koldewijn K, Geldof CJ, Kok JH, Nollet F, et al. Sustained developmental effects of the infant behavioral assessment and intervention program in very low birth weight infants at 5.5 years corrected age. J Pediatr. 2013; 162:1112–1119. PMID: 23312690.

29. Siegel AC, Burton RV. Effects of baby walkers on motor and mental development in human infants. J Dev Behav Pediatr. 1999; 20:355–361. PMID: 10533994.

30. Stanitski DF, Nietert PJ, Stanitski CL, Nadjarian RK, Barfield W. Relationship of factors affecting age of onset of independent ambulation. J Pediatr Orthop. 2000; 20:686–688. PMID: 11008754.

31. Luoma L, Herrgard E, Martikainen A. Neuropsychological analysis of the visuomotor problems in children born preterm at < or = 32 weeks of gestation: a 5-year prospective follow-up. Dev Med Child Neurol. 1998; 40:21–30. PMID: 9459213.
32. Butcher PR, Bouma A, Stremmelaar EF, Bos AF, Smithson M, Van Braeckel KN. Visuospatial perception in children born preterm with no major neurological disorders. Neuropsychology. 2012; 26:723–734. PMID: 22905735.

33. Verdugo MA, Arias B, Ibanez A, Schalock RL. Adaptation and psychometric properties of the Spanish version of the Supports Intensity Scale (SIS). Am J Intellect Dev Disabil. 2010; 115:496–503. PMID: 20946002.

34. Purdy IB, Smith L, Wiley D, Badr L. A psychoneuroimmunologic examination of cumulative perinatal steroid exposures and preterm infant behavioral follow-up. Biol Res Nurs. 2013; 15:86–95. PMID: 21900308.

35. van den Broek AJ, Kok JH, Houtzager BA, Scherjon SA. Behavioural problems at the age of eleven years in preterm-born children with or without fetal brain sparing: a prospective cohort study. Early Hum Dev. 2010; 86:379–384. PMID: 20554130.

36. Elgen SK, Sommerfelt K, Leversen KT, Markestad T. Minor neurodevelopmental impairments are associated with increased occurrence of ADHD symptoms in children born extremely preterm. Eur Child Adolesc Psychiatry. 2015; 24:463–470. PMID: 25304291.

37. Wong HS, Huertas-Ceballos A, Cowan FM, Modi N. Medicines for Neonates Investigator Group. Evaluation of early childhood social-communication difficulties in children born preterm using the Quantitative Checklist for Autism in Toddlers. J Pediatr. 2014; 164:26–33.e1. PMID: 23972644.
38. Frolek Clark GJ, Schlabach TL. Systematic review of occupational therapy interventions to improve cognitive development in children ages birth-5 years. Am J Occup Ther. 2013; 67:425–430. PMID: 23791317.

39. Curtis WJ, Lindeke LL, Georgieff MK, Nelson CA. Neurobehavioural functioning in neonatal intensive care unit graduates in late childhood and early adolescence. Brain. 2002; 125(Pt 7):1646–1659. PMID: 12077013.

40. Leversen KT, Sommerfelt K, Elgen IB, Eide GE, Irgens LM, Juliusson PB, et al. Prediction of outcome at 5 years from assessments at 2 years among extremely preterm children: a Norwegian national cohort study. Acta Paediatr. 2012; 101:264–270. PMID: 22026562.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download