INTRODUCTION
The upper esophageal sphincter (UES) is one of the important anatomical components that are associated with dysphagia in the swallowing process [
1]. In various pathological conditions including stroke, hypoxic brain injury, Parkinson's disease, poliomyelitis, amyotrophic lateral sclerosis, cerebral vasculitis, traumatic brain injury, and other brain lesions, lack of UES opening becomes a source of resistance to bolus flow from the pharynx to the esophagus [
2]. This causes complications like postswallow pharyngeal remnant, airway aspiration, and subsequent pneumonia, malnutrition, and dehydration [
34]. The most important muscle related to UES dysfunction is the cricopharyngeus muscle [
5], which is located between the lower pharynx and the upper esophagus, and participates in the formation of the UES and sends food down through the UES by harmonious relaxation and contraction [
6]. Cricopharyngeus muscle dysfunction (CPD) indicates impaired or uncoordinated UES relaxation or expansion [
7].
Thus far, treatment methods for CPD include mechanical balloon dilatation [
8], botulinum toxin injection [
9], and cricopharyngeal myotomy [
10]. Solt et al. [
8] and several other authors [
111213] have used dilatation techniques for UES relaxation. Solt et al. [
8] used balloon dilatation guided by endoscopy in five patients with primary CPD. The patients showed improvement in UES relaxation when compared to previous techniques, and the new technique was considered to be cost-effective and less invasive; however, the use of endoscopy tended to increase the cost and discomfort, or trauma in patients. Dou et al. [
11] achieved a positive result by placing a catheter balloon below the UES and pulling it in upward direction with simultaneous swallowing effort to prevent the balloon from riding up into the pharynx. However, this method was likely to cause mucosal injury as the balloon's movement was contrary to the physiologic direction [
12]; the authors sprayed antibiotics and steroids into the hypopharynx and the UES after the balloon pulling technique. Kim et al. [
13] performed videofluoroscopy guided balloon dilatation without using endoscopy as part of dysphagia rehabilitation, which was found to be safe, comfortable, and cost-effective. This method incorporated the idea of dilatation, but instead of keeping the balloon in the expanded state at the UES for some time, it mainly utilized iterative swallowing responses, which could be spontaneous, voluntary, or reflexive by irritation of the nerve plexus by the expanded balloon. Recently, Jung et al. [
14] reported cases of two patients, who were able to take oral feeding after application of technique suggested by Kim et al. [
13] in patients with UES dysfunction due to vagus nerve injury after a surgical intervention.
This study extended the research, previously conducted by Kim et al. [
13]. The effects of balloon swallowing training were assessed, however, some topics were left undiscovered for further investigations: for example, studies on the effect of balloon treatment according to the balloon size. We conducted a quantitative study to understand relationship between the size of the balloon that a patient could swallow during balloon swallowing rehabilitation and CPD severity or improvement in dysphagia after treatment. All experiments were performed using videofluoroscopy and swallowing of large balloons was evaluated in real time basis. The relationship was confirmed by measuring the maximum balloon diameter identified on videofluoroscopy and dysphagia parameters such as pharyngeal transit time and post-swallow pharyngeal remnant before and after the balloon treatment.
Go to :

MATERIALS AND METHODS
Subjects
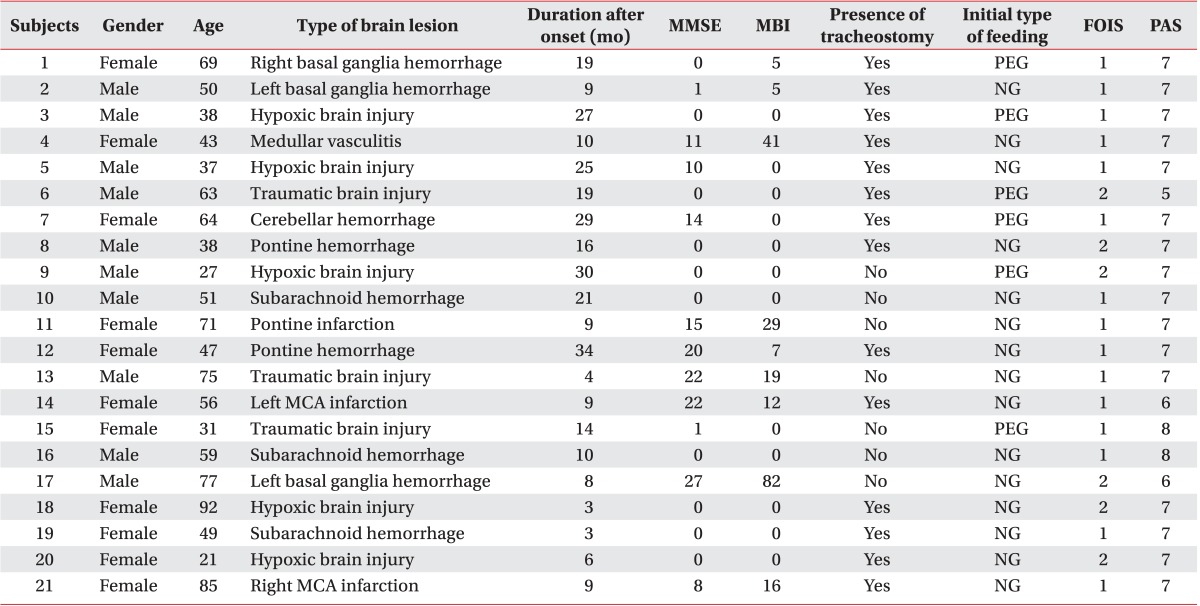
We performed a retrospective analysis of videofluoroscopic swallowing study (VFSS) data from January through December 2012 for inpatients in the Department of Physical Medicine and Rehabilitation, Myongji Hospital. Inclusion criteria were as follows. First, dysphagia was caused by brain lesions such as stroke, traumatic brain injury, brain tumor, hypoxic brain injury, and cerebral vasculitis. Second, VFSS and dysphagia rehabilitation in this hospital were conducted between three months and three years after the onset of disease. Third, CPD was diagnosed based on VFSS when post-swallow pharyngeal remnant after swallowing semisolid paste, was equal to or more than 40%, as stated in the previous study [
13]. Semisolid paste was prepared as a 2:1 volumetric mixture of dysphagia formula level 1 and contrast barium solution (375 g of barium sulfate powder, Solotop-HD provided by Taejoon Pharm Company, Ltd., Yongin, Korea, was mixed with 90 mL water for contrast solution). Data on patient characteristics, VFSS reports, medical history, previous treatment history, symptoms, and complications were extracted from medical records in the hospital. This study was approved by the Institutional Review Board of the hospital.
Balloon swallowing technique
The technique employed in the present study was similar to that used by Kim et al. [
13]. Videofluoroscopy was utilized to guide a 16-Fr Foley catheter that was to be inserted through the patient's nose or mouth, and it was placed in the pyriform sinus where the catheter balloon was inflated with contrast solution, which was visible on fluoroscopy. When the balloon stimulated the pharyngeal nerve plexus, swallowing reflex was induced and the balloon moved down into the esophagus through the UES. Patients with a well-maintained reflexive circuit would demonstrate increased reflex frequency and intense swallowing. It was also possible to instruct the patients to make intentional swallowing efforts. The balloon with contrast solution that entered the esophagus was deflated, pulled rostrally, re-positioned in the lower pharynx, and then re-inflated with contrast solution for the subsequent swallowing step.
Endoscopic evaluation of the pharynx
To determine whether there were any complications on the surface or mucosa of the contact areas after the treatment, the patient underwent transnasal endoscopic evaluation with a fiberoptic rhinolaryngoscope (ENF-GP portable fiberoptic rhinolaryngoscope provided by Olympus Medical Systems Corp., Tokyo, Japan). Vocal cord movement, laryngopharyngeal reflux, laryngeal sensation, and airway patency were also assessed.
Outcome measures
UES relaxation
Accurate size of the balloon in the pharynx was obtained by measuring the diameter of the balloon in a two-dimensional projection on videofluoroscopy screen. When a balloon is swallowed through the UES, its diameter decreases slightly. The point of maximum decrease was the moment when there was a maximum increase in the resistance of the UES. The two-dimensional diameter of the balloon at that moment was measured in mm, and compared to the annotated 100 Korean won coin (23 mm in diameter) attached to the patient's neck in order to estimate the UES opening size during balloon treatment (
Fig. 1).
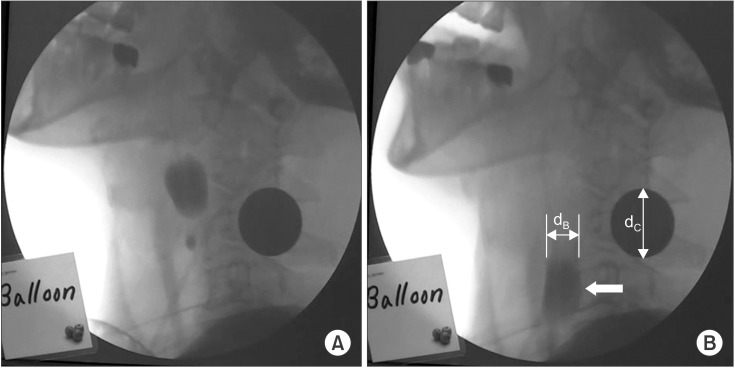 | Fig. 1A video camera recorded the videofluoroscopic swallowing study at a speed of 30 frames per second. (A) shows the moment when the balloon starts to move down after laryngeal elevation during swallowing. (B) is the moment when the balloon (thick white arrow) passes through the upper esophageal sphincter (UES), which is approximately located at the level of the 4th and 5th cervical vertebrae. The cross-sectional diameter (dB) of the balloon at this moment divided by the longest diameter (dC) of the coin multiplied by 23 mm is the approximate balloon size at the UES.
|
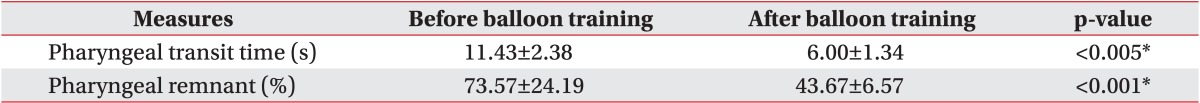
Dysphagia measures
We evaluated the pharyngeal transit time and postswallow pharyngeal remnant on VFSS, which showed significant improvement after balloon swallowing training among several dysphagia measures as reported earlier [
13]. Pharyngeal transit time is the time taken by food to pass from the pharyngeal fornix into the UES during swallowing action. Pharyngeal remnant on VFSS corresponds to the area of two-dimensional projection of food retained in the pharyngeal space after a swallow process. The area can be calculated with the help of a coin attached to the patient's neck as a reference size. Video recordings were obtained for further analysis. Two VFSS's were performed before and after iterative balloon swallowing treatments, yielding two values of pharyngeal transit time measured in seconds and two values of pharyngeal remnant measured in percentage (%). These two dysphagia measures were converted into continuous variables in order to represent changes before and after the balloon treatment and to determine regression relationships of improvement after the treatment with respect to UES relaxation expressed as balloon diameter at the UES: using the measurements for pharyngeal transit time and pharyngeal remnant before and after the balloon treatment, we calculated the ratio of two measurements, i.e., post-treatment values divided by pretreatment values and plotted them in accordance with maximum balloon diameters at the UES together with their linear regression equations.
Procedure
Patients in whom dysphagia evaluation was necessary received the VFSS, and some of them diagnosed with CPD were further treated with a catheter balloon: a 16-Fr Foley catheter was located in the lower pharynx through the nose or mouth and then filled with increasing quantities of 0, 1, 2, 3, 4, and 5 mL of contrast solution until the possible maximum size of the balloon that a patient could swallow was determined. After the maximum balloon size was determined, the iterative balloon swallowing treatment was performed for three or five minutes (about 20 swallows). Subsequently, the second VFSS was performed. The maximum balloon size, i.e., the maximum UES opening and the measured values of pharyngeal transit time and pharyngeal remnant obtained from two VFSS's were analyzed by statistical methods.
Statistical analysis
All statistical analyses were performed with SPSS ver. 18.0 (IBM Corporation, Armonk, New York, USA). Statistical significance was confirmed with the paired t-test for comparison of results before and after the balloon treatment. Relationships between UES relaxation and dysphagia measures were evaluated with linear regression analysis. A p-value<0.05 was considered to indicate statistical significance.
Go to :

DISCUSSION
Most of the patients with severe dysphagia depend on tube feeding, which in itself limits the way to practice oropharyngeal swallowing as well as reduces the opportunity to swallow real food. Kim et al. [
13] inserted a 16-Fr Foley catheter balloon into the pharynx to induce swallowing action and they could easily adjust the volume of swallowed material for performing quantitative treatment and evaluation. Videofluoroscopy not only provided them with a method that could show balloon inflation, size, and swallowing, but it also suggested a real time balloon swallowing technique. The authors reported the effectiveness of the balloon swallowing treatment. We conducted this study using the pharyngeal transit time and pharyngeal remnant as outcome measures since Kim et al. had confirmed the statistical significance and obtained the same results after the balloon treatment (
Table 2).
Table 1 shows that all 21 patients diagnosed with CPD, i.e., pharyngeal remnant >40%, received tube feeding, and thus there seemed to be no other way to practice swallowing without the risk of aspiration than swallowing a balloon. In most of the patients, reflexive or spontaneous swallowing was performed rather than voluntary swallowing due to severely impaired cognition. It is proposed that the balloon treatment presented in this study can be a very useful method that could enable a patient with cognitive deficit to swallow without the risk of aspiration and subsequent complications.
Brain lesions such as stroke cause paralysis of muscles with degradation in motor skills and coordination ability. Paralysis of the cricopharyngeus muscle causes impairments of relaxation and contraction of the UES such that food cannot reach the esophagus but remains in the pharyngeal space [
2]. An adequate UES opening is necessary to send food down to the esophagus in the swallowing process. Shaker et al. showed that dysphagia caused by abnormal UES opening was improved via a suprahyoid muscle strengthening exercise program [
17]. Isotonic and isokinetic contraction of the anterior neck muscles involved in UES opening by physical exercise improved UES opening. A six-week exercise program resulted in more than ten times reduction in the area of pharyngeal remnant on VFSS.
A training program in which a material like a balloon catheter passes through the UES repeatedly will increase the range of motion of the cricopharyngeus muscle, reduce the impedance of the UES, and improve UES relaxation. Omari et al. [
18] reported a manometry study, which revealed that the UES impedance is related to sphincter opening diameter. Improvement in this area enlarges the sphincter opening, helps swallowing function, and reduces the amount of food retained in the pharyngeal space. Pharyngeal remnant can be affected most directly among dysphagia outcome measures. Therefore, treatment with repeated swallowing of a catheter balloon in patients with severe dysphagia, who rarely perform the swallowing process can be a good dynamic treatment option, which may enable the patients to recall and practice the swallowing mechanism, ultimately leading to improvement in dysphagia.
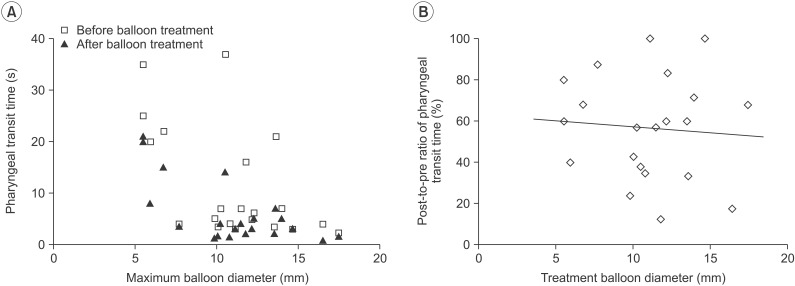
A principal feature of this study is that we could not only measure but also change the size of a balloon in real time. The diameter obtained by inflating the balloon of a 16-Fr Foley catheter is quite large. For example, inflating the balloon with 5 mL liquid provides a diameter of 21 mm. We can increase or decrease the balloon size in real time depending on the patient's ability. The larger is the balloon utilized, the more is the relaxation of the UES as well as the longer is the duration of its opening, and then more quantity of food and less amount of remnant can be expected during swallowing. Lin et al. [
19] reported that the UES relaxation duration increases when the bolus volume increases, in a study in which healthy subjects were fed liquid, thick liquid, and semisolid food with the help of high-resolution manometry. Therefore, it is regarded as an advantage spatially and temporally to induce large swallowing with a large volume of balloon. This study produced a result with statistical significance, which indicated that the degree of reduction in pharyngeal remnant was positively correlated with balloon size used in the balloon treatment (
Fig. 3B). Pharyngeal remnant can be a useful indicator that describes UES relaxation.
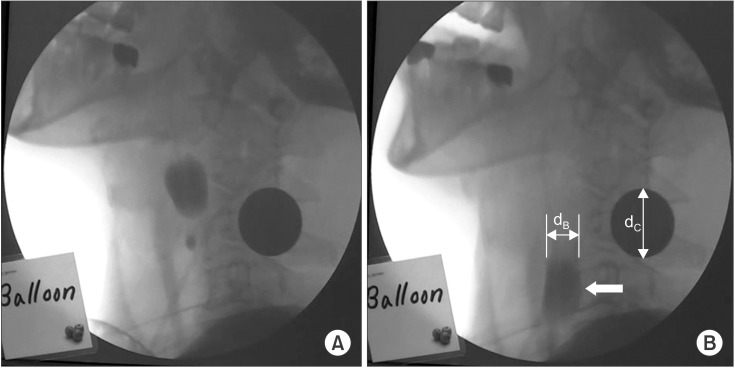
On the other hand, the pharyngeal transit time is relatively insensitive to changes in the UES because it is more associated with the movement of oropharyngeal muscles, i.e., bolus transfer or peristalsis than with UES relaxation. Iterative swallowing training for three to five minutes is expected to modify pharyngeal movement causing reduction in the pharyngeal transit time, but it will be difficult to induce any significant association between pharyngeal movement and balloon size, i.e., the extent of UES opening. In this study, the pharyngeal transit time tended to reduce in proportion to the maximum size of the balloon that a patient could swallow (
Fig. 2A) and it improved after the balloon treatment (
Table 2), but the relative improvement in the pharyngeal transit time after the balloon treatment was not associated with treatment balloon size as expected (
Fig. 2B).
In the treatment with endoscopy guided balloon dilatation, a dilated cylindrical balloon is inserted across the UES for a certain amount of time to induce a state of relaxation or a partial tear of the cricopharyngeus muscle with an ultimate goal of improving relaxation of the UES when the patient is on a real diet [
2021]. This kind of treatment is a static method that keeps a balloon at the UES in order to decrease UES resting pressure and is thus recommended in patients with high UES tone. However, excessive reduction of the UES tone will increase the incidence of problems such as reflux complications. Artificial mechanical dilatation of the UES may cause mucosal injury, perforation, or pain. Dou et al. [
11] attempted to pull a catheter balloon located in the upper esophagus towards the pharynx with simultaneous intentional swallowing effort to prevent the balloon from riding up into the pharynx. In this method, the movement of the balloon and shear force applied to the mucosa is in the direction opposite to natural swallowing, and thus the likelihood of complications such as mucosal injury, inflammation, or pain and the risk of reflux are likely to increase [
12]. In addition, this treatment requires that the patient should have sufficient cognitive function so that he or she can perform the voluntary swallowing action. In our study, which was different from that by Dou et al. [
11], the patient was trained to swallow a balloon in the natural swallowing direction so that there was very little likelihood of complications, such as mucosal injury, reflux, and pain, and compliance of patients increased accordingly. Fiberoptic transnasal endoscopic evaluation of the pharynolarynx after the balloon treatment did not show any mechanical complication; the contrary was rather observed in some cases. The initially observed laryngopharyngeal reflux was improved at the follow-up endoscopy possibly because the patients were able to swallow saliva and showed improved reflux signs. This balloon swallowing treatment allows the patients with impaired cognition, who cannot perform voluntary swallowing and the patients with severe dysphagia, who cannot practice with real food due to the risk of aspiration to participate in the dysphagia rehabilitation program along with reflexive or spontaneous swallowing in the patients with impaired cognition. It will also be a useful training method without the risk of aspiration for the patients, who have difficulty in achieving harmonious pharyngeal movement, failure of proper relaxation and coordination, or hypotensive UES tone.
A limitation of this study was that manometry data was not included to obtain data on pharyngeal peristalsis and UES relaxation. We applied the balloon treatment for CPD observed on VFSS without having correct information regarding whether the UES tone was increased or decreased. It might also be possible to verify the effects of the balloon treatment and physiological effects more quantitatively if the UES relaxation duration can be measured. However, if we apply the iterative balloon swallowing technique used in this study rather than the previous static UES dilatation techniques [
82021], it can be a more efficient approach for treating disorders with decreased pharyngeal and UES motility and those with impaired rhythmic coordination. Performing a post-treatment VFSS immediately after videofluoroscopy guided balloon treatment was an easy way to assess the effect of the balloon treatment in the absence of other confounding factors, but there was a limitation in studying the effects after long-term training. You et al. [
22] studied oroesophageal tube swallowing by comparing the condition before and after treatment for 25 or 26 days. The authors found a significant change in laryngeal elevation and oral transit time as well as in pharyngeal remnant. We studied the short-term effects of the treatment as the first VFSS during hospitalization and balloon treatment at that time for each patient was included in the study. If long-term daily training is performed, measures other than pharyngeal transit time and pharyngeal remnant may show meaningful changes. This study could not identify any significant change in laryngeal elevation, swallowing reflex frequency, etc., after the three to five minute balloon treatment although detailed data are not presented here; however, significant changes could be observed after long-term training. Meanwhile, the long-term daily training is recommended to use a blind approach that can avoid radiation exposure during videofluoroscopy. The blind approach can be performed without any difficulty in reality, which could be discussed in the future. In terms of research continuity in line with the previous study by Kim et al. [
13], the definition of CPD as pharyngeal remnant >40% might be too restrictive. Only 7.4% of the cases that underwent VFSS at our institute were diagnosed with CPD, which represents a minor group consisting of a small number of patients. However, strict criteria might be able to strengthen understanding of the balloon treatment by increasing its specificity.
In conclusion, this study reports that the balloon treatment enabled the patients with dysphagia after brain lesions such as stroke to practice swallowing without the risk of aspiration and that a large volume of balloon was advantageous for improving UES relaxation. The maximum size of the balloon that a patient can swallow is approximately equal to the maximum possible UES opening when he or she swallows a food material. A sensitive measure such as pharyngeal remnant showed a statistically significant relationship with treatment balloon size. Thus, it is necessary that a dysphagia rehabilitation program that incorporates the balloon swallowing treatment should gain popularity.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download