Abstract
Epidural steroid injections (ESI) are a common treatment for back pain management. ESI-related complications have increased with the growing number of procedures. We report a case of cervical meningomyelitis followed by multiple lumbar ESI. A 60-year-old male with diabetes mellitus presented to our hospital with severe neck pain. He had a history of multiple lumbar injections from a local pain clinic. After admission, high fever and elevated inflammatory values were detected. L-spine magnetic resonance imaging (MRI) revealed hematoma in the S1 epidural space. Antibiotic treatment began under the diagnosis of a lumbar epidural abscess. Despite the treatment, he started to complain of weakness in both lower extremities. Three days later, the weakness progressed to both upper extremities. C-spine MRI revealed cervical leptomeningeal enhancement in the medulla oblongata and cervical spinal cord. Removal of the epidural abscess was performed, but there was no neurological improvement.
Low back pain (LBP) is a major contributor of lifetime disabilities. The annual incidence of LBP continues to rise [1]. The pathophysiology of LBP is associated with inflammatory mediators including tumor necrosis factor and interleukins [2]. Epidural steroid injection (ESI) targeting of these inflammatory mediators can improve pain for 6 weeks or longer [3].
The number of lumbar ESI procedures used in the management of LBP is increasing annually [1]. Reported complications of lumbar ESI include hematoma, epidural abscess, and meningitis. These complications are more likely to occur in patients who are immunocompromised or with an underlying history of diabetes mellitus (DM) or renal failure [4]. There has been no report of cervical meningomyelitis after lumbar ESI. The current report describes a case of cervical meningomyelitis following lumbar ESI.
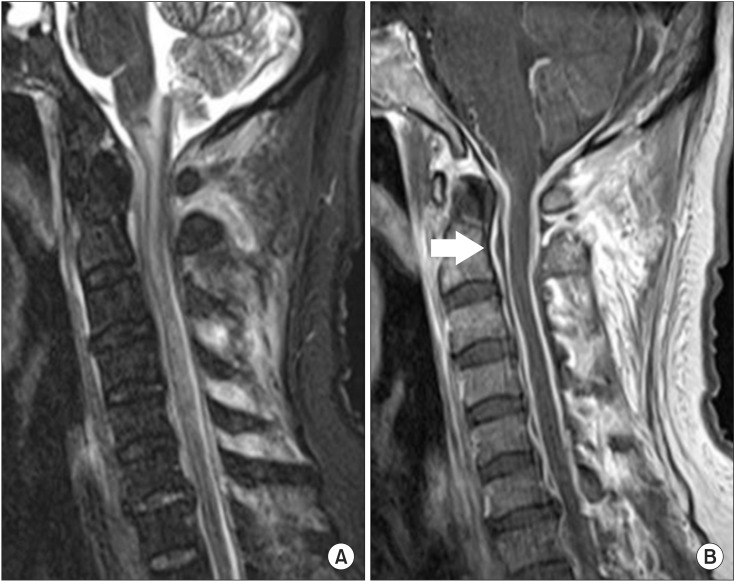
A 60-year-old male with a 5-year history of DM, 9-year history of hypertension, and 8-month history of angina presented with severe posterior neck pain and chest pain. Previously, the patient had persistent LBP with left thigh radiating pain for one month. At a local pain clinic, he was diagnosed as lumbar herniation of nucleus pulposus. He received two lumbar ESIs at the left L4 and L5 level with a 2-week interval. The injections produced no improvement. He visited another pain clinic 3 days later and received a lumbar ESI at the same level. A few hours after the injection, he complained of severe posterior neck and chest pain. He was transferred to our hospital the next day. The patient first received an electrocardiogram (ECG) and cardiac enzyme study due to the chest pain. ECG showed regular sinus rhythm and cardiac enzyme studies were all within normal limits (CK-MB 4.00 ng/mL, troponin-T <0.01 ng/mL). Fever developed a few hours after admission. Peripheral blood tests showed elevated white blood cell count of 20,430 (neutrophils 91.4%) and elevated C-reactive protein (24.14 mg/dL). Plasma glucose was also elevated (186 mg/dL). L-spine magnetic resonance imaging (MRI) revealed reticular infiltration at the left posterior epidural space of S1 level, suggesting hematoma in the left posterior epidural space at the L5 and S1 level (Fig. 1). Manual muscle test (MMT) revealed 5/5 muscle strength in all extremities. Methicillin-susceptible Staphylococcus aureus was isolated from blood culture. Under the diagnosis of lumbar epidural abscess, antibiotic treatment was started (clindamycin 600 mg IV, ceftriaxone 2 g IV). No improvement was noted, and a different antibiotic regimen was prescribed (vancomycin 2 g IV, Tazocin 4.5 g IV). The second regimen controlled the fever and laboratory findings indicated slight improvement. However, systemic elevation of plasma glucose remained, despite intensive insulin therapy. Ten days after hospitalization, the patient began to complain of bilateral lower extremity weakness and sensory disturbance. MMT showed 2/5 muscle strength in both lower extremities. Three days after the onset of motor weakness, the symptoms progressed from both lower extremities to include both upper extremities. MMT revealed 1/5 muscle strength in all extremities and the sensory examination showed hypoesthesia below the C4 dermatome. C-spine MRI revealed signal changes with swelling of the spinal cord at cervical cord and medulla oblongata with epidural fluid collection at the upper cervical area (Fig. 2A). Leptomeningeal enhancement of medulla oblongata and cervical cord was evident on the C-spine MRI (Fig. 2B). One week after the onset of motor weakness, the epidural abscess was removed with C1 and C2 laminectomy to decrease pressure of the upper cervical spine. Despite the surgery, no neurological improvement was observed. Two weeks after the surgery, a follow-up C-spine MRI revealed no interval change (Fig. 3). Two months after hospitalization, he was transferred to the department of rehabilitation medicine and received comprehensive rehabilitation therapy with the goal of improvement in motor power and stabilization of sitting balance.
Lumbar ESI has become a common non-surgical treatment modality for LBP management. Its success rate ranges from 20% to 100% [5]. Because of its proven efficacy, the use of ESI is increasing rapidly [1].
Complications associated with ESI are rare but can be severe. Hematoma, epidural abscess and meningitis are the common complications of ESI. Patients who are immunocompromised or with an underlying history of DM or renal failure are more likely to be affected [4]. In particular, DM patients with LBP need more cautious attention, since they may exhibit impaired wound healing and increased susceptibility to infections. Furthermore, injected epidural steroids produce hyperglycemic effect for about 48 hours [6]. Consistent elevation of plasma glucose level is detected in some DM patients after lumbar ESI.
Clear practice guidelines of lumbar ESI including minimal intervals between multiple injections and other relevant restrictions are lacking in high-risk patients, such as diabetic patients [5]. Data from the Korea Health Insurance Review and Assessment Service indicate that, there are no appreciable differences in practice guidelines between general hospitals and local pain clinics for appropriate doses of steroids or controlled doses of steroids for diabetic patients. Pain physicians in South Korea usually limit the total injection amount of triamcinolone to 40 mg/day and 162.6 mg/yr. Nearly 60% of these physicians limit the average amount of steroids for diabetic patients, to an average of 0.6 fold of the total steroid dose. However, the minimal interval of subsequent ESIs at local pain clinics of about 2 weeks which is statistically shorter than the interval of just over 3 weeks at general hospitals [5]. The data indicate that the average number of ESI trials at local pain clinics is 2 million, which is approximately 16 times more than the average trial number of 120,000 at general hospitals. Likewise, there is a huge difference in an average number of trials between general hospitals and local pain clinics, with the possibility of overdose of the amount of lumbar steroids, because of the absence of restrictions including minimal interval of subsequent ESIs.
A case of lumbar arachnoiditis after caudal ESI was previously reported in the United Kingdom, but there have been no reported cases of cervical meningomyelitis followed by lumbar ESI [7]. Our patient's initial symptom after ESI, which included neck stiffness, was a sign of cervical meningitis. Underlying history of DM, multiple lumbar injections, and minimal interval of subsequent ESIs less than 2 weeks would have increased the risk of infection. Elevated glucose levels and identification of S. aureus in the blood support the clinical evidence of infection due to ESI. Cerebrospinal fluid sampling was avoided because of potential risk of secondary infections.
Antibiotic treatments did not improve the patient's symptom, prompting to surgical treatment. However, there was no neurological improvement. Likewise, complications associated with ESI could present severe symptoms in high-risk patients.
Chronic LBP is a major health condition. As the number of interventions in the management of the LBP is increasing annually, the numbers of complications after ESI is also on the rise [8]. Therefore, pain physicians should be aware of complications, such as cervical meningomyelitis, which should be considered in the differential diagnosis. Also, appropriate practice guidelines for ESI need to be established for high-risk patients, including DM.
References
1. Manchikanti L, Pampati V, Falco FJ, Hirsch JA. Assessment of the growth of epidural injections in the medicare population from 2000 to 2011. Pain Physician. 2013; 16:E349–E364. PMID: 23877459.
2. Brisby H. Pathology and possible mechanisms of nervous system response to disc degeneration. J Bone Joint Surg Am. 2006; 88(Suppl 2):68–71. PMID: 16595447.

3. Abdi S, Datta S, Lucas LF. Role of epidural steroids in the management of chronic spinal pain: a systematic review of effectiveness and complications. Pain Physician. 2005; 8:127–143. PMID: 16850050.
4. Joshi SM, Hatfield RH, Martin J, Taylor W. Spinal epidural abscess: a diagnostic challenge. Br J Neurosurg. 2003; 17:160–163. PMID: 12820759.

5. Kim EJ, Moon JY, Park KS, Yoo DH, Kim YC, Sim WS, et al. Epidural steroid injection in Korean pain physicians: a national survey. Korean J Pain. 2014; 27:35–42. PMID: 24478899.

6. Even JL, Crosby CG, Song Y, McGirt MJ, Devin CJ. Effects of epidural steroid injections on blood glucose levels in patients with diabetes mellitus. Spine (Phila Pa 1976). 2012; 37:E46–E50. PMID: 21540770.

7. Nanjayan SK, Swamy GN, Yallappa S, Bommireddy R. Arachnoiditis following caudal epidural injections for the lumbo-sacral radicular pain. Asian Spine J. 2013; 7:355–358. PMID: 24353855.

Fig. 1
L-spine magnetic resonance imaging data. (A) T2 sagittal view showing bulged disc at L4-5, L5-S1. (B) T2 transverse view showing reticular infiltration at left posterior epidural space of S1.

Fig. 2
C-spine magnetic resonance imaging data. (A) T2 sagittal view showing signal change and swelling from medulla oblongata to upper thoracic cord. (B) T1 sagittal view showing leptomeningeal enhancement of medulla oblongata and cervical cord (arrow, epidural fluid collection at upper cervical area).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download