Abstract
The thalamus, located between the cerebrum and midbrain, is a nuclear complex connected to the cerebral cortex that influences motor skills, cognition, and mood. The thalamus is composed of 50-60 nuclei and can be divided into four areas according to vascular supply. In addition, it can be divided into five areas according to function. Many studies have reported on a thalamic infarction causing motor or sensory changes, but few have reported on behavioral and executive aspects of the ophthalmoplegia of the thalamus. This study reports a rare case of a paramedian thalamus infarction affecting the dorsomedial area of the thalamus, manifesting as oculomotor nerve palsy, an abnormal behavioral change, and executive dysfunction. This special case is presented with a review of the anatomical basis and function of the thalamus.
Stroke is the third leading cause of death in Korea and a leading cause of major disabilities in the elderly population. Thalamic infarctions account for 14% of all lacunar infarctions, which in turn account for a quarter of all ischemic strokes [1].
The thalamus, located between the cerebrum and midbrain, is a nuclear complex connected to the cerebral cortex and others. The thalamus has a nucleus that plays a major role in the sensory pathway and also has nuclei involved in motor skills, cognition, and mood [2]. These thalamic nuclei can be divided into five groups according to their function [3] or four groups according to their arterial supply [4].
Therefore, a thalamic arterial infarction can cause various symptoms and signs depending on the nuclei involved and combination of the nuclei involved. This report presents a recent case of a paramedian thalamic artery infarction with ophthalmoplegia, executive dysfunction, and behavioral changes. This rare case is reported with a review of the function and anatomical basis of the thalamus.
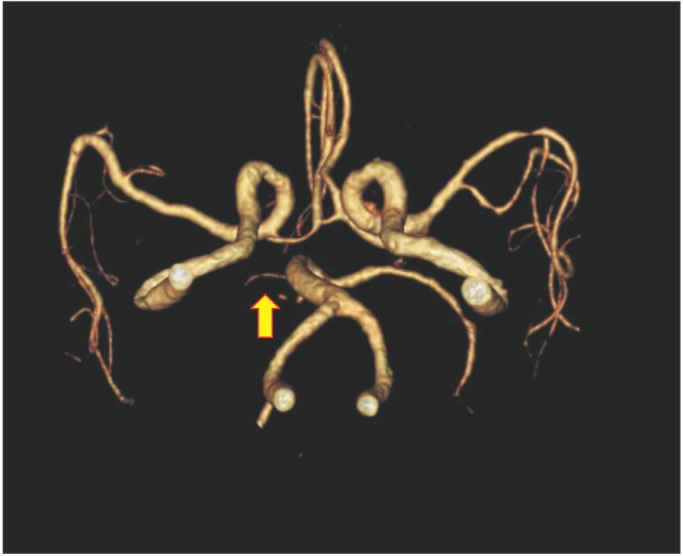
A 67-year-old man with a 20-pack-a-year smoking history was admitted to the neurology department via the emergency room because he had mild left-side weakness and dysarthria. He was diagnosed with an acute infarction of the right paramedian thalamus based on magnetic resonance imaging (MRI) (Fig. 1). Computed tomography angiography showed right posterior cerebral artery (PCA) stenosis (Fig. 2).
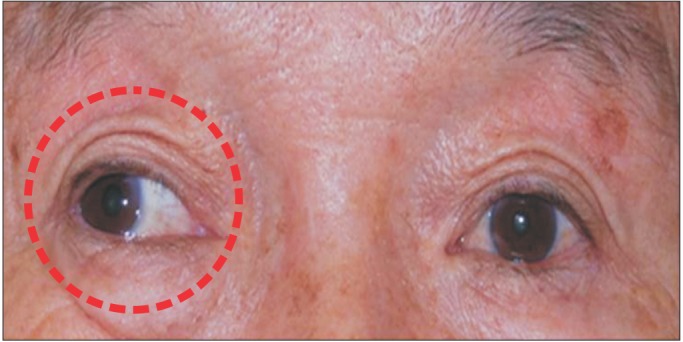
At admission, the patient was alert and oriented to time, place, and person. At rest, the patient showed a sustained outward deviation of the right eyeball (Fig. 3). Examination revealed a right ptosis with left and right pupil diameters of 3 cm and 4 cm, respectively. The right pupil showed a poor light reflex. The patient showed weakness in adduction, elevation, and depression in the movement of the right eyeball. The abduction of the right eyeball and all movements of the left eyeball were normal, and intact visual fields were observed. The patient complained of double vision. During a cranial nerve examination (excluding ophthalmoplegia), the patient showed central-type left facial nerve palsy. Gag reflexes on both sides were spared. Despite dysarthria, there was no deviation of the tongue or limitation of tongue movements.
The patient showed no pathologic reflexes from Babinski and Hoffmann tests, and his cerebellar function was normal. A slight decrease in light touch and proprioception was present in the left upper and lower extremities. All Brunnstrom recovery stages of the left upper extremities, hand, and lower extremities were checked as five, but the manual muscle test (MMT) revealed a decrease in muscle power of the left lower extremities, with a grade of 3. Other laboratory tests were normal.
The patient was transferred to department of rehabilitation medicine for the treatment of left-side weakness and dysarthria. He was then referred to an ophthalmologist for an evaluation of diplopia. An ophthalmological examination including ophthalmoscopy was normal, without any peripheral nerve or muscle involvement. An eye patch was prescribed for his right eye for the diagnosis of right third cranial nerve palsy. Four weeks after admission, his eyeball deviation and diplopia gradually recovered, and about three months later his ocular movements were normal.
During admission, the patient developed uncontrollable sexually impulsive behavior and insomnia. He asked his female caregiver to touch his body when showering and to lie down on the bed together. Due to the insomnia and behavioral changes, he was referred to the department of psychiatry but found to have no specific condition other than hypomania. To control his sexual desire and sleep cycle, the psychiatrist recommended the use of a drug, Depakote (500 mg), before sleep. When the patient started the medication, his behavioral change decreased. After two months, the medication was ceased without any worsening of symptoms.
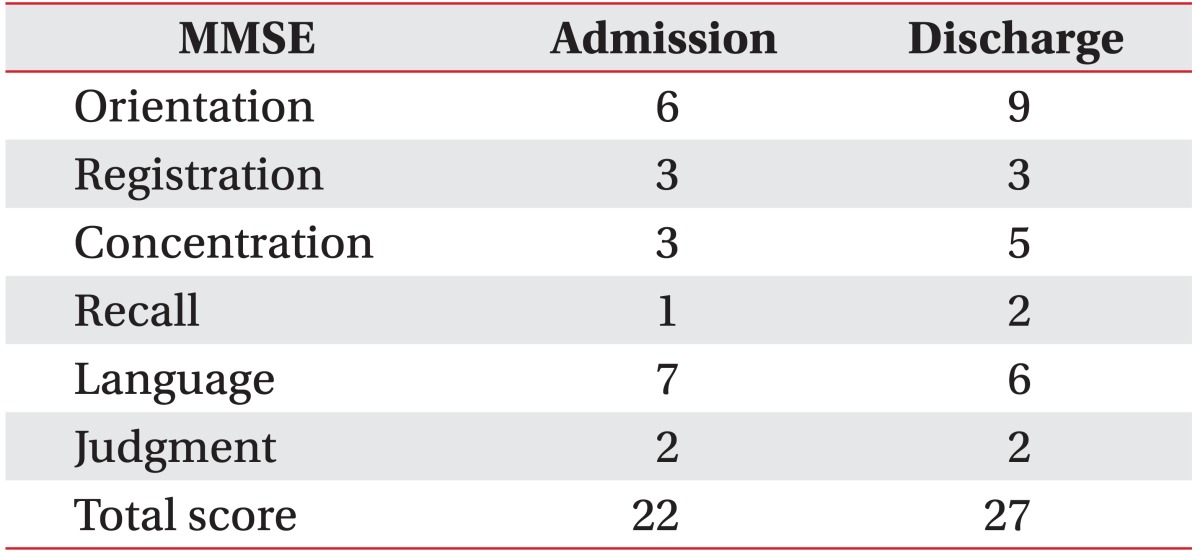
Upon admission to department of rehabilitation medicine, the Mini-Mental State Examination (MMSE) was checked as 22, and the patient showed no significant cognitive problems (Table 1). However, he presented with some definite abnormality in executive function. The frontal lobe assessment battery (FAB) showed a low score of 7 (Table 2). Other tests revealed that he had severe impairment in daily activity (Modified Barthel Index [MBI] score is 10), difficulty standing, and gait disturbance (Berg Balance Scale [BBS] is 7). The somatosensory evoked potential test showed decreased amplitude in the left upper and lower extremities, implicating some abnormality in the somatosensory pathway.
During four weeks of intensive rehabilitation, the patient went through strengthening and endurance training and static/dynamic balance training for his left-side weakness and gait disturbance. Occupational treatment was also provided to improve executive dysfunction. A mild cognitive deficit remained even after treatment but the MMT of the left lower extremities improved to grade 4. In addition, the BBS score saw an improvement to 37. The patient could walk using a walker without assistance, exhibiting substantial progress in gait disturbance. Despite signs of improvements in the MMSE (Table 1) and MBI (10 to 68), executive dysfunction showed only a slight improvement (FAB score of 9) (Table 2).
The thalamus is connected to the cerebral cortex and other structures with important neural connectivity. According to their function, thalamic nuclei can be divided into five groups: 1) reticular and intralaminar nuclei associated with arousal and pain, 2) sensory nuclei, 3) effector nuclei participating in motor and language skills, 4) associative nuclei affecting high-level cognitive functions, and 5) limbic nuclei involved in emotion and motivation [3]. In the present case, mild paresthesia and mild motor weakness were present on the affected side, indicating the involvement of sensory and effector nuclei. In addition, executive dysfunction and behavioral changes appeared to be associated with associative nuclei.
In addition to the five groups based on function, thalamic nuclei can also be divided into four groups according to their arterial supply: 1) the tuberothalamic artery, also known as the polar artery, 2) the thalamogeniculate artery, 3) the posterior choroidal artery, and 4) the paramedian artery, also called the thalamosubthalamic artery [4]. Therefore, a thalamic local lesion is capable of causing various symptoms and signs depending on the specific localization. In the present case, brain MRI revealed an ischemic infarction of the paramedian artery arising from the proximal segment (P1) of the PCA. With the exception of the tuberothalamic artery, which arises from the posterior communicating artery, all other arteries arise from the PCA. The dorsomedial and posteromedial nuclei, along with the internal medullary lamina and intralaminar nuclei of the thalamus, are supplied by the paramedian artery [5].
An infarction of the thalamus that causes uncontrollable sexual behavior and insomnia, as in the present case, has rarely been reported. Sexually abnormal behavior, disinhibition syndromes, and impulsivity are well-known symptoms of a lesion of the frontal lobe, amygdala, hypothalamus, and frontotemporal circuit. However, few such reports have presented a thalamic infarction. According to previous reports, a paramedian thalamus infarction can cause behavioral changes such as sleep disturbance, amnesia, disinhibition syndromes, personality changes, and the loss of self-activation [6]. In a paramedian thalamic infarction, behavioral change can be induced by disturbance of the dorsomedial nucleus, which is associated with the prefrontal-subcortical circuit that includes the orbitofrontal cortex. Clinicians should pay special attention to these behavioral changes because they can be easily misdiagnosed as dementia when there is no other neurological abnormality [7].
Executive dysfunction without definite dementia appears to be related to the medial dorsal nucleus, which is one of the associative nuclei responsible for high-level cognitive function. Infarction of the paramedian artery supplying the medial dorsal nucleus reduced working memory and caused executive dysfunction. Executive dysfunction has also been reported in tuberothalamic infarction, which may be related to anterior and ventral anterior nuclei associated with learning, memory, and motor programming [3]. Executive function is known to influence the long-term disability of stroke patients, and therefore accessing executive function is crucial for these patients.
Oculomotor nerve palsy is a common symptom of a midbrain infarction, but there have been few reports of a paramedian thalamic infarction inducing third-nerve palsy without a definite lesion on the brainstem, as in this present case [8]. In an infarction at paramedian artery territory of the PCA, the clinical feature of ophthalmoplegia demonstrates oculomotor palsy or vertical gaze palsy [9]. The upward gaze palsy is likely due to the involvement of the frontofugal dorsothalamic bundle transversing the mediodorsal nucleus and internal medullary lamina of the thalamus on its way to superior colliculus [410]. Along with a thalamic lesion, a coexisting lesion involving the rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF) in the upper midbrain may account for the vertical gaze palsy [10]. Even though there was no definite midbrain lesion in this case, the medial gaze palsy can be partly attributable to the involvement of the oculomotor nuclei or fascicle, which is usually associated with thalamic lesion extension [9]. In this case, the oculomotor palsy was caused by an ipsilateral thalamic infarction which was similar to the crossed hemiplegia seen in the brainstem lesion.
As mentioned earlier, a thalamic infarction can cause not only well-known symptoms such as motor impairments and sensory changes but also rare symptoms such as oculomotor palsy, abnormal behavioral changes, and impaired executive function. Such diagnostics suggest that clinicians should emphasize the early assessment and proper management of patients with a thalamic infarction.
References
1. Sacco S, Marini C, Totaro R, Russo T, Cerone D, Carolei A. A population-based study of the incidence and prognosis of lacunar stroke. Neurology. 2006; 66:1335–1338. PMID: 16682663.

2. Herrero MT, Barcia C, Navarro JM. Functional anatomy of thalamus and basal ganglia. Childs Nerv Syst. 2002; 18:386–404. PMID: 12192499.

4. Bogousslavsky J, Regli F, Uske A. Thalamic infarcts: clinical syndromes, etiology, and prognosis. Neurology. 1988; 38:837–848. PMID: 3368064.

5. Jimenez Caballero PE. Bilateral paramedian thalamic artery infarcts: report of 10 cases. J Stroke Cerebrovasc Dis. 2010; 19:283–289. PMID: 20610185.
6. Carrera E, Bogousslavsky J. The thalamus and behavior: effects of anatomically distinct strokes. Neurology. 2006; 66:1817–1823. PMID: 16801643.

7. Spinella M. Hypersexuality and dysexecutive syndrome after a thalamic infarct. Int J Neurosci. 2004; 114:1581–1590. PMID: 15512841.
8. Mondon K, Bonnaud I, Debiais S, Brunault P, Saudeau D, de Toffol B, et al. Abrupt onset of disturbed vigilance, bilateral third nerve palsy and masturbating behaviour: a rare presentation of stroke. Emerg Med J. 2007; 24:600–601. PMID: 17652699.

9. Thurtell MJ, Halmagyi GM. Complete ophthalmoplegia: an unusual sign of bilateral paramedian midbrain-thalamic infarction. Stroke. 2008; 39:1355–1357. PMID: 18309144.
10. Gentilini M, De Renzi E, Crisi G. Bilateral paramedian thalamic artery infarcts: report of eight cases. J Neurol Neurosurg Psychiatry. 1987; 50:900–909. PMID: 3625213.

Fig. 1
A magnetic resonance image showing an acute right paramedian thalamic infarction and mild ischemic change possibly due to small vessel disease (A-H). Arrows point to the areas of the paramedian infarction on a diffuse weighted image (A-C) and on an apparent diffusion coefficient image (F, G).





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download