This article has been
cited by other articles in ScienceCentral.
Abstract
Congenital muscular torticollis (CMT) and craniosynostosis are diseases that cause plagiocephaly and craniofacial asymmetry in children. In our literature review, we did not find any report of concurrent manifestation of CMT and craniosynostosis. A 41-month-old boy visited our hospital with left torticollis, right laterocollis, and craniofacial asymmetry as the main findings. During clinical examination, prominent right sternocleidomastoid muscle and limited range of motion of the neck were noted, and right CMT was confirmed by magnetic resonance imaging of the neck. Three-dimensional computed tomography of the skull, which was conducted due to the unusual appearance of the skull with a large head circumference, mild brachycephaly, as well as left plagiocephaly, revealed premature closure of the sagittal suture. Thus, we report the first case that showed concurrence of CMT and sagittal synostosis. We recommend that concurrently manifested craniosynostosis needs to be examined if the subject with CMT displays unusual craniofacial asymmetry to a greater extent than deformational plagiocephaly.
Go to :

Keywords: Torticollis, Craniosynostosis, Plagiocephaly
INTRODUCTION
Plagiocephaly refers to an asymmetrical and flattened deformity of the skull. The most common form of plagiocephaly is deformational plagiocephaly (DP), which occurs due to persistent external forces that mold the skull. There are several risk factors for DP including congenital muscular torticollis (CMT), premature birth, multiparity, delivery with cephalhematoma, auricular deformity and decreased fetal mobility or activity level [
1]. In children, DP is frequently accompanied by CMT, in which unilateral shortening of the sternocleidomastoid (SCM) muscle manifests contralateral torticollis as well as ipsilateral laterocollis with ensuing contralateral DP.
Also, plagiocephaly could be induced by craniosynostosis, which is a rare condition that causes head deformity due to premature fusion of one or more of the cranial sutures. Sagittal synostosis is the most common type of craniosynostosis, which results in a long head with bitemporal narrowing and palpable bony ridge along the sagittal suture [
2]. Since craniosynostosis can affect brain growth and increase intracranial pressure, surgical measures are needed in most of the cases. Therefore, differential diagnosis of plagiocephaly is important for proper management of this condition.
However, what happens if craniosynostosis and CMT manifest concurrently? In our review of relevant litera tures, we did not find any report of concurrent manifestation of CMT and craniosynostosis. Here, we report a case of concurrent manifestation of CMT and craniosynostosis along with a relevant literature review.
Go to :

CASE REPORT
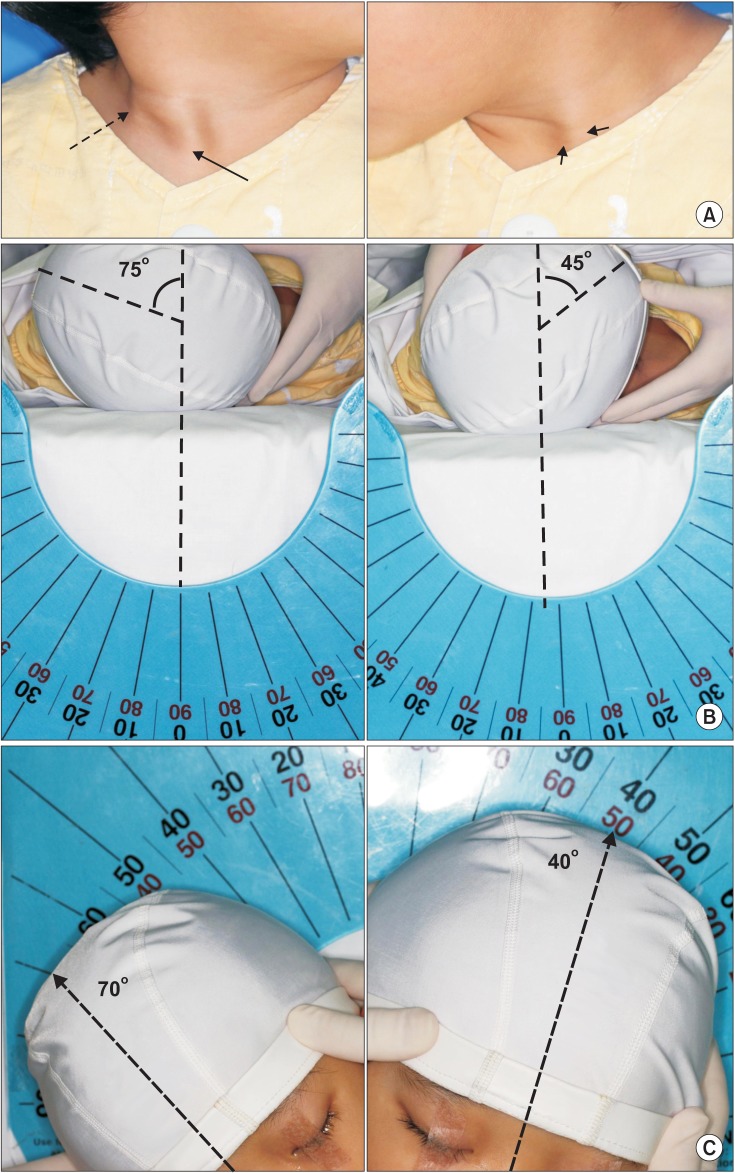
A 41-month-old boy visited our hospital with left torticollis, right laterocollis and craniofacial asymmetry as the main findings. He was born through a normal vaginal delivery at full term. Pregnancy and delivery were uncomplicated. Clinical examination revealed prominence of both sternal and clavicular heads of the right SCM (
Fig. 1A) along with limited range of motion of the neck (
Fig. 1B, 1C). Plagiocephaly on the left occiput (
Fig. 2B) was evident with 20 mm of diagonal difference, which is defined as the difference between 2 diagonal cranial diameters, and anterior displacement of the left ipsilateral ear. Flat right zygomatic arch (
Fig. 2B) was also observed. While the child's height and weight were 103 cm (75-90th percentile) and 17.9 kg (75-90th percentile), respectively, the head circumference was 54 cm (>97th percentile). The cephalic index, which is defined as the maximum skull breadth divided by the maximum AP length, was 87%, evidencing the presence of brachycephaly (normal range, 76%-85%) [
3]. Developmental history was not particularly remarkable since the child began to walk without any assistance at the age of 12 months. The full scale of intellectual quotient and social maturity quotient of the child at 41 months of age were 93 and 105.8, respectively.
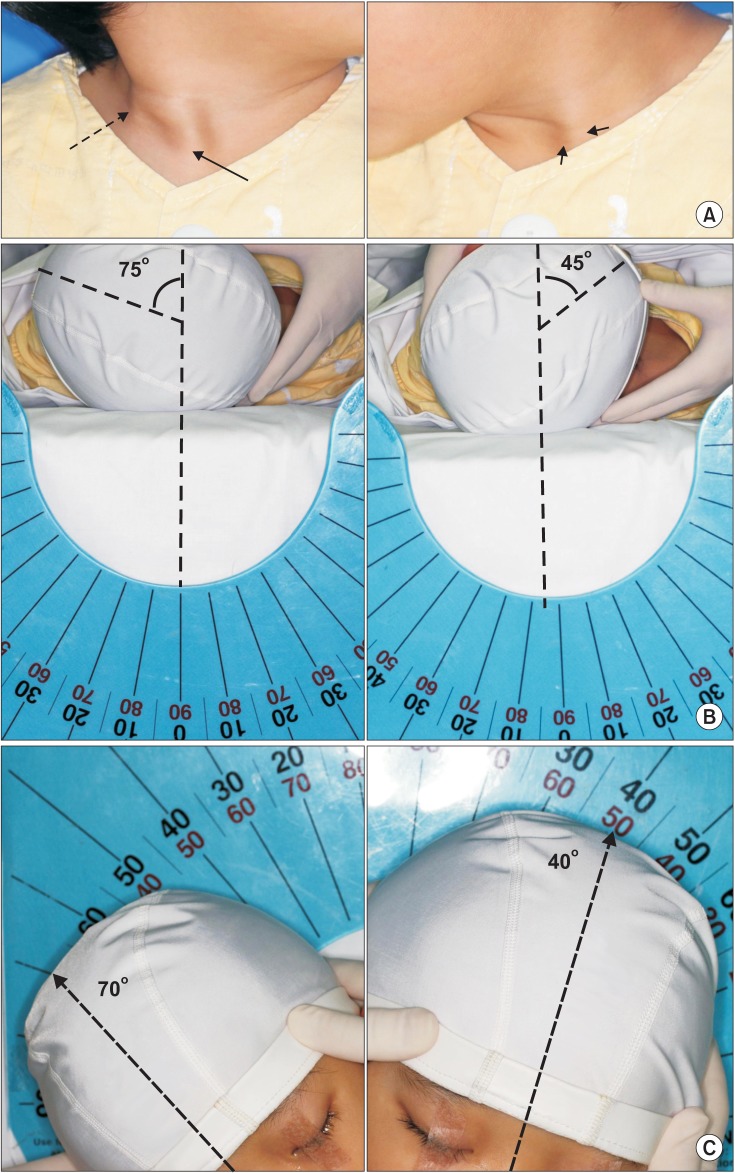 | Fig. 1A 41-month-old boy shows (A) sternal (solid arrow) and clavicular (dotted arrow) heads of the right sternocleidomastoid muscle, which are more prominent than those on the left side (short arrows). (B) Measurement of the range of motion for cervical rotation shows a 30° deficit in the cervical rotation to the right side and (C) a 30° deficit in lateral flexion to the left side compared with that on the contralateral side. 
|
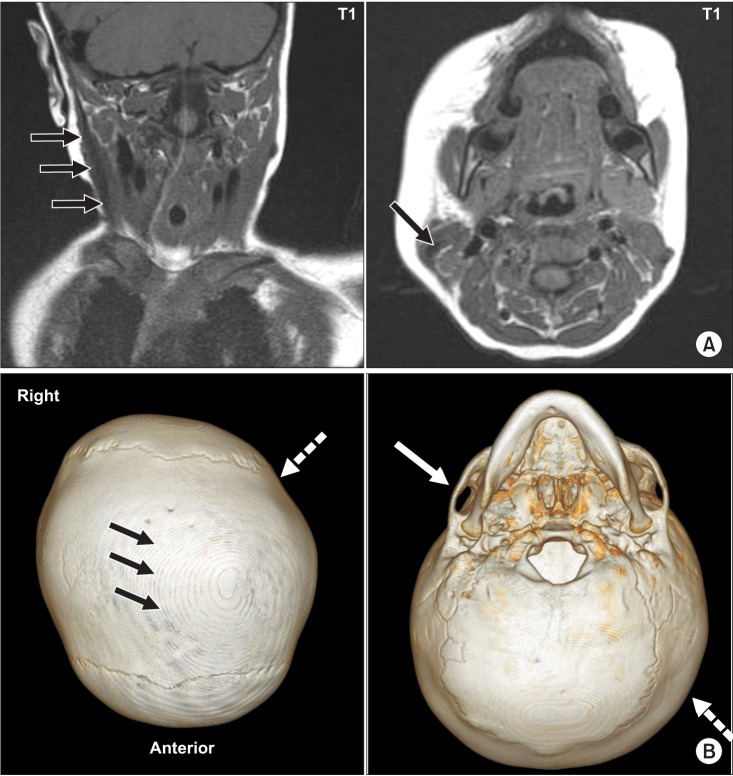
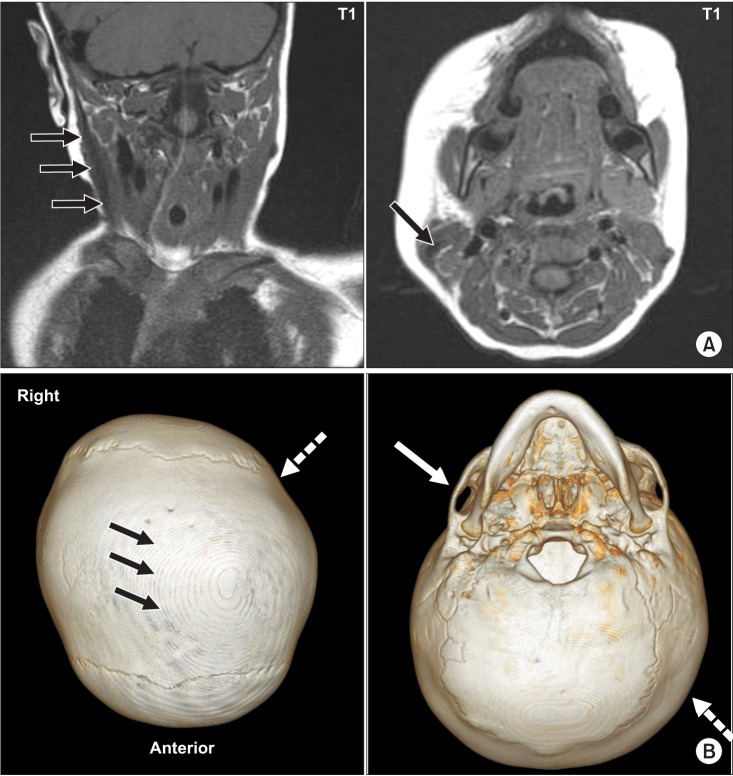 | Fig. 2(A) T1-weighted coronal and axial magnetic resonance images of the neck display fusiform thickening and low signal intensity within the right sternocleidomastoid muscle (solid arrow). (B) Three-dimensional computed tomography of the brain shows premature closure of the sagittal suture (black arrows) with left occipital plagiocephaly (dotted arrow) and flattened right zygomatic arch (white arrow). 
|
Magnetic resonance imaging (MRI) of the neck illustrated low signal intensity within the thickened right SCM, which is regarded as the typical finding of CMT [
4] (
Fig. 2A). But, due to the unusual appearance of the skull with a large head circumference, mild brachycephaly, and left plagiocephaly, three-dimensional computed tomography (3D-CT) of the skull was performed, and premature closure of the sagittal suture, which is an indication of sagittal synostosis, was observed (
Fig. 2B). No mutation was identified by Sanger sequencing of fibroblast growth factor receptor 2 (
FGFR2), which is known to be one of the genes that induce craniosynostosis. Moreover, there was no evidence of increased intracranial pressure.
Therefore, the boy was diagnosed with concurrent manifestation of CMT and sagittal synostosis. For treatment of the right CMT, he underwent unipolar resection of both the sternal and clavicular heads of the right SCM at the clavicular end. For sagittal synostosis, cranioplasty was recommended and it was taken into consideration by the child's parents.
Go to :

DISCUSSION
CMT is one of the most common musculoskeletal problems in children and it is frequently accompanied by DP. Although in most of the cases, the abnormal skull shape in CMT is due to DP, we experienced a case with concurrent manifestation of CMT and sagittal synostosis. Based on our review of relevant literatures, this appears to be the first report of concurrent manifestation of CMT and craniosynostosis, illustrating that the abnormal skull shape in CMT could be caused by factors other than DP. Therefore, the possibility that an abnormal head shape accompanied by CMT could be induced by craniosynostosis as well as by DP should be considered.
Previously, Raco et al. [
5] and Koljonen et al. [
6] reported the cases of craniosynostosis with congenital torticollis. For establishing the diagnosis of CMT, ultrasonography or MRI has been used to detect the characteristic fibrotic lesion in the SCM [
4]. However, in these two case reports, the patients did not show fibrosis or thickening of the SCM. They only reported abnormal posture of the head and the neck, which was improved by physical therapy alone. In this context, the patients in these two reports could not be diagnosed with CMT although they had abnormal posture of the head and neck.
Although CMT is thought to be caused by various factors including birth trauma, ischemia, intrauterine malposition, and heredity, the actual cause of CMT is yet to be confirmed [
7]. Some causes of craniosynostosis include biomechanical factors arising from the constraint exerted on the fetal head during pregnancy, environmental factors, hormonal factors, and genetic factors. However, familial or genetic factors are less significant in sagittal synostosis than in the other forms of craniosynostosis [
8]. Therefore, intrauterine fetal head constraint has been implicated as an important causative factor in sagittal synostosis [
9]. In our case, although it is difficult to ascertain the pathogenesis of concurrent manifestation of CMT and sagittal synostosis, the constraint exerted on the intrauterine fetal head and neck might be one of the causative factors.
In our case, the patient did not develop scaphocephaly typically associated with sagittal synostosis. Scaphocephaly is a predictable consequence of sagittal synostosis and refers to a boat-shaped skull deformity and reduced cephalic index (<76%) [
3]. In contrast, non-scaphocephalic sagittal synostosis is a rare diagnosis. Morritt et al. [
10] were the first to report non-scaphocephalic sagittal synostosis in 8 (4.1%) of the total 193 patients who had isolated sagittal synostosis. According to the report, there are a number of possible explanations including the following: if fusion of the suture occurred at a later stage after the majority of skull growth had taken place, then, the secondary defect induced by compensatory over-growth of adjacent sutures is likely to be less severe in comparison to the secondary defect arising from fusion that occurred at an earlier stage. Accordingly, the fusion of the sagittal suture at a later stage may be a possible cause in our case.
One interesting finding in our case is that although both synostotic and non-synostotic etiologies were the causes of plagiocephaly, non-synostotic DP displayed more prominent clinical expression. For example, the patient displayed a transdiagonal difference of 20 mm, contralateral occipital flattening, flattened ipsilateral zygomatic arch, and anterior shifting of the contralateral ear. As there is no case report and research demonstrating concurrent manifestation of CMT and craniosynostosis, it is difficult to conjecture the accurate pathomechanism of marked non-synostotic DP as in the case of this patient. Nonetheless, we can assume that the skull shape of the patient resulted from the internal force caused by craniosynostosis and the external force caused by CMT, respectively; however, the external force by CMT seemed to be the main reason in this case.
Here, we report the first case of concurrent manifestation of CMT and craniosynostosis with presentation of non-scaphocephalic sagittal synostosis. The diagnosis of concurrent manifestation of both conditions would be complicated and challenging. We conclude that appropriate examination of the skull shape is needed for differential diagnosis and proper management. We recommend that if a subject with CMT displays unusual craniofacial asymmetry, for example, scaphocephaly, brachycephaly, abnormal head circumference and symptoms other than DP, 3D-CT of the skull should be performed to rule out the possibility of concurrent manifestation of craniosynostosis.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download