This article has been
cited by other articles in ScienceCentral.
Abstract
Cerebral venous sinus thrombosis (CVST) is an uncommon cause of cerebral infarction, compared to arterial diseases. It is often unrecognized at initial presentation due to the diversity of causes and clinical manifestations. A 29-year-old female patient complained of severe headache and presented at the emergency room with altered consciousness. Brain computed tomography and brain magnetic resonance image revealed the left sigmoid sinus thrombosis with venous hemorrhagic infarction (VHI) in the left temporal lobe. The patient had no past medical and family history of bleeding diathesis. The laboratory finding at the admission showed severe iron-deficiency anemia (IDA), and protein C and S activities were decreased. After the neurosurgery, iron replacement, and neurorehabilitation, the patient had a good recovery. There has been no known recurrence. We report our therapeutic intervention on a very rare case of CVST and VHI, with IDA as a probable cause of cerebral thrombosis.
Go to :

Keywords: Anemia, Iron-deficiency anemia, Intracranial thrombosis, Stroke
INTRODUCTION
Cerebral venous sinus thrombosis (CVST) is the presence of thrombosis in the dural vein, which occurs when a blood clot forms in the brain's venous sinus that prevents blood from draining out of the brain [
1]. Patients with venous sinus thrombosis have a variety of symptoms [
1,
2]. Venous hemorrhagic infarction (VHI) is presented as a severe form of clinical symptom and a poor prognostic factor of CVST [
2]. CVST is a rare cause of cerebral infarction compared to arterial diseases [
1]. CVST can be caused by a variety of congenital or acquired diseases, such as dehydration, infection, or hematologic disorder [
3]. Iron-deficiency anemia (IDA) is one of common causes of pediatric CVST but not of adult CVST. Recently, IDA has been described as a very rare cause of adult CVST [
4]. We hereby report a very rare case of adult CVST and VHI with IDA, with review of the related literatures.
Go to :

CASE REPORT
A 29-year-old woman (height 168 cm, weight 55 kg, body mass index [BMI] 19.48 kg/m
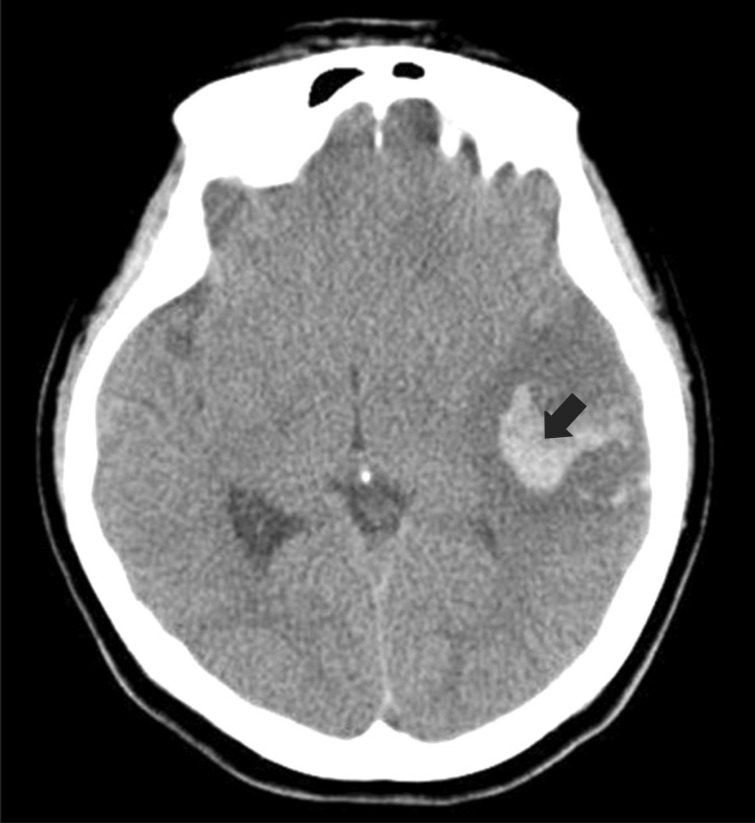
2) was presented at the emergency room with altered consciousness. The patient developed sudden onset of motor weakness in the right extremities and severe headache. Brain computed tomography (CT) was checked at a local clinic, which revealed subcortical hemorrhage in the left temporal lobe (
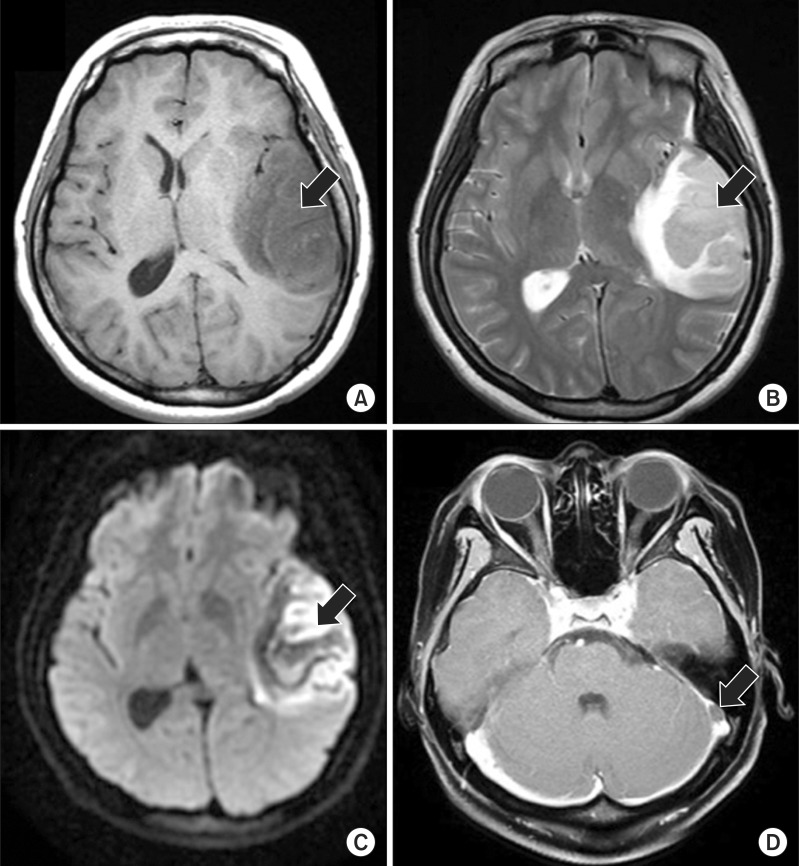
Fig. 1). After being transferred to our hospital, brain CT angiography was performed and no signs of steno-occlusive lesion, aneurysm, or arteriovenous malformation were found. Brain magnetic resonance image revealed the left sigmoid sinus thrombosis with VHI in the left temporal lobe (
Fig. 2). The vital signs were stable. The patient had no medical history, such as hypertension, diabetes mellitus, hepatitis, and pulmonary tuberculosis. She was not taking any medications. On neurological examination, her mental status was stuporous and Glasgow Coma Scale was 8 points. The laboratory data at the admission revealed severe anemia with hemoglobin 6.5 g/dL, hematocrit 26.4%, mean corpuscular volume 69.7 fL, white blood cells 13,600/mm
3, and platelet 280,000/µL. The patient was transfused with packed red blood cells. Coagulation time (PT-INR 1.04, aPTT 28.5 sec), liver function test, and renal function test were normal. Anemia study displayed IDA with serum iron concentration of 38 µg/dL (range 50-170 µg/dL), ferritin 14.2 ng/mL (range 4.63-274.6 ng/mL), and total iron-binding capacity 395 µg/dL (range 250-370 µg/dL). The patient underwent decompressive craniectomy and duroplasty after 3 days of onset, due to aggravation of parenchymal edema in VHI. After the neurosurgery, the patient received intravenous vitamin K1 10 mg for 2 days, prophylactic anticonvulsants (valproate sodium, 1,200 mg a day) for 1 month, and oral iron replacement for 4 months.
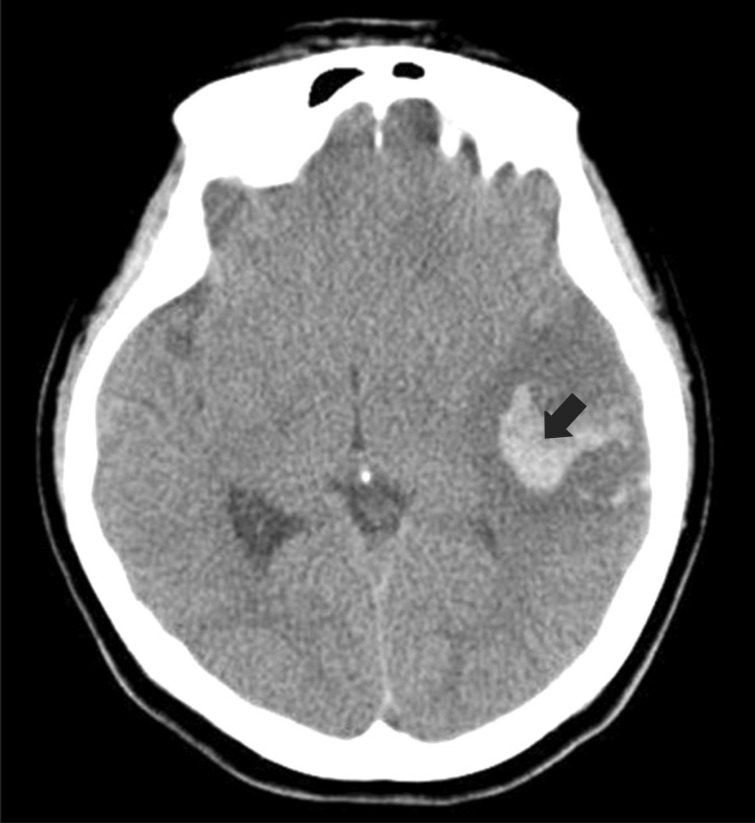 | Fig. 1Brain computed tomography shows high attenuated lesion (black arrow) in the left temporal lobe. 
|
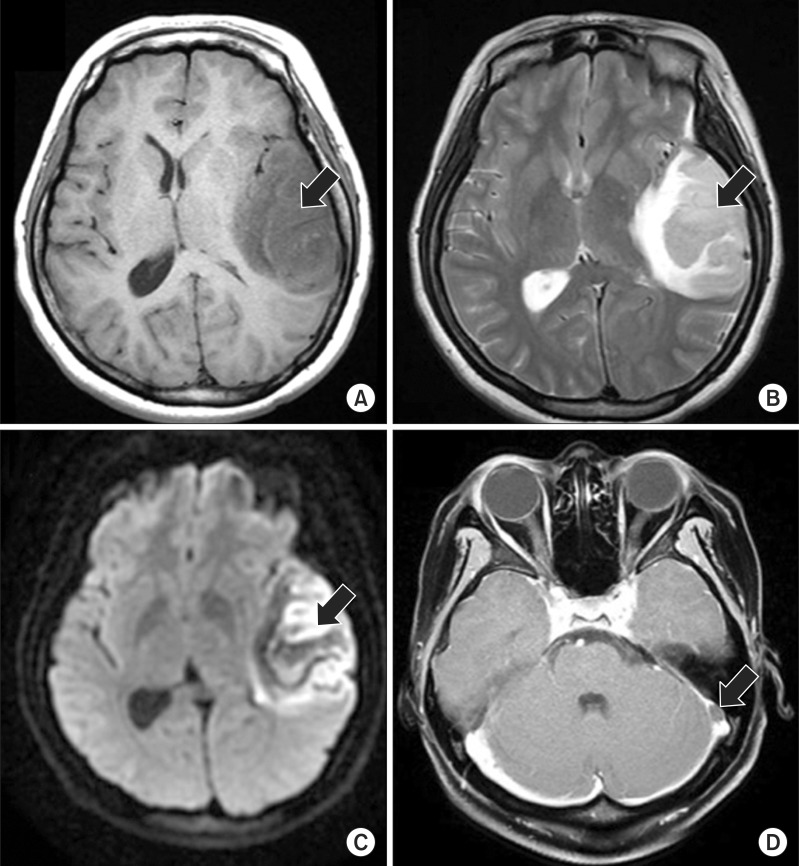 | Fig. 2Magnetic resonance images of brain. (A) T1-weighted axial image shows low signal intensity involving the left temporal lobe (black arrow). (B) T2-weighted axial image and (C) diffusion-weighted image show high signal intensity (black arrow) involving the left temporal lobe with gyral hemorrhage. (D) Post-gadolinium T1-weighted image displays filling defect (black arrow) in the left sigmoid sinus. 
|
Protein C level was 69% (range 73%-142%) and protein S was 42% (range 60%-140%). But other coagulation factors were within the normal range. The patient had no past history of coagulation abnormality, recent trauma, or hormonal substitution, and no family history of any medical diseases including bleeding diathesis. There was no evidence of gastrointestinal bleeding or history indicating possible cause of iron deficiency.
The patient was referred to rehabilitation unit at 3 weeks after the onset of symptoms. On physical examination in the Department of Rehabilitation, her mental status was alert and her muscle strength was of grade 3 in the right upper limb and grade 4 in the right lower limb, according to the manual muscle test. The aphasia quotient (AQ) on the Korean version of Western Aphasia Battery (K-WAB) was 34.2%, and the type of aphasia was transcortical motor aphasia. Activities of daily living (ADLs) were performed with moderate dependency and she could not walk without assistance. Cognitive impairment was severe and Korean Mini-Mental Status Exam (K-MMSE) score was 5/30. Rehabilitative management including Bobath neurodevelopmental therapy, gait training, neuromuscular electrical stimulation, occupational therapy, speech therapy, and ADLs training were conducted. After 1 month of rehabilitation program, the patient was able to walk under the supervision of caregiver. Almost all ADLs were performed independently. The patient spoke fluently with some difficulties in naming objects (AQ=75.5%). Cognitive function was also significantly improved to 26/30 on K-MMSE, and she was discharged to a secondary rehabilitation hospital. After 3 months of onset, anemia gradually improved with a hemoglobin value of 12.8 g/dL, and the patient was able to ambulate independently. The patient has been taken aspirin 100 mg and there has been no recurrence so far. She is planning to stay on medication of aspirin hereafter.
Go to :

DISCUSSION
The incidence of CVST is about 2-5 persons per million. It accounts for 0.5%-1% of all stroke affecting female more than male [
1]. The mean age of patients with CVST was 39-41 years [
2,
3,
5]. Its potential life-threatening condition requires rapid diagnosis and treatment. However, the diagnosis of CVST is still commonly overlooked or delayed. The management of CVST is also difficult due to its variety of clinical manifestations and the absence of a uniform treatment approach. A wide range of etiologies is one reason why it is difficult to diagnose and manage the CVST [
1,
6].
Risk factors of CVST are associated with Virchow triad of stasis of the blood, changes in the vessel wall, and changes in the composition of the blood [
6]. Initially, our case was presented as a stroke patient at young age. She had no past medical or family history of coagulation abnormality and bleeding diathesis, but she had IDA on admission. The association of CVST and IDA were not well-recognized in adults. Recently, there have been a few reports of adult CVST patients with IDA [
4]. IDA more commonly occurs in female than men, especially in young women. Acute blood loss is not a common cause of IDA, because IDA only develops over weeks to months of chronic or recurrent blood loss [
7]. Therefore, IDA can be considered as a cause of cerebral thrombosis and not as a result of it in this case. Our patient had severe IDA, but we could not document the cause of IDA in this case.
Protein C/S deficiency can also cause CVST. However, any inflammatory process reduces protein S activity. Indeed, 20% of all hospitalized patients show low free protein S levels. Secondary deficiency of protein C and S can occur due to acute thrombosis [
8]. In this case, protein C and S were tested long after the admission, so we could not figure out the association between CVST and protein C/S deficiency. In this regard, deficiency factors do not seem to be the reason for CVST.
The mechanisms causing thrombosis in IDA are not completely understood, but there are some reports supporting the probability between IDA and thrombosis [
9]. Reactive thrombocytosis secondary to IDA is a rare but recognized cause of stroke. It is well-documented that iron deficiency causes reactive thrombocytosis. However, all cases of iron-related thrombotic events do not accompany elevated platelet count. There was no presence of thrombocytosis in this case. In other pathogenic mechanisms, iron deficiency may contribute to a hypercoagulable state by affecting blood flow within the vessel, by decreased deformability, and increased viscosity of microcytic red blood cells [
9,
10].
Our patient displayed VHI as an initial presentation and underwent neurosurgery. Despite the prediction of poor prognosis, she showed good recovery [
5]. Although we could not precisely pin the cause of CVST, we think that IDA can become a cause of CVST in adults. Therefore, the management of IDA would be necessary for the prevention of cerebral thrombosis.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download