Abstract
Objective
To determine the cutoff value of the pharyngeal residue for predicting reduction of aspiration, by measuring the residue of valleculae and pyriformis sinuses through videofluoroscopic swallowing studies (VFSS) after treatment with neuromuscular electrical stimulator (VitalStim) in stroke patients with dysphagia.
Methods
VFSS was conducted on first-time stroke patients before and after the VitalStim therapy. The results were analyzed for comparison of the pharyngeal residue in the improved group and the non-improved group.
Results
A total of 59 patients concluded the test, in which 42 patients improved well enough to change the dietary methods while 17 did not improve sufficiently. Remnant area to total area (R/T) ratios of the valleculae before treatment in the improved group were 0.120, 0.177, and 0.101 for solid, soft, and liquid foods, respectively, whereas the ratios for the non-improved group were 0.365, 0.396, and 0.281, respectively. The ratios of the pyriformis sinuses were 0.126, 0.159, and 0.121 for the improved group and 0.315, 0.338, and 0.244 for the non-improved group. The R/T ratios of valleculae and pyriformis sinus were significantly lower in the improved group than the non-improved group in all food types before treatment. The R/T ratio cutoff values were 0.267, 0.250, and 0.185 at valleculae and 0.228, 0.218, and 0.185 at pyriformis sinuses.
Aspiration occurs sporadically in the general population, but when it becomes persistent, it is classified as a pathologic condition requiring evaluation and treatment of the cause [1]. One of the causes of aspiration is cerebrovascular disease and more than half of it is silent aspiration [2,3]. Diagnosing dysphagia by conducting videofluoroscopic evaluation and providing appropriate thickness of food as management is crucial [4]. There have been continuous studies objectively and quantitatively analyzing effects of the videofluoroscopic swallowing study (VFSS) [5,6,7]. One of the studies attempted to analyze the movement of the hyolaryngeal complex three-dimensionally to quantify the difficulty of swallowing [6]. Yet, evaluating the functional status only by the movement of the hyolaryngeal complex was difficult, and the result showed that pharyngeal movement was more important than the movement of the hyoid bone. In another study, scoring was conducted on the subsections, such as lip seal, penetration, and pharyngeal residue, to quantitatively analyze the process of swallowing [7]. This study suggested that the amount of pharyngeal residue is related to aspiration, and the study method was used where the amounts of pharyngeal residue were classified into four groups as follows: no residue and residue of below 10%, below 50%, and over 50%. However, this study method had no reference. Thus, this study attempted to confirm the cutoff value of the amount of pharyngeal residue when aspiration occurs.
Facilitative therapeutic approaches to stop aspiration, such as the Shaker exercise, have been studied [8]. Subsequent studies continually presented the neuromuscular electrical stimulation (NMES) as having as much effectiveness as traditional treatments. If combined with traditional treatment methods, the swallowing ability was shown to have more improvement than traditional treatment alone [9,10,11]. However, in conducting NMES, the predictive index on the improvement of dysphagia has not yet been distinctive. Thus, there is a need for an objective index which can help to predict this. Also, pharyngeal residues of valleculae and pyriformis sinuses, which are the index of dysphagia, are predictive factors of improvement when quantitatively measured through VFSS after the VitalStim treatment [12]. The authors confirmed this through a retrospective study.
Participants were in-patients of Yonsei University Wonju College of Medicine from January 2010 to February 2011, who satisfied the following criteria: 1) having first-ever-occurred strokes, 2) currently at less than sixty days since the onset of stroke, 3) sufficient dysphagic level to limit or modify dietary method to prevent complications, 4) sufficient cognitive level to follow instructions and communications, and 5) being capable of sitting with support to conduct VFSS which is the diagnosis evaluation.
The exclusion criteria were as follows: 1) recurrence of stroke; 2) past medical history of treating dysphagia with electrical stimulation; and 3) prohibiting factors of VitalStim, such as active neoplasm, implantable electrical devices, deep brain stimulator, vagal nerve stimulator, history of seizure, and inserted metallic transplant in current path.
Dysphagia was analyzed with VFSS using an X-ray generator (KXO-50N; Toshiba Co., Tokyo, Japan) and a fluoroscopy system (POPULUS So; Hitachi Medical Co., Tokyo, Japan), with the whole process videotaped with a hard disk camcorder (GZ-MG730 KR; Vitor Company of Japan Ltd., Yokohama, Japan). Aspiration was defined as when materials were observed below the vocal folds. Penetration was defined as barium crossing the upper plane of the laryngeal aditus (Fig. 1), or the imaginary line from the arytenoids cartilages to the aryepiglottic fold [1].
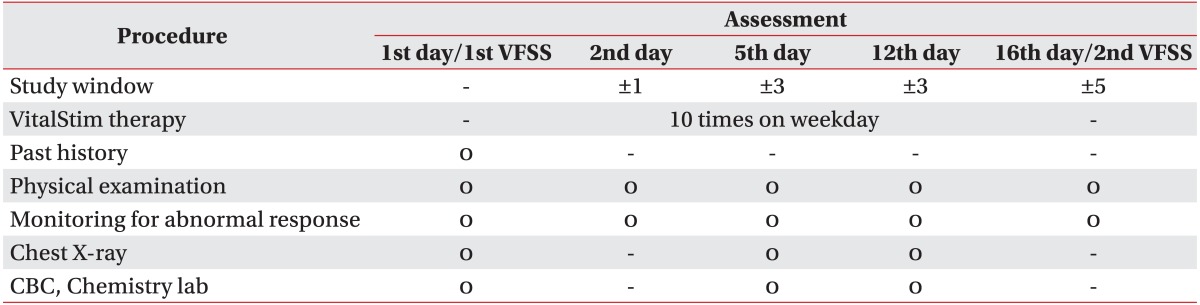
Participants were in-patients with strokes, who were capable of conducting VFSS and who required limitation or modification to their diet for the prevention of complications. After diagnosis, participants were treated with NMES using VitalStim one hour every day for two five-day weeks. A follow-up VFSS was conducted within three days after the two weeks of treatment (Table 1). Two rehabilitation medicine trainees and a rehabilitation specialist with twenty years of clinical experience formally deciphered the VFSS in solid/soft/liquid foods, in order to confirm the possibility of material modification and execution according to stage. After analyzing the medical records and VFSS results, the participants were classified into two groups based on the follow-up VFSS after treatment, which showed adequate or inadequate results in their ability to move on to higher level of food intake without aspiration.
Lateral VFSS images of individuals classified into two groups were analyzed using an image analysis program (ImageJ, http://imagej.nih.gov/ij/). Residues of valleculae and pyriformis sinuses were analyzed using remnant area to total area (R/T) ratio which is the proportion of residues of valleculae and pyriformis sinuses to their total spaces in solid/soft/liquid foods (Figs. 2, 3). Linear spreading test was done to check viscosity of food. The average value of the test was taken after repeating 10 times on glass plate using pipe containing specimen of 5 mL. Results were acquired after one minute of tilting the pipe that is 2 cm in diameter and height [13]. Pudding was used as solid food which showed 0.48 cm on linear spreading test. Soft food (rice porridge) showed 1.83 cm on linear spreading test. Liquid food which was yogurt with ioversol (Optiray 320; Mallinckrodt Korea Inc., Seoul, Korea) showed 5.27 cm. Classification of groups and calculation of the R/T ratio were done by a different individual to satisfy requirements of the double blind test.
To test the interpersonal reliability of the R/T ratio, two medical trainees were involved to confirm that there are no differences between their analysis results. The calculated R/T ratio was analyzed to find out whether the improved group and the non-improved group showed any differences before the treatment. Participants who failed to complete scheduled treatments were excluded from the analysis.
For the collected data, the independent variable was the presence of improvement in dysphagia and the dependent variable was the initial amount of residue in valleculae and pyriformis sinuses of the improved group and the non-improved group. With these variables, paired t-test was conducted using SPSS ver. 20.0 (IBM, Armonk, NY, USA), which is a statistical analysis program.
A total of 82 participants were initially enrolled in this study, but 10 participants had stroke recurrences, 4 had hemorrhagic transformation, and 9 withdrew due to transferring out of the institute or change of mind during the study. A total of 59 participants concluded this study. Among them, 42 participants improved enough to modify their food thickness and 17 did not show improvement enough to modify food. Thus, the improvement rate of VitalStim for dysphagic patients with stroke was 71.19%.
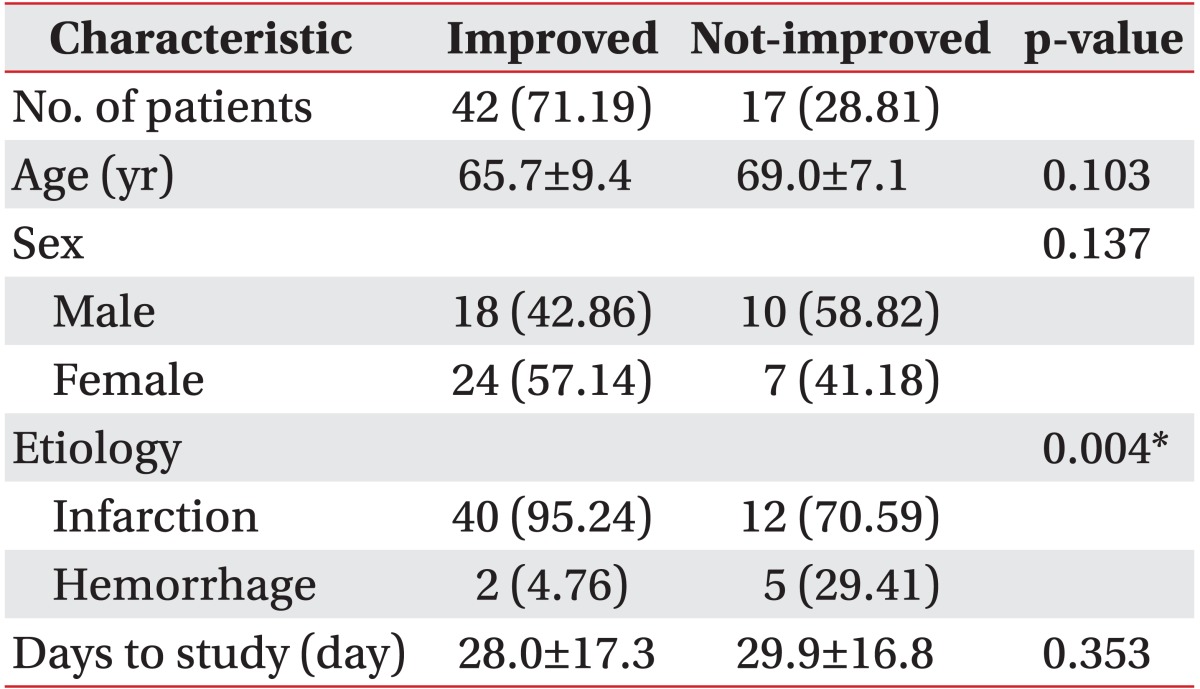
The average age was 65.7±9.4 years in the improved group and 69.0±7.1 years in the non-improved group, with no difference in statistical significance (p=0.103, p>0.05). Average number of days passed since the onset of stroke to the start of dysphagia treatment was 28.0±17.3 in the improved group and 29.9±16.8 in the non-improved group, which was not significantly different.
In the improved group, 18 were male and 24 were female. In the non-improved group, 10 were male and 7 were female. The number of each gender (p=0.137, p>0.05) in each group did not show any statistically significant difference (Table 2).
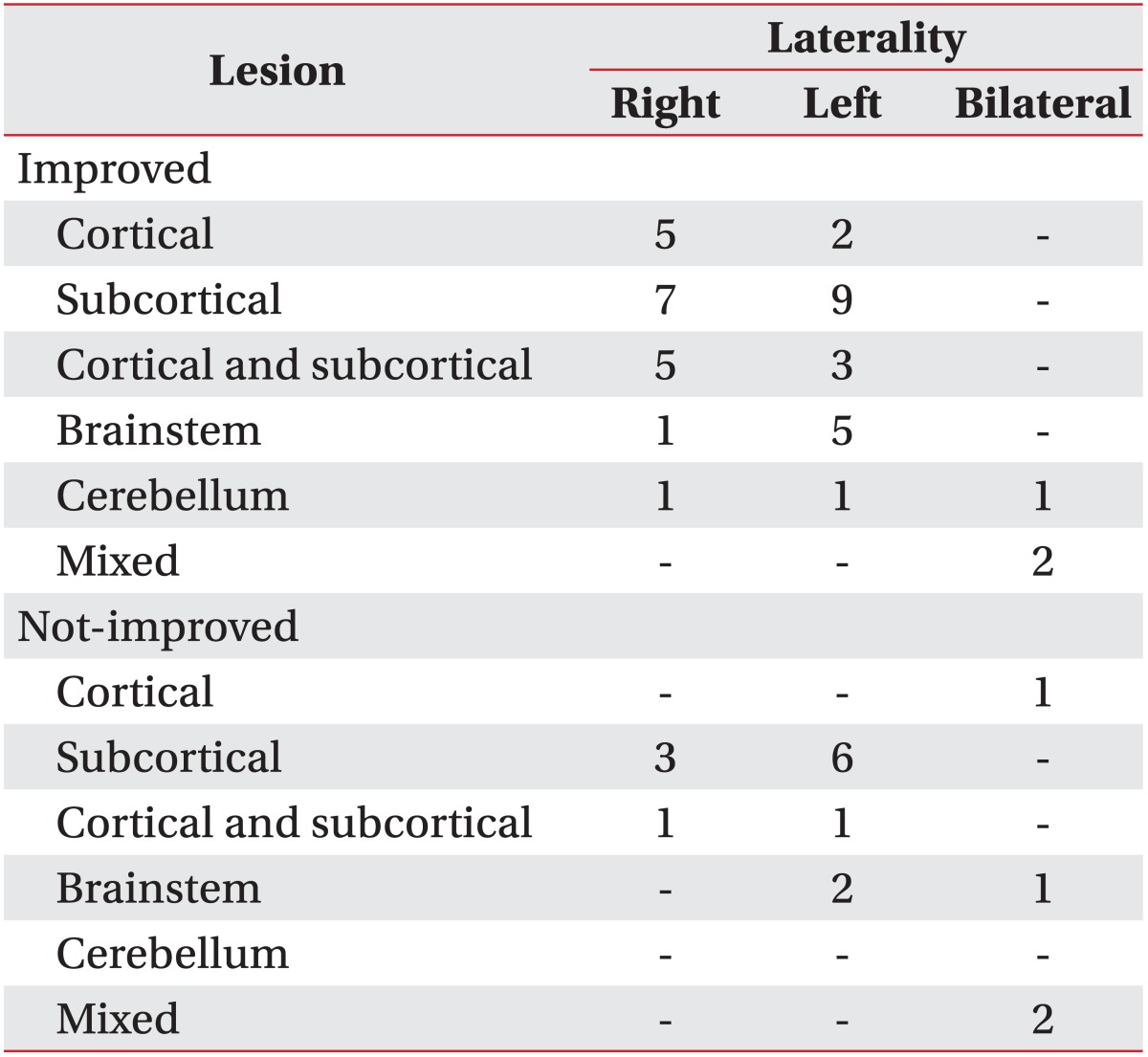
The improved group included 42 cases of cerebral infarction and 2 cases of intracranial hemorrhage, while the non-improved group included 20 cases of cerebral infarction and 5 cases of intracranial hemorrhage, showing a difference of statistical significance in the ratio of diseases (p=0.004, p<0.05) (Table 3).
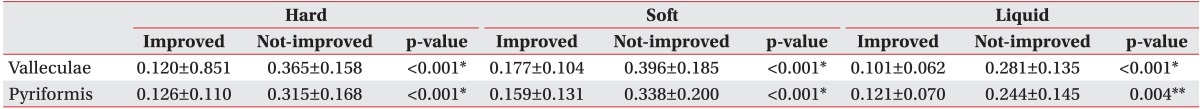
The inter-rater reliability was tested by intra-class correlation coefficient (ICC). The ICC was 0.920 in solid, 0.962 in soft, and 0.887 in liquid foods. The valleculae R/T ratio (improved group vs. non-improved group, 0.120±0.851/0.177±0.104/0.101±0.062 vs. 0.365±0.158/0.396±0.185/0.281±0.135) and the pyriformis sinuses R/T ratio (improved group vs. non-improved group, 0.126±0.110/0.159±0.131/0.121±0.070 vs. 0.315±0.168/0.338±0.200/0.244±0.145) showed statistical significance in solid/soft/liquid foods before treatment. The valleculae and pyriformis sinuses R/T ratio of the improved group was significantly smaller than that of the non-improved group in all solid (p<0.001), soft (p<0.001), and liquid foods (p<0.005) (Table 4).
Although it was not statistically significant, the difference in improvement of the R/T ratio after treatment was analyzed between male and female, since female ratio of the improved group was relatively high. As a result, improvement of the valleculae and pyriformis sinuses R/T ratio showed no significant difference between male and female in all solid/soft/liquid foods. Thus, no significant difference was found between male and female group in overall.
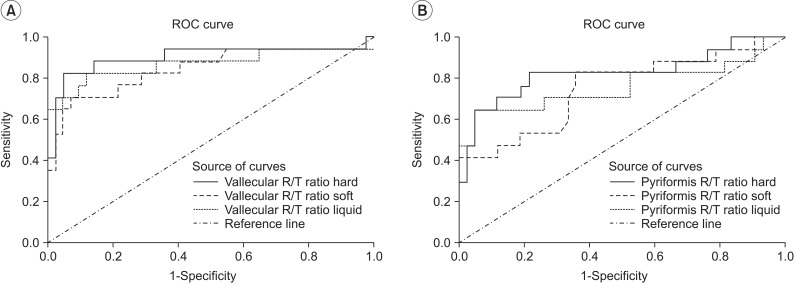
The cutoff value of the R/T ratio, which was used for predicting improvement after treatment with VitalStim, was determined based on sensitivity (Sn) and specificity (Sp) through the receiver operating characteristic (ROC) curve of each food type.
In valleculae, cutoff value of the R/T ratio was 0.267 (Sn 0.824; Sp 0.952) in solid, 0.250 (Sn 0.824; Sp 0.714) in soft, and 0.185 (Sn 0.824; Sp 0.881) in liquid foods (Fig. 4A). In pyriformis sinuses, cutoff value of the R/T ratio was 0.228 (Sn 0.824; Sp 0.786) in solid, 0.218 (Sn 0.824; Sp 0.643) in soft, and 0.185 (Sn 0.824; Sp 0.476) in liquid foods (Fig. 4B).
A previous study attempted to assess the amount of pharyngeal residue required for defining dysphagia. Although this proved the correlation between the two, it assessed the self-defined sections stage by stage and failed to quantitatively assess the amount of pharyngeal residue as a continuous variable [7]. However, with vague evidence of defining the section, our study attempted to quantitatively analyze the amount of residue which is clinically important. Since measuring the absolute amounts of pharyngeal residue is limited due to the variations in anatomical shape and size, we used the ratio of each patient's residue to anatomical structure as an objective parameter. As a result, although some differences existed among food types, the pharyngeal residues of the valleculae in the non-improved group were 36.5%-39.6% for solid and soft foods and 28.1% for liquid food. Also, the pharyngeal residues in the pyriformis sinuses were 31.5%-33.8% in solid and soft foods and 24.4% in liquid food. Residue of more than 1/3 of the total area for solid and soft foods and more than 1/4 for liquid food were expected to be a sign of not responding well to the treatment. Furthermore, the cutoff value of the R/T ratio of different food types was similar in solid and soft foods, but it was reduced significantly in liquid foods. This is considered to reflect the fact that people are more vulnerable to aspiration with liquid foods even with less pharyngeal residue.
There was no statistically significant difference in the decrease of R/T ratio after valleculae treatment between the improved group and the non-improved group. They were 0.062, 0.091, and 0.047 in the improved group and 0.061, 0.104, and 0.066 in the non-improved group. Degree of decrease of R/T ratios of the pyriformis sinuses also showed no statistically significant difference between the improved group and the non-improved group. They were 0.065, 0.078, and 0.058 in the improved group and 0.061, 0.104, and 0.066 in the non-improved group for solid, soft, and liquid foods, respectively.
Positive or negative correlation between valleculae and pyriformis sinuses R/T ratios was not observed in any same type of food.
According to review of literature, patients with intracranial hemorrhage showed more improvement than patients with cerebral infarction in Functional Independence Measure, Motor Assessment Scale, and gait velocity, whether or not their initial neurologic deficits were in similar levels [14,15]. However, it was impossible to confirm the difference in the level of improvement due to the etiology. A study on the predictive factors of improvement after cerebral infarction indicated that predictive improvement or degenerative factors had no statistical significance in the case of hemorrhagic transformation after cerebral infarction [16]. In this study, patients with intracranial hemorrhage were distributed more significantly in the non-improved group. Yet, in order to draw a conclusion that dysphagia shows unfavorable prognosis in intracranial hemorrhage than cerebral infarction, the design of the study should be more sophisticated. The above mentioned studies measured the degree of neurologic deficits, so the severity of dysphagia should be accurately measured and more cases should be added to show statistical significance.
Similar to other studies, the difference in sex did not affect the recovery from dysphagia, since the improvement of R/T ratio did not differ by sex as far as this study is concerned [14].
The term between the onset of stroke and the start of treatment was different from previous studies; it ranged from 20 days to 2 years. However, patients in the relatively early phase of stroke participated in this study, and interpreting and applying the results should be limited to subacute patient with dysphagia occurring due to stroke [7,8,9,10,11,16]. The treatment effectiveness of VitalStim on dysphagia due to subacute phase of stroke is considered to have clinical significance.
In the ROC curve, the pyriformis sinuses R/T ratio was similar in sensitivity, but the area under curve (AUR) and specificity were lower compared to the valleculae residue. This might be the result of error being measured with exaggeration in the smaller pyriformis sinuses area compared to valleculae area. The errors of pyriformis sinuses residual R/T ratio from analyzing only the lateral view of VFSS could be the limitations of this study, which could be more accurately measured in the AP view. Future studies are advised to measure the valleculae R/T ratio, to consider the fact that specificity of the pyriformis sinuses R/T ratio would decline when analyzing only the R/T ratio of the lateral image.
In conclusion, improvement in dysphagia after a stroke with NMES treatment (VitalStim) could be predicted by quantitatively measuring the residue per total area of valleculae and pyriformis sinuses through video-recording by VFSS.
References
1. Allen JE, White CJ, Leonard RJ, Belafsky PC. Prevalence of penetration and aspiration on videofluoroscopy in normal individuals without dysphagia. Otolaryngol Head Neck Surg. 2010; 142:208–213. PMID: 20115976.

2. Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, et al. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009; 18:329–335. PMID: 19717014.

3. Garon BR, Sierzant T, Ormiston C. Silent aspiration: results of 2,000 video fluoroscopic evaluations. J Neurosci Nurs. 2009; 41:178–185. PMID: 19678503.
4. Diniz PB, Vanin G, Xavier R, Parente MA. Reduced incidence of aspiration with spoon-thick consistency in stroke patients. Nutr Clin Pract. 2009; 24:414–418. PMID: 19483070.

5. Murguia M, Corey DM, Daniels SK. Comparison of sequential swallowing in patients with acute stroke and healthy adults. Arch Phys Med Rehabil. 2009; 90:1860–1865. PMID: 19887209.

6. Kim Y, McCullough GH. Maximal hyoid excursion in poststroke patients. Dysphagia. 2010; 25:20–25. PMID: 19655199.

7. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–682. PMID: 11346847.

8. Logemann JA, Rademaker A, Pauloski BR, Kelly A, Stangl-McBreen C, Antinoja J, et al. A randomized study comparing the Shaker exercise with traditional therapy: a preliminary study. Dysphagia. 2009; 24:403–411. PMID: 19472007.

9. Carnaby-Mann GD, Crary MA. Examining the evidence on neuromuscular electrical stimulation for swallowing: a meta-analysis. Arch Otolaryngol Head Neck Surg. 2007; 133:564–571. PMID: 17576907.
10. Blumenfeld L, Hahn Y, Lepage A, Leonard R, Belafsky PC. Transcutaneous electrical stimulation versus traditional dysphagia therapy: a nonconcurrent cohort study. Otolaryngol Head Neck Surg. 2006; 135:754–757. PMID: 17071307.

11. Shaw GY, Sechtem PR, Searl J, Keller K, Rawi TA, Dowdy E. Transcutaneous neuromuscular electrical stimulation (VitalStim) curative therapy for severe dysphagia: myth or reality? Ann Otol Rhinol Laryngol. 2007; 116:36–44. PMID: 17305276.

12. Kelly AM, Macfarlane K, Ghufoor K, Drinnan MJ, Lew-Gor S. Pharyngeal residue across the lifespan: a first look at what's normal. Clin Otolaryngol. 2008; 33:348–351. PMID: 18983345.

13. Han TR, Shin HI, Park JW, Park IC. The effects of viscosity on oropharyngeal phase. J Korean Acad Rehabil Med. 2001; 25:236–240.
14. Paolucci S, Antonucci G, Grasso MG, Bragoni M, Coiro P, De Angelis D, et al. Functional outcome of ischemic and hemorrhagic stroke patients after inpatient rehabilitation: a matched comparison. Stroke. 2003; 34:2861–2865. PMID: 14615613.
15. Katrak PH, Black D, Peeva V. Do stroke patients with intracerebral hemorrhage have a better functional outcome than patients with cerebral infarction? PM R. 2009; 1:427–433. PMID: 19627929.

16. Kumar S, Doughty C, Doros G, Selim M, Lahoti S, Gokhale S, et al. Recovery of swallowing after dysphagic stroke: an analysis of prognostic factors. J Stroke Cerebrovasc Dis. 2014; 23:56–62. PMID: 23102742.

Fig. 1
Aspiration is defined as presence of material below the vocal folds (double line). Penetration is defined as barium crossing the upper plane of the laryngeal aditus (single line), or the imaginary line from the arytenoid cartilages (short arrow) to the aryepiglottic fold (long arrow).
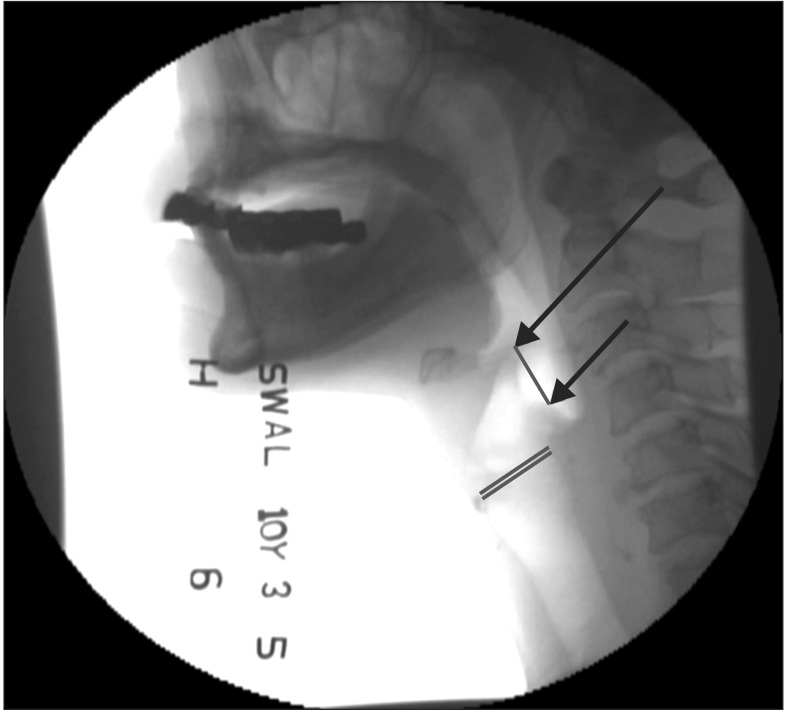
Fig. 2
Vallecular remnant area to total area ratio is defined as proportion of residue areas of valleculae (A) to their total space (B) viewed on lateral image of videofluoroscopic swallowing study.
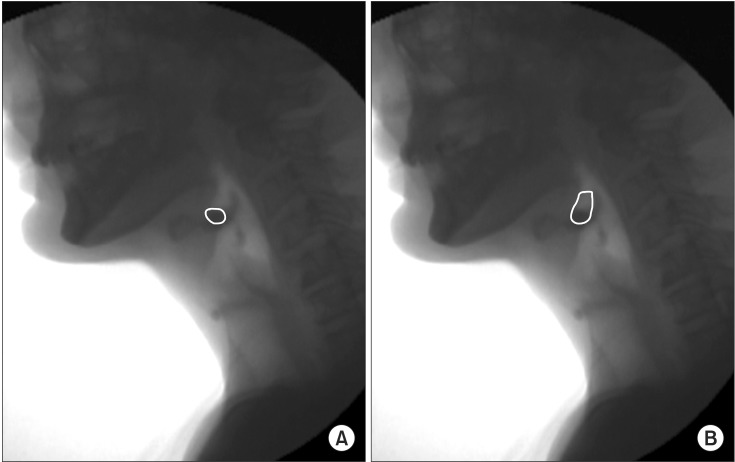
Fig. 3
Pyriformis remnant area to total area ratio is defined as proportion of residue areas of pyriformis sinuses (A) to their total space (B) viewed on lateral image of videofluoroscopic swallowing study.
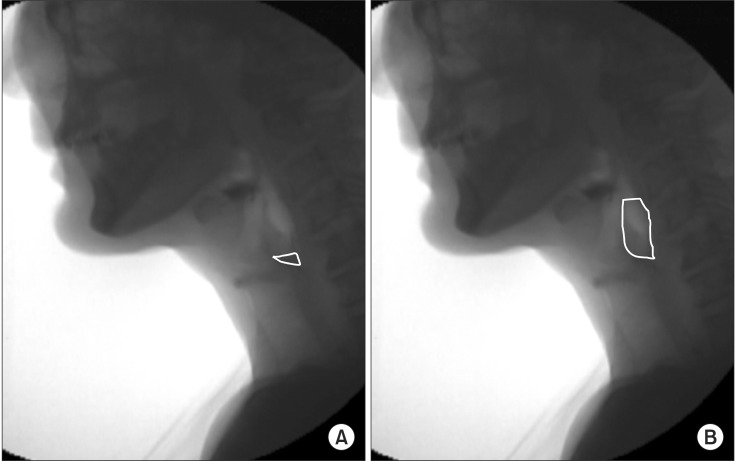
Fig. 4
ROC curve shows remnant area to total area (R/T) ratio to be a good screening test for the prediction of effectiveness of NMES therapy for dysphagia at valleculae (A) and pyriformis (B). ROC, receiver operating characteristic; NMES, neuromuscular electrical stimulation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download