1. Cho NH, Jung YO, Lim SH, Chung CK, Kim HA. The prevalence and risk factors of low back pain in rural community residents of Korea. Spine (Phila Pa 1976). 2012; 37:2001–2010. PMID:
22588379.

2. Badley EM, Rasooly I, Webster GK. Relative importance of musculoskeletal disorders as a cause of chronic health problems, disability, and health care utilization: findings from the 1990 Ontario Health Survey. J Rheumatol. 1994; 21:505–514. PMID:
8006895.
3. Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992; 5:383–389. PMID:
1490034.

4. Panjabi MM. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord. 1992; 5:390–396. PMID:
1490035.

5. Bergmark A. Stability of the lumbar spine: a study in mechanical engineering. Acta Orthop Scand Suppl. 1989; 230:1–54. PMID:
2658468.
6. Saal JA. The new back school prescription: stabilization training. Part II. Occup Med. 1992; 7:33–42. PMID:
1531892.
7. Hodges PW, Richardson CA. Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Arch Phys Med Rehabil. 1999; 80:1005–1012. PMID:
10489000.

8. Danneels LA, Coorevits PL, Cools AM, Vanderstraeten GG, Cambier DC, Witvrouw EE, et al. Differences in electromyographic activity in the multifidus muscle and the iliocostalis lumborum between healthy subjects and patients with sub-acute and chronic low back pain. Eur Spine J. 2002; 11:13–19. PMID:
11931058.

9. MacDonald D, Moseley GL, Hodges PW. Why do some patients keep hurting their back? Evidence of ongoing back muscle dysfunction during remission from recurrent back pain. Pain. 2009; 142:183–188. PMID:
19186001.

10. Sihvonen T, Lindgren KA, Airaksinen O, Manninen H. Movement disturbances of the lumbar spine and abnormal back muscle electromyographic findings in recurrent low back pain. Spine (Phila Pa 1976). 1997; 22:289–295. PMID:
9051891.

11. Ferreira PH, Ferreira ML, Hodges PW. Changes in recruitment of the abdominal muscles in people with low back pain: ultrasound measurement of muscle activity. Spine (Phila Pa 1976). 2004; 29:2560–2566. PMID:
15543074.
12. Hides JA, Stanton WR, McMahon S, Sims K, Richardson CA. Effect of stabilization training on multifidus muscle cross-sectional area among young elite cricketers with low back pain. J Orthop Sports Phys Ther. 2008; 38:101–108. PMID:
18349481.

13. O'Sullivan PB, Phyty GD, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine (Phila Pa 1976). 1997; 22:2959–2967. PMID:
9431633.
14. Richardson CA, Jull GA. Muscle control-pain control. What exercises would you prescribe? Man Ther. 1995; 1:2–10. PMID:
11327788.

15. Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine (Phila Pa 1976). 2001; 26:E243–E248. PMID:
11389408.

16. Porcari JP, Miller J, Cornwell K, Foster C, Gibson M, McLean K, et al. The effects of neuromuscular electrical stimulation training on abdominal strength, endurance, and selected anthropometric measures. J Sports Sci Med. 2005; 4:66–75. PMID:
24431963.
17. Alon G, McCombe SA, Koutsantonis S, Stumphauzer LJ, Burgwin KC, Parent MM, et al. Comparison of the effects of electrical stimulation and exercise on abdominal musculature. J Orthop Sports Phys Ther. 1987; 8:567–573. PMID:
18797021.

18. Coghlan S, Crowe L, McCarthyPersson U, Minogue C, Caulfield B. Electrical muscle stimulation for deep stabilizing muscles in abdominal wall. Conf Proc IEEE Eng Med Biol Soc. 2008; 2008:2756–2759. PMID:
19163276.

19. Coghlan S, Crowe L, McCarthyPersson U, Minogue C, Caulfield B. Neuromuscular electrical stimulation training results in enhanced activation of spinal stabilizing muscles during spinal loading and improvements in pain ratings. Conf Proc IEEE Eng Med Biol Soc. 2011; 2011:7622–7625. PMID:
22256103.

20. Glaser JA, Baltz MA, Nietert PJ, Bensen CV. Electrical muscle stimulation as an adjunct to exercise therapy in the treatment of nonacute low back pain: a randomized trial. J Pain. 2001; 2:295–300. PMID:
14622808.

21. Baek SO, Cho HK, Jung GS, Son SM, Cho YW, Ahn SH. Verification of an optimized stimulation point on the abdominal wall for transcutaneous neuromuscular electrical stimulation for activation of deep lumbar stabilizing muscles. Spine J. 2014; 2. 14. [in press].
http://dx.doi.org/10.1016/j.spinee.2014.02.016.

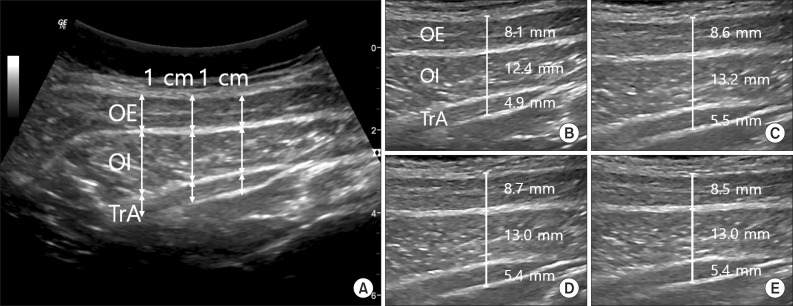
22. Hodges PW, Pengel LH, Herbert RD, Gandevia SC. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve. 2003; 27:682–692. PMID:
12766979.

23. Koppenhaver SL, Fritz JM, Hebert JJ, Kawchuk GN, Parent EC, Gill NW, et al. Association between history and physical examination factors and change in lumbar multifidus muscle thickness after spinal manipulation in patients with low back pain. J Electromyogr Kinesiol. 2012; 22:724–731. PMID:
22516351.

24. Hebert JJ, Koppenhaver SL, Parent EC, Fritz JM. A systematic review of the reliability of rehabilitative ultrasound imaging for the quantitative assessment of the abdominal and lumbar trunk muscles. Spine (Phila Pa 1976). 2009; 34:E848–E856. PMID:
19927091.

25. Hodges PW, Richardson CA. Contraction of the abdominal muscles associated with movement of the lower limb. Phys Ther. 1997; 77:132–144. PMID:
9037214.

26. Hides JA, Richardson CA, Jull GA. Magnetic resonance imaging and ultrasonography of the lumbar multifidus muscle: comparison of two different modalities. Spine (Phila Pa 1976). 1995; 20:54–58. PMID:
7709280.
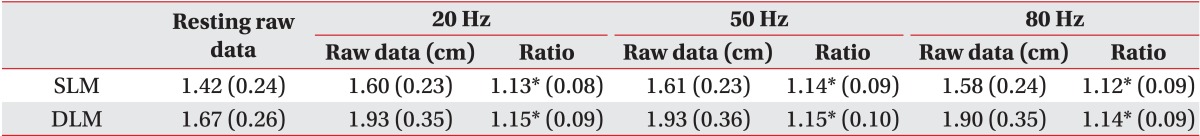
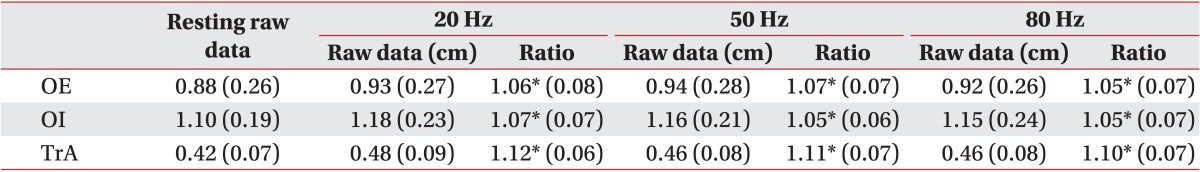
27. Sbruzzi G, Schaan BD, Pimentel GL, Signori LU, Da Silva AN, Oshiro MS, et al. Effects of low frequency functional electrical stimulation with 15 and 50 Hz on muscle strength in heart failure patients. Disabil Rehabil. 2011; 33:486–493. PMID:
20597628.

28. Kramer JF. Effect of electrical stimulation current frequencies on isometric knee extension torque. Phys Ther. 1987; 67:31–38. PMID:
3797474.

29. Hainaut K, Duchateau J. Neuromuscular electrical stimulation and voluntary exercise. Sports Med. 1992; 14:100–113. PMID:
1509225.

30. Halback J, Straus D. Comparison of electro-myo stimulation to isokinetic training in increasing power of the knee extensor mechanism. J Orthop Sports Phys Ther. 1980; 2:20–24. PMID:
18810165.

31. Delitto A, Brown M, Strube MJ, Rose SJ, Lehman RC. Electrical stimulation of quadriceps femoris in an elite weight lifter: a single subject experiment. Int J Sports Med. 1989; 10:187–191. PMID:
2674035.

32. Gondin J, Cozzone PJ, Bendahan D. Is high-frequency neuromuscular electrical stimulation a suitable tool for muscle performance improvement in both healthy humans and athletes? Eur J Appl Physiol. 2011; 111:2473–2487. PMID:
21909714.







 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download