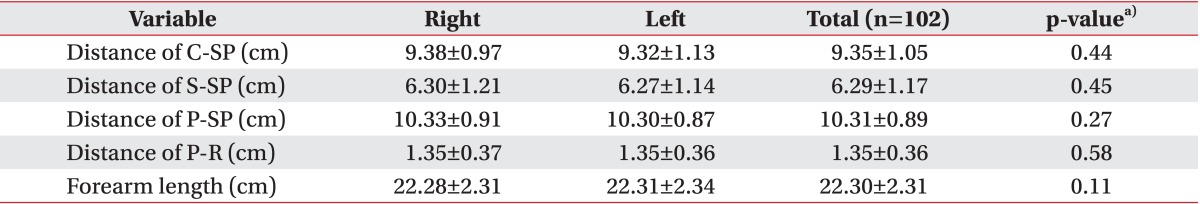
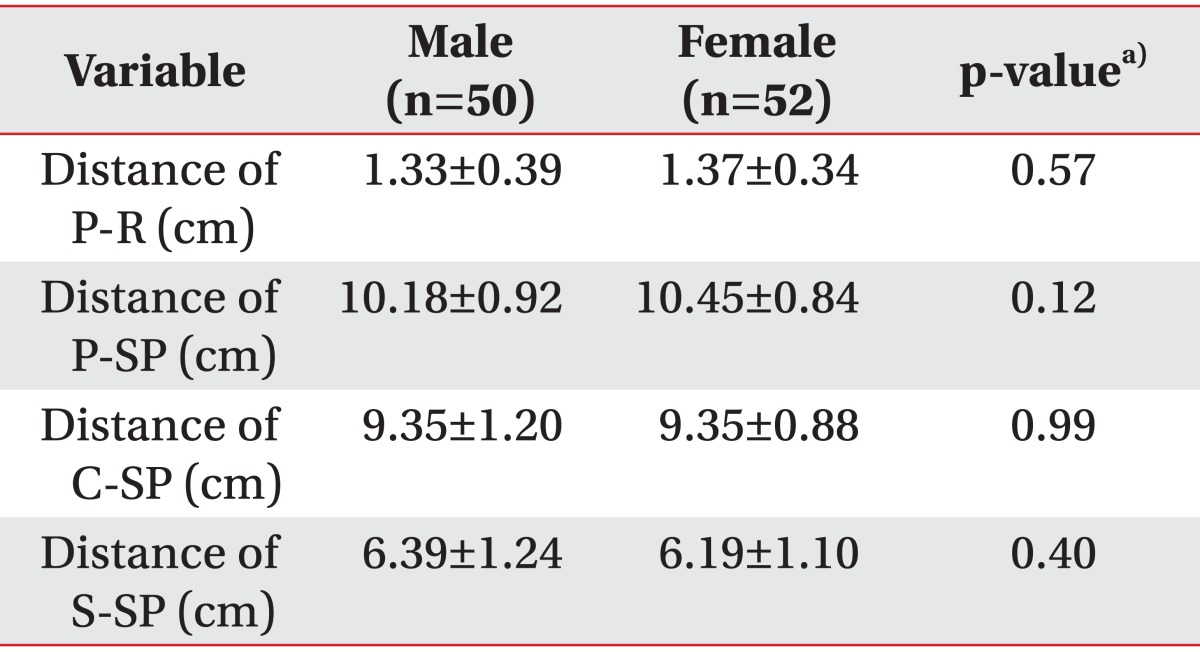
The present study was conducted to evaluate the SRN and the CV in the forearm by ultrasonography and revealed the close anatomical relationship between the SRN and the CV in the distal forearm. The SRN started to contact the CV at 9.35±1.05 cm distance from the RSP and was separated from the CV at 6.29±1.17 cm distance from the RSP.
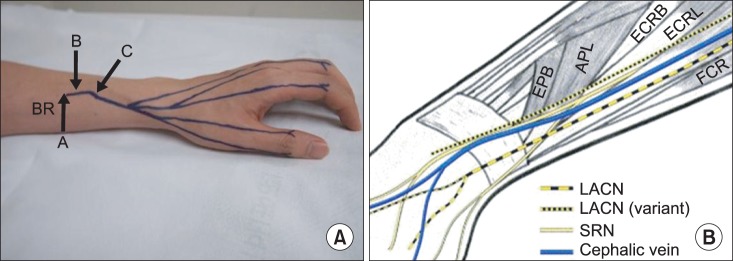
The SRN emerges just dorsal to the brachioradialis muscle in the mid-forearm, and it terminates in fine sensory branches at the level of the wrist and over the dorsum of the hand [
6]. Injury to this nerve results in a variable area of anesthesia that may include the dorsal surfaces of the proximal halves of the thumb, index, and middle fingers. It is usually limited to a triangular area on the dorsum of the web between the first and second metacarpal [
2]. Although the distribution of the SRN has been described in anatomic textbooks, the characteristics of its pathway which are related to its clinical importance have not been clearly demonstrated. Also, the majority of the studies have been focused on the SRN of cadavers. In one study on anatomic variation of SRN using cadavers, the SRN became subcutaneous at a mean of 9.20 cm and bifurcated at a mean of 4.90 cm proximal to the styloid process of the radius in 48 specimens [
7]. Another anatomic study of the SRN and the CV in 14 hands from 10 cadavers reported that the mean distance from the styloid process of radius to the point at which the SRN pierced fascia was 79.9±9.84 mm (range, 60 to 93 mm) and from the styloid process of radius to the crossing point of the SRN with the CV was 29.5±15.24 mm (range, 13 to 55 mm) [
4]. These findings that are inconsistent with the present study may be due to a distinction between cadavers and living subjects. The cadaveric study could have a measurement error because of the transposition of anatomic structures, especially of such structures as subcutaneous nerves or vessels, occurring during dissection. In contrast, ultrasound is able to search the anatomic constructions without transposition. In addition, there is some benefit of the ultrasonographic evaluation. It provides anatomic information not available with electrodiagnostic studies, and it is readily available, is inexpensive, does not involve radiation exposure, and is painless [
8]. It can provide information about nerve structure to help assess nerve pathologies. Many studies have reported the usefulness of ultrasonography to investigate nerve diseases [
9]. On the other hand, acquisition of accurate ultrasonographic images depends on the operator. Our ultrasound scanning of both SRN was performed by a single sonographer, so inter-rater reliability was not evaluated. Also due to the size of SRN being very small, technical errors, like misinterpretation, can occur. These might have effected a discrepancy between this study and the cadaveric study. Injury to the SRN has been reported after trauma and surgery [
10] and during routine peripheral vein cannulation. Injury resulted in the development of a neuroma and considerable discomfort and disability [
2]. According to a recent study on the histological and ultrasonographical findings of the SRN, with advancing age, the changes in SRN intraneural anatomy were noticed in the form of an increased amount of adipose tissue in the interfascicular domains. These findings may help to explain poor prognosis with advancing age following repair [
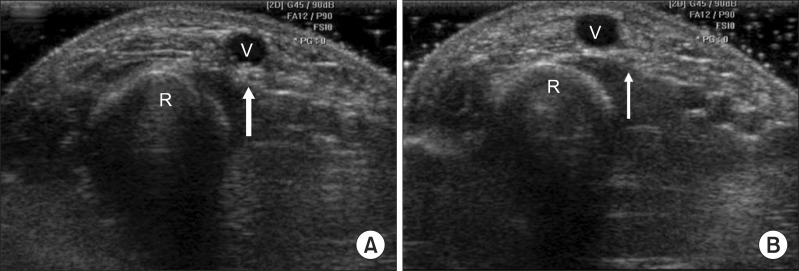
11]. In another study on nerve evaluation using ultrasonography, most nerves in the upper extremity showed a clear fascicular pattern similar to that of a honeycomb. However, according to other reports, small nerves, such as the superficial radial or posterior interosseous nerve, appeared as only 1 hypoechoic fascicle with an oval shape [
9].
To our knowledge, this is the first attempt to evaluate the anatomic relationship between the SRN and the CV in living subjects through ultrasonographic examination. The current study demonstrated the close anatomical relationship between the SRN and the CV in the distal forearm through ultrasonography. This implies that the cephalic venipuncture in the distal forearm requires close attention to the possibility of the SRN injury. Furthermore, we investigated the point where the SRN pierced the brachioradialis fascia and became subcutaneous. This result provides the appropriate stimulation site in an SRN conduction study for optimal response of sensory nerve action potentials.
This study has several limitations. First, most participants were Asian and of old age with relatively short statures which could influence the forearm length and the results. Second, the SRN and the CV were measured with the forearm in neutral position only. There is a possibility of a change in the measurement data according to the forearm position, such as pronation. Further studies are necessary regarding this matter. Nonetheless, all of the participants thoroughly completed the ultrasonographic examination without any particular adverse effects.
In conclusion, the SRN has close approximation to the CV in the distal second quarter of the forearm in ultrasonographic examination. We recommend that cephalic venipuncture had better be avoided in this area, that is, the crossing point of the SRN with the CV. If needed, it should be carried out with caution not to cause injury to the SRN. Also, when physicians perform nerve conduction studies of the SRN, the stimulation point within about 10 cm proximal to the styloid process of radius is recommend.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download