Abstract
A ganglion cyst is a relatively common benign tumor on the wrist. Conservative and surgical approaches have been used for its treatment. Various conservative treatment methods have been suggested such as reassurance, aspiration, sclerosant injection, and direct compression. But, there is no acceptable treatment of choice yet because each suggested method has a relatively high recurrence rate. We want to report two cases in which the size of the wrist ganglion was decreased by using electroacupuncture. One patient presented with a chronic ganglion for six years and the other patient presented with a recently occurred acute ganglion. We applied electroacupuncture for 20 minutes once a week for eight weeks to both of them. Afterwards, the size of the wrist ganglion diminished in the follow-up sonography and the accompanying pain was also relieved. Herein we report both cases along with a review of the relevant literature.
Go to : 
Ganglion is a cystic benign tumor of the hand, usually on the wrist. It is known as one of the most common soft tissue tumors of the hand, wrist, and foot. Most ganglia are asymptomatic, but swelling, pain and restriction of the joint motion may be shown in some cases [1,2] and may affect the activities of daily living. The clinical findings are sufficient in almost all cases to describe a ganglion. However, some imaging methods, such as ultrasonography and magnetic resonance imaging, may be helpful for a diagnosis [2].
So far, many methods that involve either surgical or conservative approaches, such as observation, percutaneous aspiration, sclerotherapy, and surgery, have been reported for the treatment of ganglions [2]. However of the current conservative remedies, there is none with a clear remedial value. This seems to be caused by the obscure pathophysiology.
In 2006, Tekeoglu and Dogan [3] presented a case of electroacupuncture treatment in a patient with a wrist ganglion. At this time point was electroacupuncture a not existing remedy. In both herein presented cases, we tried this method to determine the effect of electroacupuncture on ganglions.
Go to : 
A 16-year-old female patient visited our outpatient clinic because of a six-year-old left wrist mass and pain that occurred accidentally, without any special traumatic history. According to the patient's history, the mass was first detected on her left wrist dorsal area when she was 10 and the mass had grown increasingly bigger since then. She was first diagnosed with a ganglion cyst at other hospitals, but the conservative treatment was not effective. An open excision was implemented four years later. However, the cyst recurred and gradually became bigger about six months after the operation. One year after the operation, an aspiration was implemented and even a steroid injection was executed. However, the mass still became bigger and the pain grew stronger, so the patient eventually came to our hospital.
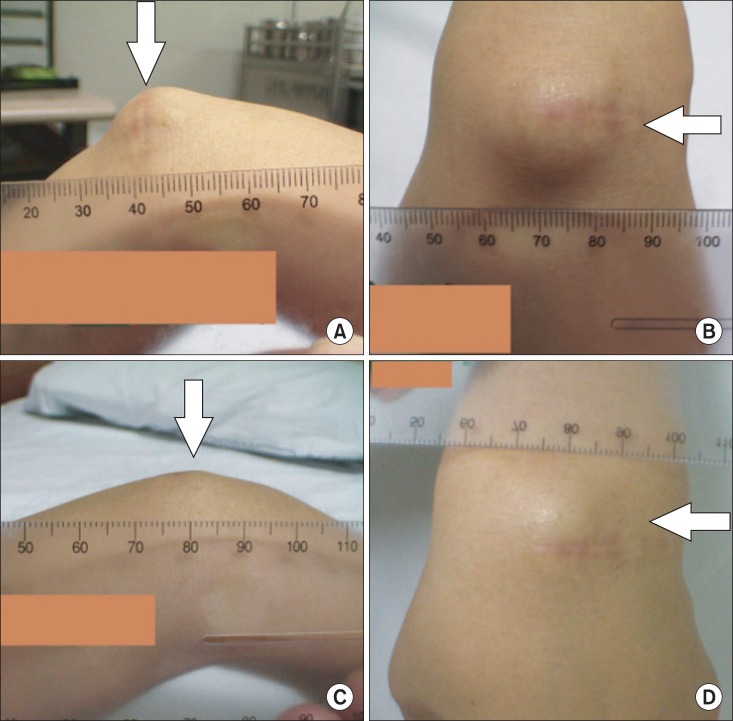
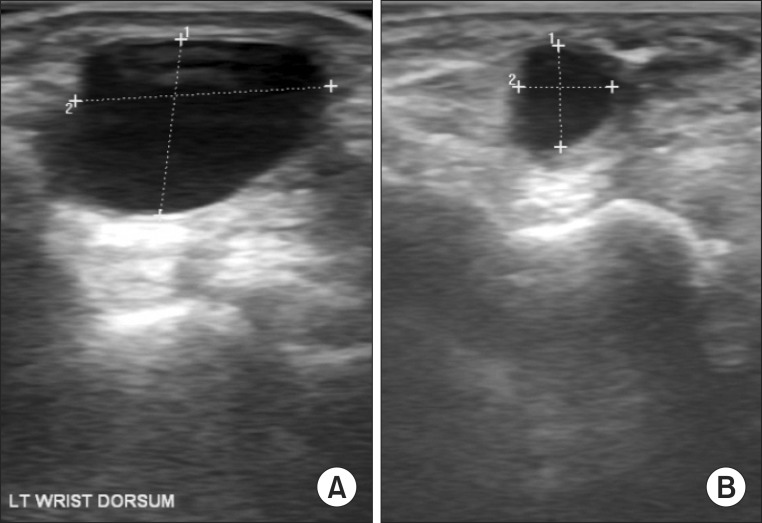
A visible mass with a surgery scar was detected on her left wrist dorsum upon physical examination (Fig. 1A, B). The mass felt very similar to a firm rubber ball and was well tethered in place. Tenderness was not clear at palpation. Neither heating sense nor erythema was seen and no pulsation was felt. The range of motion (ROM) of the left wrist showed a 50° limit of flexion and the patient expressed an excruciating pain from 30° on between point 6 and 7 on the visual analogue scale (VAS). Her left wrist extension was slightly limited to 50°. The manual muscle testing (MMT) of the wrist flexion was diminished at the 3+/5 point, possibly because of the influence of pain, and the wrist extension was evaluated as 4/5. The sensory examination results were normal. No fracture, bony erosion and osteophyte were seen on the simple X-ray of the wrist. The blood test also showed a normal erythrocyte sedimentation rate (ESR) of 3 mm/hr, C-reactive protein (CRP) of 0.1 gm/dL, and anti-cyclic citrullinated peptides (anti-CCP) of 0.1 U/mL. No cervical radiculopathy or carpal tunnel syndrome was observed in the electromyography. A 1.46×1.01-cm cystic mass was observed on the left wrist dorsum area via ultrasonography (Fig. 2A).
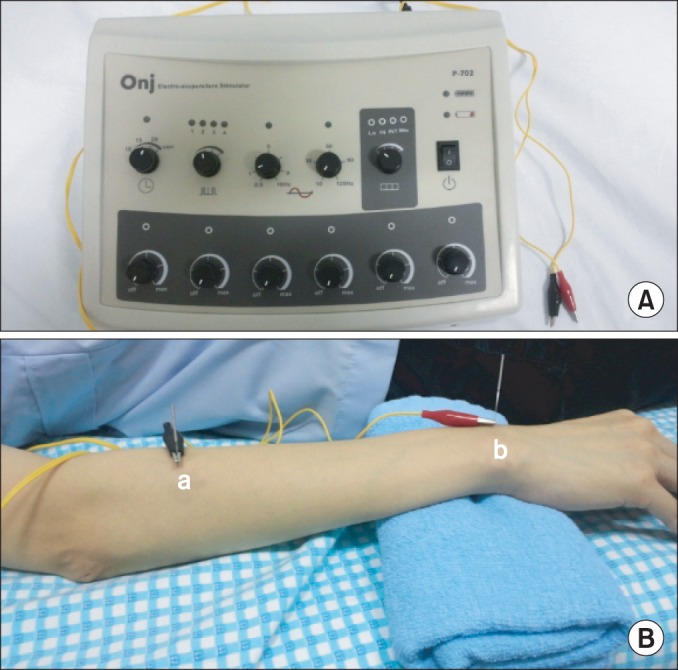
We first explained the procedure to the patient and obtained her consent for the experimental method. We used ONJ P-702 (Hyumedi, Seoul, Korea) as electroacupuncture equipment (Fig. 3A). The size of the sterile needle was 0.35×30 mm. The patient maintained a supine position with 20° shoulder abduction, 15° elbow flexion, full-ROM forearm pronation, and 10° wrist flexion by using the roll. One of the needles was located on the muscle belly of the extensor digitorum communis muscle and the other was located on the ganglion site (Fig. 3B). The electroacupuncture was connected to the needle and implemented for 20 minutes with 1 Hz direct current. The intensity of the current was increased to the highest degree that could be tolerated by the patient.
The patient received the procedure once a week for eight times' altogether. The decrease of ganglion size could be seen with bare eyes after eight weeks (Fig. 1C, D). The size was diminished to 0.53×0.58 cm in the follow-up ultrasonography (Fig. 2B) and the left wrist pain improved to point 2 on the VAS scale. The left wrist flexion ROM recovered to 80°. The wrist flexion and extension MMT also improved to 5/5 and the procedure was halted after the patient expressed her satisfaction.
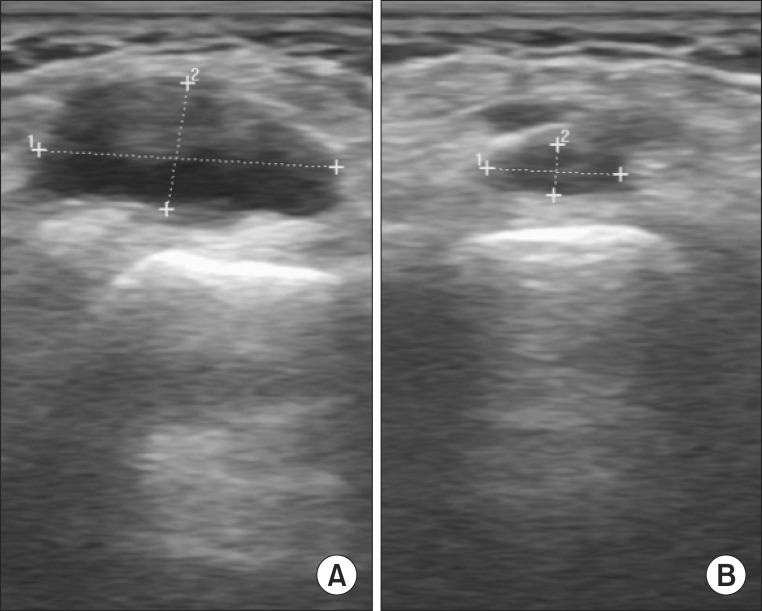
A 52-year-old female homemaker patient visited our clinic. Her main complaint was a mass on her right wrist dorsum that she accidentally discovered a month earlier. The patient reported her wrist was bent while it was pressed against her body five or six years earlier and she had been experiencing intermittent wrist pain since then. The pain increased when she used her wrist to wipe something with a cloth or when she held a mouse for too long. A visible soft mass well tethered in place that felt like a firm rubber ball was observed on her right wrist dorsum area upon physical examination. No inflammation signs, such as a heat sensation or erythema, were observed and the tenderness was not prominent. The wrist flexion/extension ROM were normal at 90°/70° and the pain degree was point 5 at the VAS scale with a wrist flexion of 45°. Both, the right wrist flexion and the extension MMT were evaluated as 4/5. The sensory examination results were normal. No fracture line, bony spur or bone erosion was observed in the simple X-ray of the right wrist. The blood tests also showed normal results with ESR 5 mm/hr, CRP 0.4 gm/dL, and anti-CCP 0.5 U/mL. The size of the cyst was determined as 1.45×0.62 cm in the ultrasonography (Fig. 4A).
As in case 1, we explained the procedure to the patient and obtained her consent on the experimental method. She received electroacupuncture once a week for 20 minutes eight times altogether. Eight weeks later, the cyst shrunk to 0.64×0.25 cm as seen in the ultrasonography (Fig. 4B), and the degree of the wrist pain dropped to point 1 on the VAS. The MMT also improved to 5/5 on both the wrist flexion and extension, and the procedure was halted after the patient expressed satisfaction.
Go to : 
A wrist ganglion occurs relatively often and can be diagnosed relatively easy by clinical symptoms. But, many parts of ganglion are still not well identified as compared with the incidence rate or easiness of diagnosis. They are typically seen in the second through the fourth decades of life. Women are three times more likely to be affected than men. Wrist ganglions usually occur on the dorsal wrist over the scapholunate interval and on the volar wrist over the radioscaphoid articulation. In contrast, the etiology of ganglions is unknown. There are no known occupational risk factors and the pathophysiology remains still unclear. As a result, the treatment of choice is not precisely known yet [1].
In 2006, Tekeoglu and Dogan [3] announced the implementation of electroacupuncture on a 53-year-old female patient with a five-year-old wrist ganglion. She was treated four times in two weeks and no recurrence was reported until a year after the follow-up. In our cases, the decrease in the ganglion size could be attributed to the implementation of electroacupuncture in both patients based on this report. Especially in the case of the 16-year-old student whose ganglion recurred even after aspiration, steroid injection and open excision operation, the decrease in the mass size was observed with bare eyes only after eight weeks of electroacupuncture implementation. The electroacupuncture approach for the treatment of patients with ganglion has the following advantages: 1) it does not have special adverse effects; 2) it does not require the patient to take time off from work, unlike as in case of surgery; and 3) it shows good compliance because the procedure is painless. This seems to be a method worthy of further research on the statistical meaning of the remedial effects or the optimal parameters, such as the frequency, intensity and stimulation type of the treatment method. Moreover, the recurrence rate should be further evaluated through long-term follow-ups.
The pathophysiology of ganglion cysts is still unclear, although multiple theories have been proposed. These cysts were initially believed to occur as a result of a synovial herniation, but the lack of a cellular synovial lining makes this theory unlikely [1,4,5]. Microscopically, the pedicle contains a tortuous lumen that connects the cyst to the underlying joint. According to the report of Andren and Eiken [4] in 1971, in two-thirds of patients in whom carpal arthrography was performed, the contrast medium was filled with ganglions and had a tortuous narrow duct connection. On the other hand, no such connection could be demonstrated in case of injection into the ganglion. Thus, a one-way valve mechanism has been postulated.
Evaluations via electron microscopy demonstrated that these are most likely fibroblasts or some other type of mesenchymal cell and did not, in any way, appear to be cells of synovial origin [6]. The analysis of the cystic fluid revealed that it is a gelatinous material that contains mainly hyaluronic acid and lesser amounts of glucosamine, globulins, and albumen. This fluid is biochemically different and is much thicker than the intra-articular synovial fluid [5].
Based on these, three theories are still being actively discussed. First, a rent in the joint capsule or tendon sheath allows the leakage of synovial fluid, which irritates the surrounding tissue. This local tissue reacts by forming a pseudocapsule and subsequently, a ganglion. The reaction between this tissue and the synovial fluid produces the ganglion fluid [1]. Second, joint stress may lead to a mucinous degeneration of the adjacent extra-articular connective tissue with subsequent fluid accumulation and eventual cyst formation. This theory holds that the cyst and the pedicle form a direct connection to the joint only after the creation of the cyst [1,5]. Third, some theorize that stress, such as stretching of the capsular and ligamentous supporting joint structures, stimulates the production of mucin, which produces cells that may be modified synovial cells, mesenchymal cells or fibroblasts, all of which have been shown to produce hyaluronic acid [5].
Despite the several limits, our both experienced cases arouse curiosity about the mechanism of the meaningful diminution of the wrist ganglion size. Tekeoglu and Dogan [3], as the first to report on this method, inferred that its mechanism includes acute local vasoconstriction followed by vasodilation from the release of mediators, such as bradykinin, acetylcholine, and leukotrienes [3]. However, it was difficult to think that only the vasomotor function directly influenced the diminution of the ganglion size.
We have inferred a few mechanisms from papers of various fields. First, in 1998, Reed [7] reported that electrical simulation can affect the microvascular permeability in the decrease of edema. According to this report, the electric current could have been involved in the fluid absorption of the ganglion by affecting the cell membrane permeability. Second, in 2012, Hwang et al. [8] announced that the human mesenchymal cell can influence the tissue regeneration due to the effect of electrical stimulation on it. In this report, the electrical stimulation enhanced the gene expression of growth factors (bone morphogenetic protein 2, insulin-like growth factor 1, vascular endothelial growth factor), chemokines (chemokine (C-X-C motif ) ligand 2), interleukin-8, and chemokine receptors (C-X-C chemokine receptor type 4, interleukin-8 receptor and beta). Various chemokines and growth factors may regulate the microenvironment, accelerate the chemotaxis, and may result in the differentiation of mesenchymal cells into specific cells [8]. Among the various hypotheses on the mechanism of the cystic fluid formation in a ganglion, one states that an undifferentiated mesenchymal cell in the ganglion cyst wall may be the origin of the mucin production [5]. As electrical stimulation could help the mesenchymal cell to morph into a certain mature cell type, the number of mesenchymal cells may decrease and the fluid production may decrease and could diminish the ganglion size as a result. The third possibility concerns hyaluronic acid, the main component of ganglion cyst fluid. In 2004, Kim et al. [9] published a report about hydrogel containing hyaluronic acid that shrank after electrical stimulation. The ganglion could also have shrunk as the hyaluronic acid decreased after it was directly affected by the electric current. Finally, the needle could have been directly inserted into the ganglion site and could have caused the fluid leakage and diminished the size.
We observed the decrease of ganglion size and pain after the electroacupuncture was performed on two patients. Thus, this is considered an interesting method of dealing with ganglions and hereby we provided our report with the related literatures.
Go to : 
References
1. Thornburg LE. Ganglions of the hand and wrist. J Am Acad Orthop Surg. 1999; 7:231–238. PMID: 10434077.

2. Gumus N. A new sclerotherapy technique for the wrist ganglion: transcutaneous electrocauterization. Ann Plast Surg. 2009; 63:42–44. PMID: 19546671.
3. Tekeoglu I, Dogan A. Electroacupuncture in the treatment of a ganglion of the wrist: a case report. Acupunct Med. 2006; 24:29–32. PMID: 16619407.
4. Andren L, Eiken O. Arthrographic studies of wrist ganglions. J Bone Joint Surg Am. 1971; 53:299–302. PMID: 5546702.

5. Gude W, Morelli V. Ganglion cysts of the wrist: pathophysiology, clinical picture, and management. Curr Rev Musculoskelet Med. 2008; 1:205–211. PMID: 19468907.

6. Loder RT, Robinson JH, Jackson WT, Allen DJ. A surface ultrastructure study of ganglia and digital mucous cysts. J Hand Surg Am. 1988; 13:758–762. PMID: 3241054.

7. Reed BV. Effect of high voltage pulsed electrical stimulation on microvascular permeability to plasma proteins: a possible mechanism in minimizing edema. Phys Ther. 1988; 68:491–495. PMID: 2451258.
8. Hwang SJ, Song YM, Cho TH, Kim RY, Lee TH, Kim SJ, et al. The implications of the response of human mesenchymal stromal cells in three-dimensional culture to electrical stimulation for tissue regeneration. Tissue Eng Part A. 2012; 18:432–445. PMID: 21913836.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download