Abstract
Hereditary neuropathy with liability to pressure palsies (HNPP) is an autosomal dominantly inherited disorder that affects peripheral nerves by repeated focal pressure. HNPP can be diagnosed by clinical findings, electrodiagnostic studies, histopathological features, and genetic analysis. Ultrasonography is increasingly used for the diagnosis of neuromuscular diseases; however, sonographic features of HNPP have not been clearly defined. We report the sonographic findings and comparative electrodiagnostic data in a 73-year-old woman with HNPP, confirmed by genetic analysis. The cross-sectional areas of peripheral nerves were enlarged at typical nerve entrapment sites, but enlargement at non-entrapment sites was uncommon. These sonographic features may be helpful for diagnosis of HNPP when electrodiagnostic studies are suspicious of HNPP and/or gene study is not compatible.
Hereditary neuropathy with liability to pressure palsies (HNPP) is an autosomal dominantly inherited disorder that affects peripheral nerves by repeated focal pressure. The incidence of HNPP is estimated at 16 per 100,000 in South-Western Finland. This may be an underestimation due to the insidious nature of the disease [1]. HNPP can be diagnosed by clinical findings, electrodiagnostic studies, histopathological features, and molecular genetics. It is clinically characterized by recurrent episodes of painless, acute-onset nerve paralysis, often precipitated by minor trauma or compression to nerve, especially of the median, ulnar and peroneal nerves. Electrodiagnostic studies have demonstrated slowing of distal motor and sensory nerve conduction velocities, predominantly at nerve entrapment sites. Histopathological changes include focal sausage-shaped thickening of the myelin sheath (tomacula) and segmental demyelination. The diagnosis is confirmed genetically by demonstrating a deletion in chromosome 17p11.2-12 containing the PMP22 gene or point mutation in the PMP22 gene [2].
High-resolution ultrasonography is increasingly used for the diagnosis of neuromuscular disorders. However, there are only few reports on sonographic features of the peripheral nerves in HNPP [1,3]. There are some differences in the sonographic findings of the nerves among these studies.
To our knowledge, there are no reports in the literature on the sonographic findings and comparative electrodiagnostic data of HNPP in Asian patients. We have experienced a typical HNPP case, and report on sonographic findings and comparative electrodiagnostic data of the peripheral nerves.
A 73-year-old, right-handed woman visited our hospital in September 2010, complaining of right foot drop and numbness on right lower leg in the previous month. There was no history of diabetes, trauma or any other polyneuropathy. She had undergone a lumbar disc operation five years previously. In particular her first son and grandson had a history of transient monoparesis of upper limbs that spontaneously resolved.
Neurological examination revealed weakness of right foot dorsiflexion and eversion (Medical Research Council scale grade 3) and reduced pinprick and touch sensations on the dorsal side of the right foot and the lateral aspect of the lower leg. Deep tendon reflexes at both knees and ankles were decreased.
Electrodiagnostic studies showed a right peroneal neuropathy around the knee level and chronic bilateral L5 radiculopathy. The sonographic examinations demonstrated swelling of right common peroneal nerve around the fibular head level (cross-sectional area [CSA], 18 mm2), compared with contralateral side (CSA, 9.6 mm2).
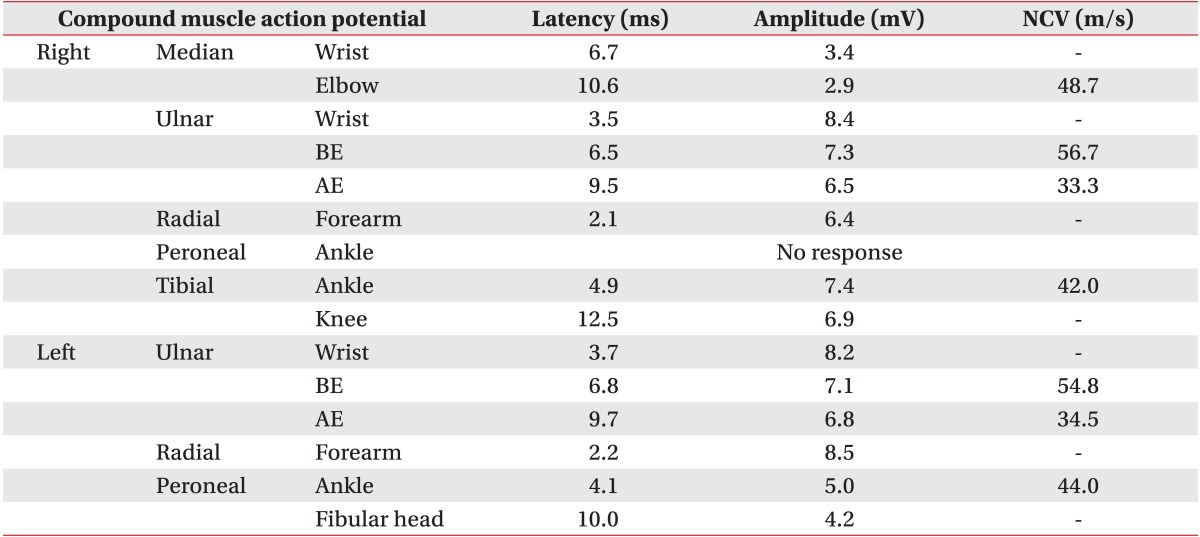
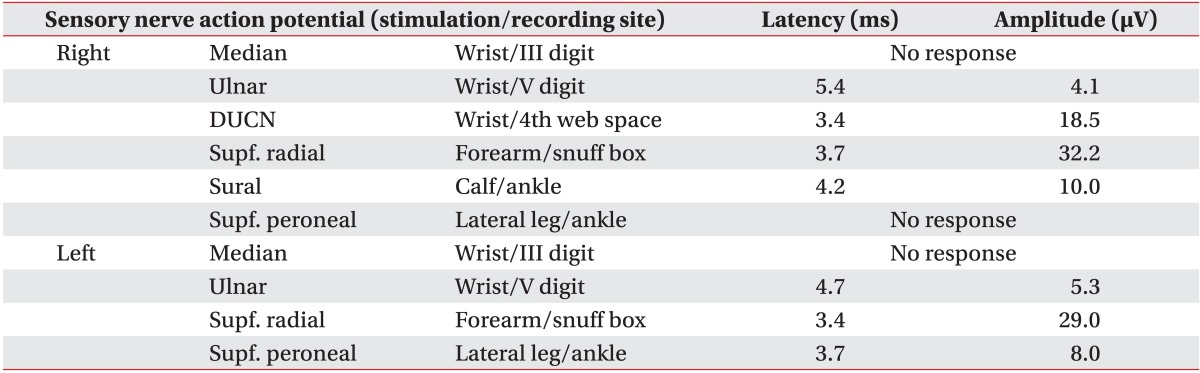
Six months later, while she was recovering from foot drop, she had another presentation with wrist drop on the right side. Electrodiagnostic studies were performed to rule out radial neuropathy. Motor nerve conduction studies showed prolonged distal latency and reduced compound muscle action potential amplitude in the right median nerve and no response in the right peroneal nerve. The ulnar nerve's segmental conduction velocities across the elbow were decreased (Table 1). In sensory nerve conduction studies, sensory nerve action potentials (SNAP) of both median nerves and right superficial peroneal nerve were not generated. The distal sensory latency was prolonged, and SNAP amplitude was reduced in both ulnar nerves (Table 2). In needle electromyography, ulnar innervated muscles including the abductor digiti minimi, first dorsal interosseous, and flexor carpi ulnaris showed large amplitude, long duration and polyphasic motor unit action potentials (MUAP) with reduced recruitment. In the forearm muscles innervated by radial nerve, extensor digitorum communis and extensor indicis proprius showed no MUAP. However brachioradialis and extensor carpi radialis longus muscles did not show any abnormalities. Median innervated muscles, such as abductor pollicis brevis and flexor carpi radialis, showed long duration and polyphasic MUAP. In lower limb muscles, abnormal spontaneous activities and large amplitude, long duration and polyphasic MUAP with reduced recruitment were demonstrated in right peroneal innervated muscles, such as tibialis anterior and peroneus longus (Table 3). These electrodiagnostic studies suggested not only right radial neuropathy, but also bilateral median, ulnar neuropath and right common peroneal neuropathy. The clinical findings and electrodiagnostic findings suggested HNPP, and the diagnosis was confirmed by genetic test demonstrating a PMP22 gene deletion.
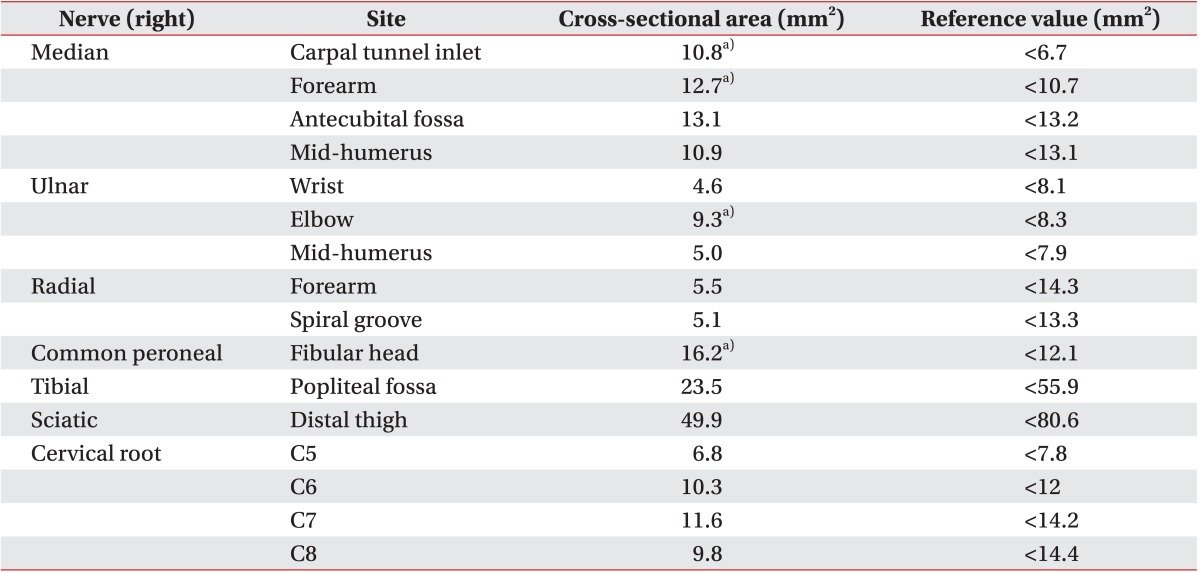
Peripheral nerves of the upper and lower extremities were examined by ultrasonography with an HD15 ultrasound system (Philips Ultrasound Inc., Bothell, WA, USA) using a 7-12 MHz linear array transducer. We traced most of the peripheral nerves, which were typically measured in previous studies about normal reference values of CSA in sonography, including median nerve at the level of carpal tunnel inlet and outlet in the forearm at the antecubital fossa and mid-humerus, ulnar nerve at the wrist and elbow, mid-humerus and radial nerve in the forearm and spiral groove level, common peroneal nerve at the fibular head level, tibial nerve at the popliteal fossa, sciatic nerve in the distal thigh and cervical roots at the C5-8 level. All measurements were done on the right side. CSA was measured using a direct tracing method just inside the hyperechoic rim of each nerve, and the CSA findings were compared with normal reference values [4-8].
The CSA of the median nerve at the carpal tunnel inlet and outlet (CSA, 10.8 mm2 and 9.8 mm2; normal value <6.7 mm2) and in the forearm (CSA, 12.7 mm2; normal value <10.7 mm2) was enlarged (Fig. 1). However the CSA of median nerve at the antecubital fossa (CSA, 13.1 mm2; normal value <13.2 mm2) and mid-humerus level (CSA, 10.9 mm2; normal value <13.1 mm2) was not swollen. The CSA of ulnar nerve was enlarged at the elbow (CSA, 9.3 mm2; normal value <8.3 mm2), but not in the wrist (CSA, 4.6 mm2; normal value <8.1 mm2), and not in the mid-humerus level (CSA, 5.0 mm2; normal value <7.9 mm2). The radial nerve was not swollen in the forearm (CSA, 5.5 mm2; normal value <14.3 mm2) or at the spiral groove level (CSA, 5.1 mm2; normal value <13.3 mm2). In the lower limb, the CSA of common peroneal nerve at the fibular head level was enlarged (CSA, 16.2 mm2; normal value <12.1 mm2) (Fig. 2). However, other nerves of lower extremity were not swollen: the tibial nerve at the popliteal fossa (CSA, 23.5 mm2; normal value <55.9 mm2) and the sciatic nerve in the distal thigh (CSA, 49.9 mm2; normal value <80.6 mm2). The cervical nerve roots (C5-8) were not enlarged at any root level: C5 root (CSA, 6.8 mm2; normal value <7.8 mm2), C6 root (CSA, 10.3 mm2; normal value <12 mm2), C7 root (CSA, 11.6 mm2; normal value <14.2 mm2) and C8 root (CSA, 9.8 mm2; normal value <14.4 mm2) (Table 4).
In this study, the nerve enlargements were seen at the entrapment sites which corresponded with the sites of neuropathy in electrodiagnostic studies, but enlargements at non-entrapment sites were only seen at the median nerve in the forearm level. There have been few previous reports on the sonographic features in HNPP. Beekman and Visser [3] first described sonographic features of HNPP in a case report. They demonstrated diffuse enlargement of several peripheral nerves at typical entrapment sites (ulnar nerve at the ulnar groove, Guyon canal, median nerve at the carpal tunnel) and outside these sites (ulnar nerve at the upper arm, median nerve at the forearm, tibial nerve at the medial malleolus). They hypothesized that diffuse nerve enlargement may be due to tomaculous (sausage-like) swelling of the myelin sheath, also that it may induce focal entrapment neuropathies at the typical entrapment site, such as carpal tunnel. In contrast, Hooper et al. [1] demonstrated enlarged nerves at the typical entrapment sites (median nerve at the wrist, ulnar nerve at the elbow), but enlargement at sites of non-entrapment (median and ulnar nerves in the forearm) was uncommon, except in tibial nerve at the ankle. They suggested that these multifocal nerve enlargements may be a clue to the diagnosis of HNPP. The sonographic findings of our study are consistent with the findings of Hooper et al. [1], but different from those of Beekman and Visser [3].
We obtained electrodiagnostic data that suggested median and ulnar neuropathy, right radial neuropathy, and right peroneal neuropathy. Correlation with sonographic findings, the sites of nerve enlargement were consistent with the sites of neuropathy in electrodiagnostic studies. Whereas radial nerve was not enlarged in spite of radial neuropathy, the reason for this discordance may be that we did not measure radial nerve at common entrapment site, such as arcade of Frohse, but measured at midforearm level. Other enlarged nerves were measured at entrapment site, such as carpal tunnel in median nerve, elbow level in ulnar nerve and fibular head level in common peroneal nerve, except forearm level in median nerve. These findings suggest that enlargement of nerve is occurred at the entrapment sites.
Hereditary neuropathies, such as Charcot-Marie-Tooth disease (CMT) and HNPP, were often confirmed by genetic analysis with distinguishing subtype. In HNPP patients, deletion of the PMP22 gene is detected in 85%-90% [2]. Thus, there is a possibility of false negative results from genetic analysis. Tekin and Ozgul [9] have reported on an HNPP patient with normal genetic analysis, diagnosed by clinical symptoms (left arm weakness and hypoesthesia), electrodiagnostic findings (bilateral median, ulnar, radial and fibular neuropathy) and ultrasonographic findings (focal thickenings of the median nerves at the wrists and ulnar nerves at the cubital tunnels). In ultrasonographic findings, diffuse nerve enlargement including at sites of non-entrapment were typical findings of the demyelinating neuropathies, such as CMT or chronic inflammatory demyelinating polyneuropathy (CIDP). In CMT and CIDP patients, the peripheral nerves are often enlarged throughout the course in the arm and forearm [10]. On the other hand, HNPP is characterized by more random nerve enlargement with multiple nerve entrapments (e.g., median neuropathy at the wrist and ulnar neuropathy at the elbow in combination) [1], and usually the nerve enlargements are seen at those entrapment sites. According to the study of Hooper et al. [1] and our case, the nerve enlargements at non-entrapment sites were uncommon, whereas Beekman and Visser [3] demonstrated diffuse nerve enlargement including at non-entrapment sites. Therefore, the presence of nerve enlargement at non-entrapment site in HNPP is debatable, and typical sonographic findings of HNPP are not clearly defined. If multiple focal nerve enlargement is identified on ultrasound, correlation with conduction block sites in the electrodiagnostic studies is helpful for the diagnosis of HNPP.
CSA of nerve may be correlated with age, gender, body mass index (BMI), height, and weight. Zaidman et al. [10] demonstrated that the nerve CSA has positive correlation with BMI, height, and weight. Typically Asian body types are slender and shorter than those of Western populations. Thus using the Western cutoff values of nerve CSA may have led to false negative results in our patient who was relatively thin and short (55 kg, 156 cm, BMI 22.6 kg/m2) with the upper normal limit being too high for her. In this study, we used Asian cutoff values of nerve CSA in median nerve at the carpal tunnel inlet, peroneal nerve at the fibular head and C5-8 roots [5,7,8]. However, other sites were analyzed with the Western cut-off values. Therefore there is a possibility of false negative results in those sites where the Western cutoff values were used. In addition we measured nerve CSA only on the right side, which was clinically affected. Comparison with the contralateral side and measuring of the side-to-side ratio of the CSA may be helpful to demonstrate ipsilateral nerve pathology.
In conclusion, sonographic detection of multifocal nerve enlargement is useful for the diagnosis of HNPP, especially when electrodiagnostic studies are limited and/or genetic analysis is not compatible. Further large scale studies of ultrasonography findings in HNPP correlated with clinical findings and electrodiagnostic studies are needed.
References
1. Hooper DR, Lawson W, Smith L, Baker SK. Sonographic features in hereditary neuropathy with liability to pressure palsies. Muscle Nerve. 2011; 44:862–867. PMID: 22102454.

2. Dubourg O, Mouton P, Brice A, LeGuern E, Bouche P. Guidelines for diagnosis of hereditary neuropathy with liability to pressure palsies. Neuromuscul Disord. 2000; 10:206–208. PMID: 10734269.

3. Beekman R, Visser LH. Sonographic detection of diffuse peripheral nerve enlargement in hereditary neuropathy with liability to pressure palsies. J Clin Ultrasound. 2002; 30:433–436. PMID: 12210462.

4. Cartwright MS, Passmore LV, Yoon JS, Brown ME, Caress JB, Walker FO. Cross-sectional area reference values for nerve ultrasonography. Muscle Nerve. 2008; 37:566–571. PMID: 18351581.

5. Park JY, Park SR, Lee SH, Choi KH. The ultrasonographic findings of the median nerve in the carpal tunnel according to age and sex of normal Korean adults. J Korean Acad Rehabil Med. 2008; 32:564–569.
6. Cartwright MS, Shin HW, Passmore LV, Walker FO. Ultrasonographic findings of the normal ulnar nerve in adults. Arch Phys Med Rehabil. 2007; 88:394–396. PMID: 17321837.

7. Won SJ, Kim BJ, Park KS, Kim SH, Yoon JS. Measurement of cross-sectional area of cervical roots and brachial plexus trunks. Muscle Nerve. 2012; 46:711–716. PMID: 23055312.

8. Park KC, Kwon DR, Kim MY, Lee HI, Ha DH, Hwang TS. Reference value for the cross sectional area of fibular nerve ultrasonography through the anatomic investigation in Korean. J Korean Acad Rehabil Med. 2011; 35:224–228.
9. Tekin L, Ozgul A. Ultrasound aids in the diagnosis of hereditary neuropathy with liability to pressure palsies. Surg Neurol. 2009; 71:399–400. PMID: 18440055.

10. Zaidman CM, Al-Lozi M, Pestronk A. Peripheral nerve size in normals and patients with polyneuropathy: an ultrasound study. Muscle Nerve. 2009; 40:960–966. PMID: 19697380.

Fig. 1
Transverse sonogram of right median nerve (dotted line) at the carpal tunnel inlet (A) and the forearm (B). The median nerve is hypoechoic and enlarged (cross-sectional area 10.8 mm2 and 12.7 mm2 at the carpal tunnel inlet and in the forearm, respectively).
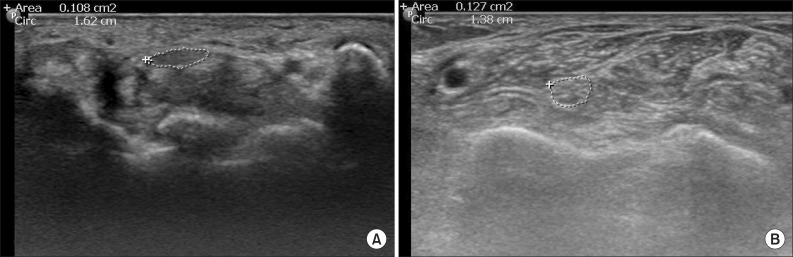
Fig. 2
Transverse sonogram of right common peroneal nerve (dotted line) at the fibular head (FH) level. The common peroneal nerve is swollen (cross-sectional area 16.2 mm2).
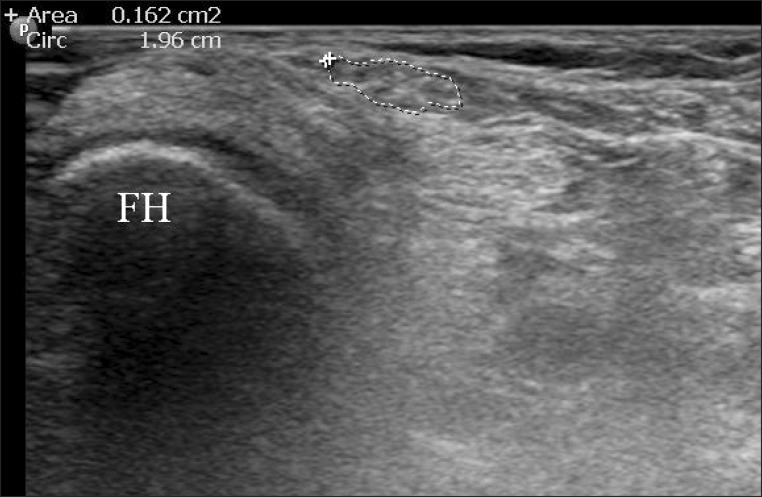
Table 3
Needle electromyography
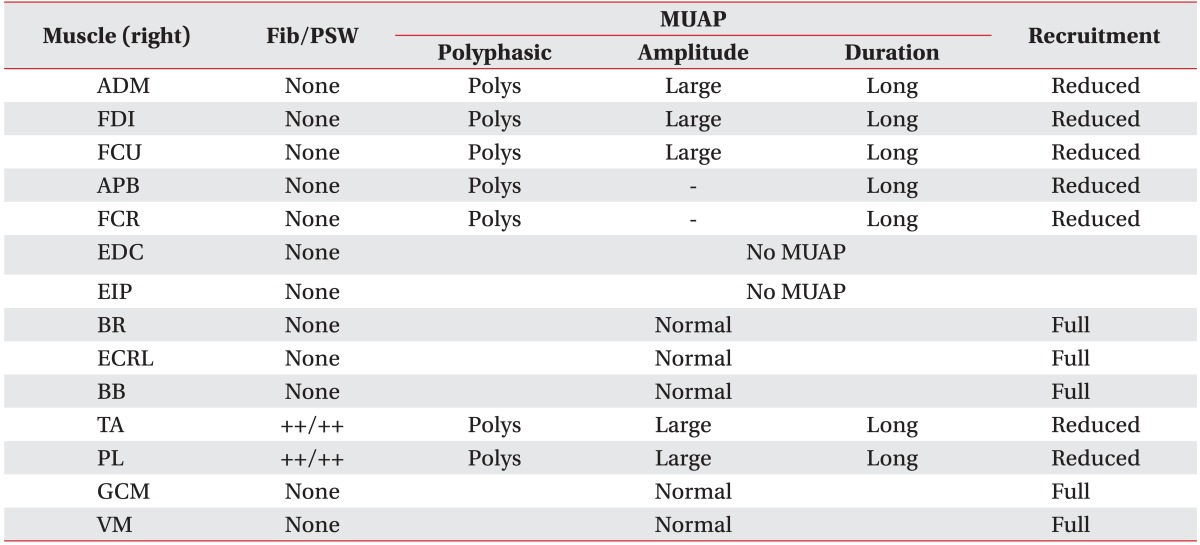
Fib/PSW, fibrillation potential/positive sharp wave; MUAP, motor unit action potentials; Polys, polyphasic; ADM, abductor digiti minimi; FDI, first dorsal interosseous; FCU, flexor carpi ulnaris; APB, abductor pollicis brevis; FCR, flexor carpi radialis; EDC, extensor digitorum communis; EIP, extensor indicis proprius; BR, brachioradialis; ECRL, extensor carpi radialis longus; BB, biceps brachii; TA, tibialis anterior; PL, peroneus longus; GCM, gastrocnemius medial head; VM, vastus medialis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download