Abstract
Recent years, various percutaneous procedures including cervical nucleoplasty have been developed for disc decompressions to relieve radicular pains caused by disc herniations. We report the application of percutaneous cervical nucleoplasty (PCN) by using the navigable disc decompression device in two patients of cervical herniated intervertebral discs (HIVD). A 38-year-old female diagnosed with C4-C5 disc extrusion with bilateral C5 roots impingement received nucleoplasty twice at C4-C5 disc level. After second procedure, her pain was improved from 6-7/10 to 1-2/10 by visual analog scale (VAS). The second case, a 51-year-male was diagnosed with C6-C7 disc extrusion with right C7 roots impingement and received the procedure at C6-C7 disc level. The pain improved from 8/10 to 3-4/10 by VAS. Successfully, we decompressed cervical herniated discs in 2 HIVD patients without major complications. The PCN with the navigable device will be recommended as an alternative treatment method for cervical HIVD.
Neck pain is the common problem that represents a spectrum of disorders affecting the cervical spine [1]. The clinical history and physical examination of patients with neck pain dictate the proper timing and selection of diagnostic studies, such as plain radiography, magnetic resonance imaging (MRI), and computed tomography (CT) myelography. Most neck pains are self-limiting and will resolve with appropriate conservative care. Nonsurgical treatment is the most appropriate first step in almost all cases of cervical radiculopathy.
Over the last 10 years, only one percutaneous intradiscal therapy, the Nucleoplasty (ArthroCare Co., Sunnyvale, CA, USA) [2], has been developed for cervical disc decompressions to relieve neck pains and radicular pains without the risks of open disc surgery. Nucleoplasty has been shown to remove disc tissues and reduce intradiscal pressure [2,3], but it cannot remove herniated disc materials directly. Recently, we developed the navigable disc decompression device, the L'DISQ (U&I Co., Uijeongbu, Korea), which is a minimally-invasive device for percutaneous disc decompressions [4]. It uses bipolar radiofrequency technology which is applied to a conductive medium (e.g., saline) as to achieve tissues removal with minimal thermal damages to collateral tissues. This is an advanced procedure which is compared with previous intradiscal procedures on the respect of safety with neural tissue stimulation and efficacy of removing herniated materials.
The purpose of this study is a clinical application of percutaneous disc decompressions using the navigable disc decompression device (L'DISQ) for patients with cervical herniated intervertebral disc (HIVD).
A 38-year-old female came to complain of neck pain with radiating to the bilateral upper extremities after a traffic accident at April 26, 2009. The rate of her pain was at 7-8/10 by visual analog scale (VAS) and the pain was aggravated by bending backward and relieved only slightly by resting.
A physical examination revealed a positive Spurling sign in the bilateral upper extremities. She had no sensory deficits but mild motor weaknesses in the right upper extremity. Deep tendon reflexes are normal and symmetrical. MRI images (Fig. 1) demonstrated central disc extrusion at C4-C5, making contact with bilateral C5 nerve roots. The patient was diagnosed with a C4-C5 disc extrusion with bilateral C5 roots impingement. Percutaneous cervical nucleoplasty (PCN) with the navigable disc decompression device (L'DISQ) was performed at C4-C5 disc level with CT and fluoroscopic guidance on June 3, 2009. The procedure was performed using a standard midline approach (Fig. 2) [5]. Procedure time required 3 hours. Her pain was reduced to 5/10 by VAS the first postoperative day. After leaving the hospital, she visited hospital again on June 9, 2009 and did not appeal any pains at that time. However, she admitted again due to aggravation of neck pains radiating to the right upper extremities from January 2010. The rate of her pain was at 6-7/10 by VAS. A physical examination revealed a positive Spurling sign in the right upper extremity. She has no motor deficits but only mild paresthesia on right C4 and C5 dermatomes. The patient was diagnosed with a C4-C5 disc extrusion with right C5 roots impingement. PCN using the L'DISQ was performed again at the same level on March 25, 2010 with fluoroscopic guidance (Fig. 3). Tip of the L-DISQ catheter reached the end of the bulging disc, and disc decompression was done successfully. Her pain was reduced to 5/10 and negative Spurling sign was observed the first postoperative day. After the procedure, posterior neck area axial pain was improved to 4/10 at 2 months and 2/10 by VAS at 6 months later without the pains radiating to the right upper extremity.
A 51-year-male visited the hospital because of neck and low back pains since February 2009 after a traffic accident. The patient was admitted to other hospitals and received physical therapy and selective nerve block. However, it was not effective enough to relieve the pain. The rate of his pain was at 8/10 by VAS. A physical examination revealed a positive Spurling sign with pain radiating to right upper extremity. He had no motor deficits but mild hypoesthesia on the right upper extremity with non-dermatomal distribution patterns. Deep tendon reflexes are normal and symmetrical. MRI images findings showed disc extrusion at C6-C7, making contact with right C7 nerve root (Fig. 4). The patient was diagnosed with a C6-C7 disc extrusion with right C7 roots impingement. The PCN used the L-DISQ and was performed at C6-C7 disc level with fluoroscopic guidance on June 16, 2009 for 90 minutes (Fig. 5). The procedure performed used a standard midline approach. He did not appeal any immediate pains after finishing the procedure, but within an hour he had to consume pain killers due to procedure site pains. The following day, the pain radiated to the right upper extremity was improved to 2-3/10 and posterior neck area axial pain was reduced to 3-4/10 by VAS. He was discharged the next day of the procedure and visited hospital again on July 29, 2009. Postoperative evaluation showed that axial neck area pain remained 3-4/10 by VAS and the pain radiating to the right upper extremity had disappeared.
In this study, two patients who had received PCN using the navigable disc decompression device (L'DISQ) showed significant pain reliefs. One patient showed recurrence of right C5 radiculopathy, but symptom was decreased by reapplying the procedure on the C4-C5 intervertebral disc.
Disc decompression has been shown to treat symptomatic patients with contained herniated discs at the cervical and lumbar spines. A variety of techniques have been used to decompress discs, including chemical, mechanical, and thermal/heat (radiofrequency and laser) methods at the cervical and lumbar spines [6-8]. Among the methods, decompression with nucleoplasty is a minimally invasive treatment for HIVD that uses radiofrequency energy for partial decompression of the nucleus pulposus [3]. However, nucleoplasty cannot remove the herniated disc materials directly and merely decompresses the central pressure. In case of excessive removals of the tissues, it will cause losses of disc heights and possibly lead to disc degenerations [9]. Moreover, thermal injury to the disc is possible. Introduction of large instruments into the nucleus of the disc can cause irreparable damages to the annulus.
L'DISQ is a newly development minimally invasive device for percutaneous disc decompressions by using bipolar radiofrequency technology [4]. The tip of L'DISQ wand is designed to access the posterolateral or posterocentral disc, and decompresses the herniated nuclear material. Unlike the nucleoplasty which uses rigid and uncontrolled tip, the L'DISQ adopts navigable tip which can be curved to the desired angles by the rotation of the control wheel. Therefore, L'DISQ can directly access and eliminate the herniated tissues, even in cases of extruded discs. The temperature did not exceed 13℃ above the initial temperature at distances of 1 mm from the advanced wand tip during ablation, thus, indicating that denaturation of adjacent neural tissues did not occur. Also, histopathologic examinations demonstrated decompressions of the nucleus pulposus without thermal damages to the surrounding neural tissues [10]. In fact, about 90% of normal tissues were preserved after this procedure.
The distance of two electrodes on L'DISQ tip is 0.8 mm. If the nerve root is placed more than 0.8 mm from the tip, it would be safe from the electric shocks or damages, and the thin outer annulus is a poor conductor of electrical currents [4]. The electric currents should pass the other electrode rather than the nerve root. Previous to the disc decompression adjacent the nerve roots, we have always used the electric stimulations to prevent neural tissue damages. Post-procedural infections, bleeding, and other complications were also not found in this study.
The limitation of this study is that it is a pilot study which needed long-term follow-up reports for outcomes. However, both people showed dramatic improvements of pain after the procedure, and we can expect that the PCN using the navigable disc decompression device (L'DISQ) could be recommended as a new treatment method for cervical HIVD.
References
1. Smith MD. Cervical radiculopathy: causes and surgical treatment. Minn Med. 1995; 78:28–30. 42–45. PMID: 7760784.
2. Chen YC, Lee SH, Saenz Y, Lehman NL. Histologic findings of disc, end plate and neural elements after coblation of nucleus pulposus: an experimental nucleoplasty study. Spine J. 2003; 3:466–470. PMID: 14609691.

3. Li J, Yan DI, Zhang ZH. Percutaneous cervical nucleoplasty in the treatment of cervical disc herniation. Eur Spine J. 2008; 17:1664–1669. PMID: 18830638.

4. Lee SH, Derby R, Sul DG, Hong JW, Kim GH, Kang S, et al. Efficacy of a new navigable percutaneous disc decompression device (L'DISQ) in patients with herniated nucleus pulposus related to radicular pain. Pain Med. 2011; 12:370–376. PMID: 21332936.

5. Slipman CW, Derby R, Simeone FA, Mayer TG. Interventional spine: an algorithmic approach. Philadelphia: Elsevier;2008.
6. Kambin P, Schaffer JL. Percutaneous lumbar discectomy: review of 100 patients and current practice. Clin Orthop Relat Res. 1989; 238:24–34. PMID: 2910608.
7. Karasek M, Bogduk N. Twelve-month follow-up of a controlled trial of intradiscal thermal anuloplasty for back pain due to internal disc disruption. Spine (Phila Pa 1976). 2000; 25:2601–2607. PMID: 11034644.

8. Nerubay J, Caspi I, Levinkopf M, Tadmor A, Bubis JJ. Percutaneous laser nucleolysis of the intervertebral lumbar disc: an experimental study. Clin Orthop Relat Res. 1997; 337:42–44. PMID: 9137174.

9. Castro WH, Halm H, Rondhuis J. The influence of automated percutaneous lumbar discectomy (APLD) on the biomechanics of the lumbar intervertebral disc: an experimental study. Acta Orthop Belg. 1992; 58:400–405. PMID: 1485502.
10. Yoo SH. An assessment of a new navigable percutaneous disc decompression device (L'DISQ) through histologic evaluation and thermo-mapping in human cervical cadaveric discs [dissertation]. Seoul: Korea University;2012.
Fig. 1
Cervical magnetic resonance imaging shows central disc extrusion at C4-C5. (A) Sagittal view, (B) axial view.

Fig. 2
(A), (B) show placement of the L-DISQ catheter tip into the herniated disc with computed tomography guidance of the standard midline approach.
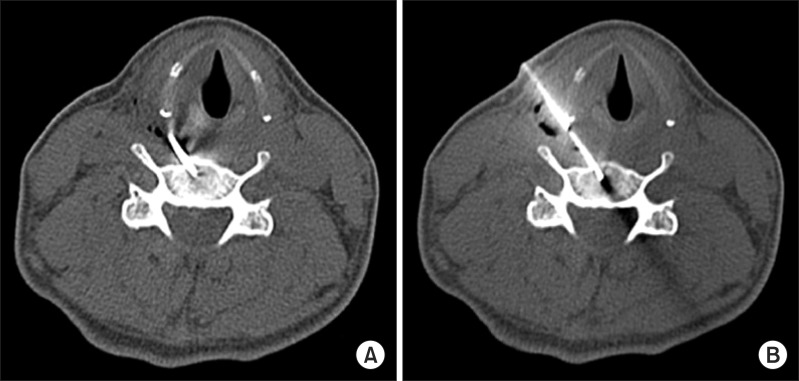
Fig. 3
Placing the tip of the L-DISQ catheter into the herniated disc. (A) Lateral view, (B) anterior-posterior view.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download