This article has been
cited by other articles in ScienceCentral.
Abstract
The postoperative infectious spondylitis has been reported to occur among every 1% to 12%. It is difficult to early diagnose in some cases. If the diagnosis is delayed, it can be a life-threatening condition. We report a 32-year-old male patient with postoperative infectious spondylitis. He had surgical treatments for traumatic intervertebral disc herniations in L3-4 and L4-5. Three weeks after surgery, he complained for fever and paraplegia. Cervicothoracic magnetic resonance imaging showed the collapsed T2 and T3 vertebral body with changes of bone marrow signal intensity. Moreover, it showed anterior and posterior epidural masses causing spinal cord compressions which suggested infectious spondylitis. After the use of antibiotics and surgical decompressions T2-T3, his general conditions were improved and muscle power of lower extremities began to be gradually restored. However, we could not identify the exact organisms that may be the cause of infectious spondylitis. It could be important that the infectious spondylitis, which is presented away from the primary operative level, should be observed in patients with fevers of unknown origin and paraplegia.
Go to :

Keywords: Spondylitis, Intervertebral disc displacement, Spinal cord compression
INTRODUCTION
Infectious spondylitis is a severe disease which includes spondylodiscitis, septic discitis, myelitis, and epidural abscess, among others. The reported incidence rate of this rare pyogenic infectious spondylitis is 0.2-2 cases in one million persons per year. Recently, an increase has been found due to the suspected elongated life expectancy of patient with chronic diseases [
1]. Moreover, the incidence rate of postoperative infectious spondylitis has been increasing. Higher incidence is due to increases of using spinal surgical instruments in operations and antimicrobial-resistant pathogens [
2].
Most postoperative infectious spondylitis occurs at the operated level or its adjacent vertebrae while few cases occur at distant from operated site. According to a previous case report, the pyogenic spondylitis occurred at the non-operated level was approximately seven years postoperatively. At the sites of infection, Harrington hooks and screws were inserted [
3]. We recently experienced a case of infectious spondylitis that occurred distantly from the operated vertebrae. In this present case, we reported a patient who had an infectious spondylitis of thoracic vertebrae three weeks after surgical treatments of herniated lumbar intervertebral disc.
Go to :

CASE REPORT
A 32-year-old Mongolian male developed lower back pains after a traffic accident and was diagnosed to have traumatic L3-4 and L4-5 herniation of intervertebral disc via magnetic resonance imaging (MRI) at a Mongolian orthopedic clinic. The patient had no past medical history of high blood pressure, diabetes, tuberculosis or hepatitis, and he was not a smoker. After a week, he had an operation on total laminectomy and discectomy at L3-4, L4-5 levels and posterior interbody fusions at L3-5 (
Fig. 1). The patient had a fever 3 weeks after the surgery, and also developed bilateral lower extremities and external anal sphincter muscle weakness.
 | Fig. 1Lumbosacral spine X-ray shows a surgical intervention of posterior instrumentation from L3 to L5 vertebrae: (A) lateral image, (B) anteroposterior image. 
|
To investigate the causes of fever and neurological deficits, a lumbosacral MRI follow-up was performed but no definite abnormalities were found. Seven weeks after surgery, the patient was transferred to the department of neurosurgery at our medical institution for further evaluations and treatments. When performed a whole spine MRI, the T2 and T3 vertebral body destruction and compressive myelopathy were detected (
Figs. 2,
3). Anterior and posterior epidural mass formations caused the compressive myelopathy at T2 to T4 levels. In addition, the epidural mass was extended to bilateral T3-T4 neural foramen, thus, forming the paravertebral mass.
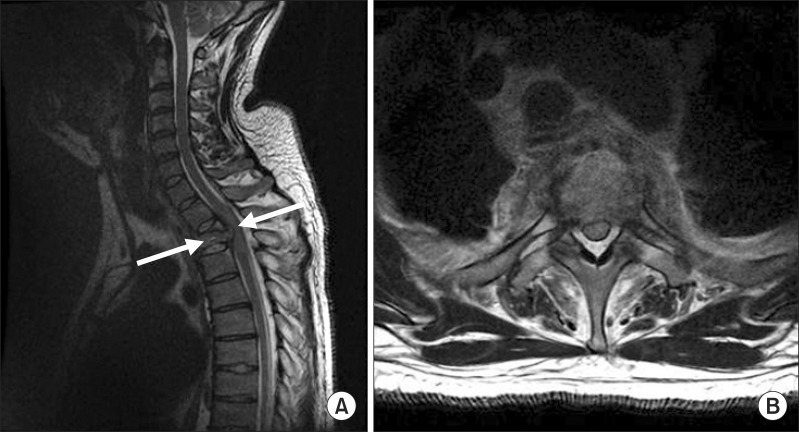 | Fig. 2(A) Sagittal T2-weighted magnetic resonance image of the cervicothoracic spine showing collapsed T2 and T3 vertebrae (arrow), anterior and posterior epidural mass formation, causing compressive myelopathy at T2 to T4 level. (B) Axial T2-weighted magnetic resonance image between T2 and T3 level. 
|
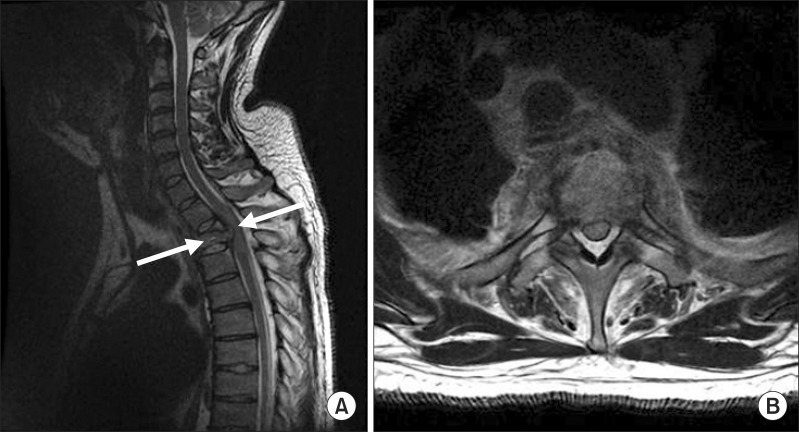
 | Fig. 3(A) Sagittal contrast-enhanced T1-weighted magnetic resonance image of the cervicothoracic spine showing collapsed T2 and T3 vertebrae (arrow) and enhanced anterior and posterior epidural mass formation, causing compressive myelopathy at T2 to T4 level. (B) Axial contrast-enhanced T1-weighted magnetic resonance image between T2 and T3 level. 
|
Based on the laboratory studies, white blood cell (WBC) count resulted to 7,020/µL, the erythrocyte sedimentation rate (ESR) is at 54 mm/hr, and the C-reactive protein (CRP) level reached 0.87 mg/dL. The reported values represented increases from the normal ranges.
Upon physical examinations, voluntary anal contracture was not checked. Therefore, a manual muscle testing in accordance to the Medical Research Council (MRC) scale was performed to the bilateral hip flexors and knee extensor which resulted in the MRC grade II. Bilateral ankle dorsiflexors, big toe extensors, and plantar flexors were checked as MRC grade I. Sensory deficit was noted below bilateral T9 dermatome. In addition, there were also no perianal and deep anal sensations. Both the left knee and ankle jerks were brisk. Babinski sign was bilaterally checked while the ankle clonus was not.
Open bone biopsy of thoracic vertebrae, blood culture, and antigen detection assays were performed to determine microorganisms. The specimens were sent for bacterial culture, acid-fast bacilli smear and culture, fungal culture and polymerase chain reaction for Mycobacterium tuberculosis. The results of the tests were all negative. Microscopic histological examinations of thoracic vertebrae biopsy revealed chronic spondylitis. T2 and T3 vertebrae showed hypercellular bone marrow tissues with bone desorptions and high cellularity with focal infiltrations of chronic inflammatory cells including plasma cells in normal marrow. An open biopsy of the soft tissues at the lumbar operative site was also performed which showed foreign body reactions with granulation tissues and fat necrosis.
For the treatment of compressive myelopathy, the patient had a decompression laminectomy at T2-T3 level. The patient was also treated by antibiotics. Nafcillin was applied for 11 days followed by cefadroxil for 5 weeks. The patient was then transferred to a rehabilitation medicine department when his neurological and medical conditions were stabilized.
The laboratory tests showed improvements after surgery and antibiotics treatments. Results were 5,900/µL, 14 mm/hr, and 0.38mg/dL, for the WBC count, ESR, and CRP level, respectively.
After decompressions of laminectomy and antibiotics treatment, the weaknesses of bilateral lower extremities were improved. Bilateral hip flexor, bilateral knee extensors, and right ankle dorsiflexor were checked for MRC grade IV. Left ankle dorsiflexor, bilateral big toe extensors, and bilateral ankle plantar flexors were checked as grade III. Moreover, the voluntary anal contraction was mildly checked, and the perianal skin sense and deep anal sense were recovered. After positive examinations, the patient was discharged from the hospital with no additional complications.
Go to :

DISCUSSION
In recent years, as the spinal surgery has been frequently performed and its technique has diversified, the incidence of spinal infections due to surgery has increased [
4]. It varies depending on the types of spinal surgery. Nevertheless, the rate of infection has been reported to be approximately 0.7%-2.8% following palliative laminectomy and discectomy in cases for herniation of the intervertebral disc, 0.9%-6.0% following posterior fusion concomitantly with vertebral laminectomy, and 1.3%-12.0% following vertebral instrumentation concomitantly with posterior interbody fusion [
2]. Not only because the dura mater is directly exposed when the affected site is opened for surgical operation, but also because it is difficult to remove the surgical instruments postoperatively due to the vertebral instability. Thus, more special attention should be paid to the possible occurrences of posterior infections as compared with other body areas [
1]. Particularly in patients who developed neurological deficits due to the formation of epidural abscess, a poor prognosis is expected. Therefore, a conscientious monitoring for possible infections is essential for these patients [
4].
In the present case, the infections occurred in the thoracic vertebral regions which are distant from the sites of operation. The operators suspected the fever and lower limb weakness originating from infections when operating for lumbar disc herniation. They performed a lumbosacral MRI, but failed to identify the causative factors. As described, infections found at non-operated sites are rarely being reported. According to a previous study, through an analysis on the location of discitis occurring following operations of lumbar disc herniation, the infections occurred in 13 out of 111 patients at non-operated sites [
5]. All of these 13 patients had infections localized to the lumbar region, and there were no cases of infections occurring in the thoracic or cervical regions. Furthermore, there were also no cases of epidural abscess and myelopathy. These features are different from the present case.
The postoperative infectious spondylitis has been reported to arise from the direct contaminate at the operated site and the hematogenous spread [
6]. It has also been reported that the infections occurring at the non-operated sites are associated with hematogenous seeding. Also in the present case, the infections might have spread to the thoracic spine from the operated site via a hematogenous route. In cases of pyogenic spondylitis which occurred postoperatively, the
Staphylococcus aureus accounts for 60% of total causative bacteria that have been identified [
5]. However, it is known that the causative bacterial strains are unidentifiable in approximately one-third of total cases on infectious spondylitis [
7]. In the present case, according to the blood culture and several tests of the thoracic region specimens, there were no specific types of infectious microorganisms. However, there was fever and increased serum levels of inflammatory markers. In addition, we observed epidural abscess on the MRI scan and spondylitis on histopathologic finding. These findings led to a clinical diagnosis, followed by the institution of antibiotic treatments. Therefore, the fever and increased serum levels of inflammatory markers were also being improved.
For all patients who underwent spinal surgery, clinicians should be aware of the possibility that non-operated spinal levels are also subjected to infections. In addition, it is also necessary to closely monitor the possible increasing serum levels of inflammatory markers as well as postoperative fevers and pains. Thus, attempts should be made to detect the postoperative infections at the earliest possible stage.
Typical findings appeared on plain radiography at 2-4 weeks following the onset of the disease. Thus, a plain radiography cannot be used as the primary imaging study [
6]. It has been reported that an MRI has a sensitivity of 96%, a specificity of 92%, and an accuracy of 94% for patients with pyogenic spondylitis [
8]. For such reasons, an MRI should be performed for patients who are suspected of having spondylitis. Additionally, an MRI is an imaging modality that has higher levels of resolution for soft tissues. It is advantageous for confirming whether the infections were spread by visualizing the bone marrow, the paravertebral soft tissues, spinal canals, and spinal nervous structures including the spinal cord [
5]. As shown in the present case, the patient had infections at the thoracic level which was distant from the operated site although no infections occurred at the operated, lumbar one. Based on this case, clinicians should be aware of the possibility that infectious spondylitis might be present in patients who had the fever postoperatively and increased serum levels of inflammatory markers. In addition, clinicians should evaluate all the non-operated, non-adjacent spines as well as the operated site on MRI scans, for which they should perform an overall evaluation of the spine or obtain scout film.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download