Abstract
Objective
To evaluate the usefulness of plain abdominal radiography as an evaluation method for bowel dysfunction in patients with spinal cord injury (SCI).
Methods
Forty-four patients with SCI were recruited. Patients were interviewed about their clinical symptoms, and the constipation score and Bristol stool form scale were assessed. The colon transit time (CTT) was measured by using radio-opaque markers (Kolomark). The degree of stool retention and the presence of megacolon or megarectum were evaluated using plain abdominal radiographs. We examined the relationship between clinical aspects and CTT and plain abdominal radiography.
Results
The constipation scores ranged from 1 to 13, and the average was 4.19±3.11, and the Bristol stool form scale ranged from 1 to 6, with an average of 4.13±1.45. CTTs were 19.3±16.17, 19.3±13.45, 15.32±13.15, and 52.42±19.14 in the right, left, rectosigmoid, and total colon. Starreveld scores were 3.4±0.7, 1.8±0.86, 2.83±0.82, 2.14±1, and 10.19±2.45 in the ascending, transverse, descending, rectosigmoid, and total colon. Leech scores were 3.28±0.7, 2.8±0.8, 2.35±0.85, and 8.45±1.83 in the right, left, rectosigmoid, and total colon. The number of patients with megacolon and megarectum was 14 (31.8%) and 11 (25%). There were statistically significant correlations between the total CTT and constipation score (p<0.05), and Starreveld and Leech scores (p<0.05). Significant correlations were observed between each segmental CTT and the segmental stool retention score (p<0.05).
Bowel dysfunction due to a neurogenic bowel after spinal cord injury (SCI) usually manifests as constipation, fecal incontinence and fecal impaction, which is one of the most common complications reported in 39% of the patients with SCI [1]. However, the importance of gastrointestinal problems has been relatively ignored compared to its incidence rate and severity. This is because complications due to a neurogenic bowel are chronic and difficult to control, and are less severe and fatal than complications of a neurogenic bladder [2].
While the evaluation of neurogenic bowel in patients with SCI depends on subjective symptoms such as bowel frequency, considering previous reports that show the memories of patients concerning their bowel habit are sometimes inaccurate [3], objective evaluation methods such as plain abdominal radiography and colon transit time are recommended [4]. Since plain abdominal radiography has advantages such as being simple to perform and is less expensive and involves less radiation than other types of radiological investigations, it is a useful method to evaluate the degree and distribution of feces in the colon and to show the presence of megacolon, and it can also help in evaluating proper bowel management, the degree and location of fecal impaction and the establishment of a proper treatment plan [5]. In previous studies, Leech et al. [6] reported that plain abdominal radiography showed high reproducibility and high inter-inspector consistency in evaluating stool retention among children with constipation. Starreveld et al. [4] reported that plain abdominal radiography was significantly correlated with characteristics of the bowel pattern such as bowel frequency, and hardness and weight of the feces. However, studies on the scoring system using plain abdominal radiography have focused on children or adult patients with functional constipation, and correlations with subjective symptoms such as the bowel pattern or frequency were observed, and thus these studies had the limitation of having no comparisons with the colon transit time, which is known as an objective evaluation method. In addition, the pattern of bowel dysfunction in patients with SCI may be different from the pattern of bowel dysfunction in functional constipation, and there has been no study of patients with SCI which examines whether or not plain abdominal radiography evaluates the degree of stool retention quantitatively and whether the results are helpful in guiding proper management.
Therefore, this study is aimed to evaluate the relationship between the degree of total and segmental stool retention, bowel pattern and colon transit time using plain abdominal radiographs, with the purpose of determining the usefulness of plain abdominal radiographs and examining the convenience of their use clinically including their use in proper bowel management, with methods of management chosen according to the location and degree of stool retention.
Patients with SCI who were admitted to the rehabilitation medicine department from December, 2004 to November, 2011 at least 2 months after injury completed a questionnaire on their bowel pattern, and their constipation score and morphological stool characteristics were recorded. Their stool retention score and the presence of megacolon and megarectum were evaluated. A total of 44 subjects who were also evaluated for their colon transit time were included in this study. Among the candidate patients, those who had a history of organic gastrointestinal disease or a history of gastrointestinal surgery except for simple appendectomy or cholecystectomy were excluded. The subjects were asked to maintain a regular diet and ordinary life style during the evaluation. There was no change made to the medications they used.
With respect to the bowel pattern, the constipation score was evaluated using the Rome II Diagnostic Criteria [7] and the morphological stool characteristics were recorded. For Rome II Diagnostic Criteria, the bowel frequency for 7 days, and the presence of straining, lumpy or hard stools, sensation of incomplete evacuation, and sensation of anorectal obstruction and the need for additional manual maneuvers to facilitate defecation during the last 2 months were recorded. In detail, for bowel frequency, 0 point was assigned to '3 or more bowel movements per week', 1 point to '1-2 per week', 2 points to '1 for 10 days', 3 points to 'hard to move the bowel for more than 10 days'. For the items of 'straining', 'lumpy or hard stools', 'sensation of incomplete evacuation', 'sensation of anorectal obstruction' and 'need for additional manual maneuvers to facilitate defecation', 0 point was assigned to 'none', 1 point to 'at least 1 among 4 times', 2 points to '2-3 times among 4 times', 3 points to 'always'. The range of the constipation score was 0-18, and a higher score meant more severe constipation was present.
To examine the morphological stool characteristics, the form of the stool after a bowel movement was checked on the Bristol stool form scale which classifies the form into 7 types, from type 1 to type 7 [8].
For the measurement of the colon transit time to evaluate colonic motility, the subjects were asked to take 1 capsule of Kolomark (MI Tech, Seoul, Korea) containing 20 marker rings with radio-opacity for 3 days at 9:00 AM. At 9:00 AM on the 4th day, a plain abdominal radiograph was taken.
To measure the segmental colon transit time in the plain abdominal radiographs, the total colon was divided into the right colon, left colon and rectosigmoid colon and the total and the segmental transit times were calculated.
For the plain abdominal radiography, the plain abdominal radiograph administered on the 4th day was used for evaluation of the colon transit time. Two skilled radiologists analyzed the provided plain abdominal radiographs using the Starreveld score and Leech score to examine the degree of stool retention and additionally the presence of megacolon and megarectum. The Starreveld score was divided into the ascending colon, transverse colon, descending colon, and rectosigmoid colon. The Leech score was divided into the right, left, and rectosigmoid colon. If stool was observed only in the rectum, 1 point (never) was assigned. If stool was observed in the rectum and non-continuously observed in the colon, 2 points (mild) were assigned. If stool was observed in the rectum and continuously observed in the total colon, 3 points (moderate) were assigned. If stool was continuously observed in any place in the total colon and the rectosigmoid colon was filled with stool, 4 points (severe) were assigned. Using such a scoring system, the Starreveld score was recorded as 4-16 points, whereas the Leech score was recorded as 4-12 points.
As for megacolon and megarectum, the criteria proposed by Margulis and Burhenne [10], in which megacolon was defined as having a maximum colon diameter of over 6 cm and megarectum as having a maximum rectum diameter of over 4 cm, was used.
Statistical analysis used SPSS ver. 19.4 (IBM SPSS, Armonk, NY, USA). Pearson correlation coefficients were used to analyze correlations in the bowel patterns such as the constipation score and the Bristol stool form scale, and the degree of stool retention on plain abdominal radiography and colon transit time, as well as inter-inspector reliability. The mean difference in colon transit time between the two groups, depending on the presence/absence of megacolon and megarecturm, was analyzed using the independent t-test, using a significance level of p<0.05.
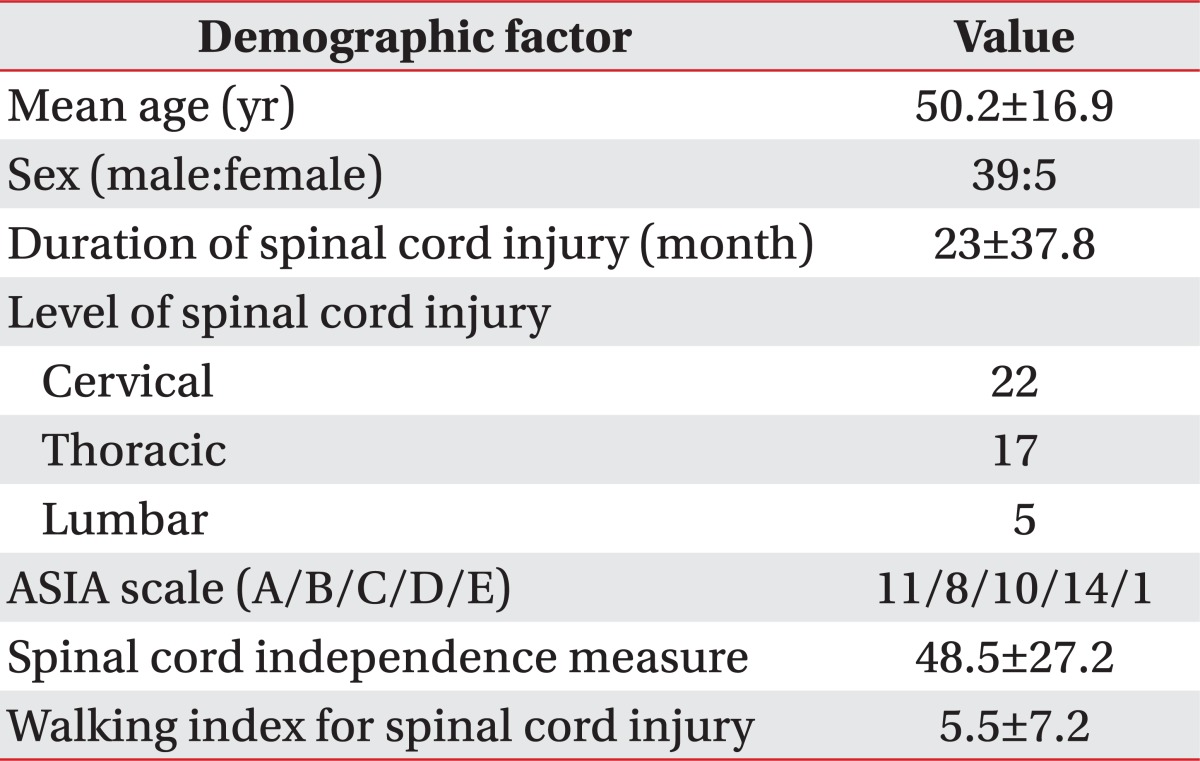
The study subjects totalled 44 patients (39 males and 5 females). Their age ranged from 22 to 76 years with an average age of 50.2±16.9. The period from injury to evaluation was 23±37.8 months on average. As for the degree of SCI, there were 11 patients with complete SCI and 33 with incomplete SCI. The injury levels included 22 cervical level, 17 thoracic level and 5 lumbar level. According to the scale of the American Spinal Cord Injury Association, 11 fell into A, 8 into B, C into 10, 14 into D, and 1 into E. The average Spinal Cord Independence Measure (SCIM) was 48.5±27.2; the average Walking Index for Spinal Cord Injury II was 5.5±7.2 (Table 1).
When the Rome II Diagnostic Criteria was applied, 39 patients were positive for constipation. Their constipation score ranged 1 to 13 with an average score of 4.19±3.11. The Bristol stool form scale score ranged from 1 to 6 with an average score of 4.13±1.45.
Colon transit time was 19.3±16.17 for the right colon, 19.3±13.45 for the left colon, and 15.32±13.15 for the rectosigmoid colon. The total colon transit time was 52.42±19.14, which was long compared to the colon transit
time of normal persons.
The Starreveld score measured with the plain abdominal radiograph was 3.4±0.7 at the ascending colon; 1.8±0.86 at the transverse colon, 2.83±0.82 at the descending colon, and 2.14±1.0 at the rectosigmoid colon. It was measured as 10.19±2.45 at the total colon. The Leech score was 3.28±0.7 at the right colon, 2.8±0.8 at the left colon, and 2.35 ± 0.85 at the rectosigmoid colon. It was measured as 8.45±1.83 at the total colon (Fig. 1).
Megacolon was observed in 14 patients (31.8%). All of the incidences of megacolon were observed at the ascending colon. Megarectum was observed in 11 patients (25%). Both megacolon and megarectum were observed in 5 patients (11.4%).
To evaluate inspector variations in reading plain abdominal radiographs, the consistency of the degree of stool retention and presence/absence of megacolon or megarectum were compared. The results showed that the inter-inspector consistency in reading was significantly high (p<0.01) (Fig. 2).
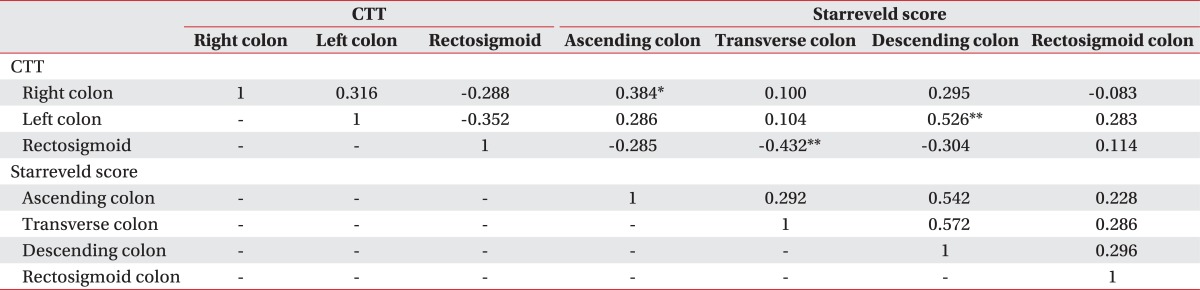
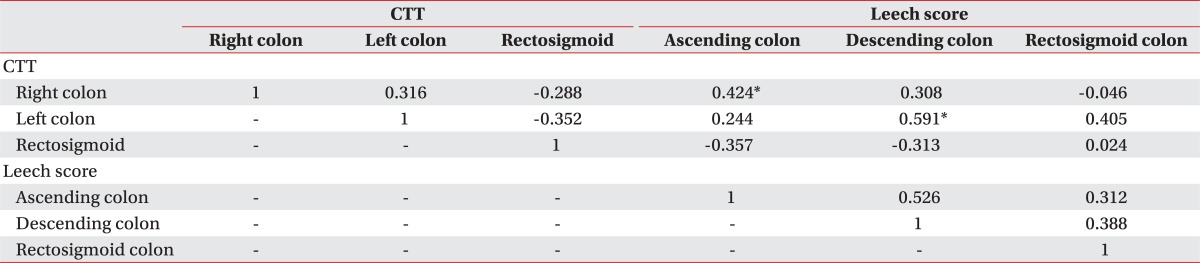
In the correlation between segmental colon transit time and the Starreveld score, as the right colon transit time increased, the stool retention score at the ascending colon increased, and as the left colon transit time increased, the stool retention score at the descending colon increased (p<0.05), and a negative correlation was observed in that as the rectosigmoid colon transit time increased, the stool retention score at the transverse colon decreased (p<0.01) (Table 2). For the relationship between segmental colon transit time and the Leech score, as the right colon transit time increased, the stool retention score at the ascending colon increased, and as the left colon transit time increased, the stool retention score at the descending colon increased (p<0.01). However, there was no correlation observed between colon transit time and the stool retention score at the rectosigmoid colon (Table 3).
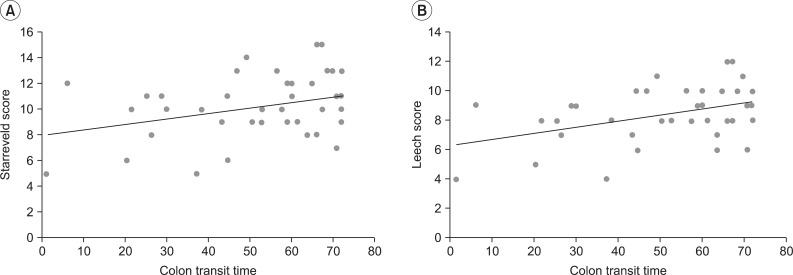
As the total colon transit time increased, both the Starreveld score (p<0.05) and Leech score (p<0.01) significantly increased, and this was a statistically significant positive correlation (Fig. 3).
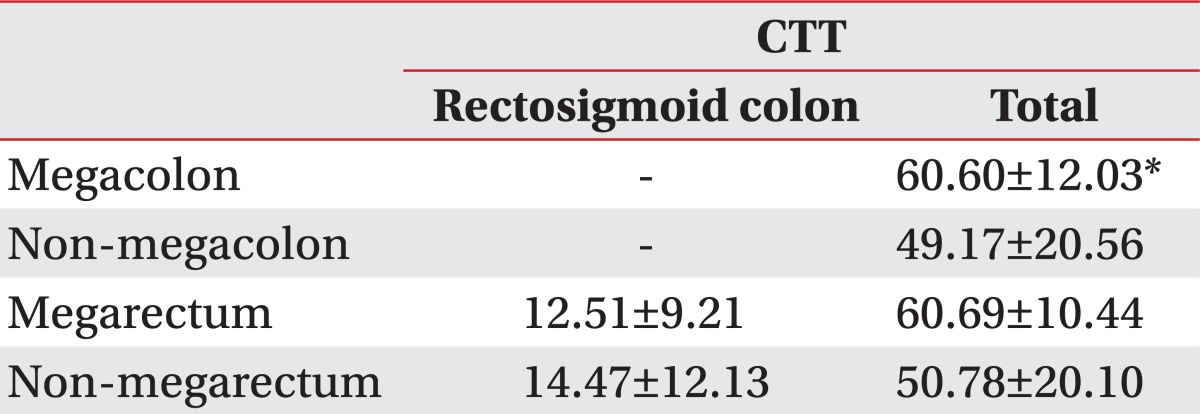
The total colon transit time in the two groups according to the presence/absence of megacolon was 60.60±12.03 for the megacolon group and 49.17±20.56 for the non-megacolon group, and this difference was statistically significant (p<0.05). The rectosigmoid colon and total colon transit times according to the presence/absence of megarectum did not show a statistically significant difference (Table 4).
Although bowel dysfunction due to a neurogenic bowel is a common complication [11,12], there have been relatively few studies on this problem compared with studies on respiratory and urinary complications [13]. This is because the medical implications of this problem are less severe and its complications tend to be less fatal. However, bowel dysfunction after SCI is not only difficult to treat properly but also requires continuous management. Thus, it is one of the most common and important problems that reduce the quality of life and delay social adjustment in patients [11,13,14].
Prior to the management of bowel dysfunction, it is important to accurately evaluate it. There are a few of methods known for such a purpose. The colon transit time is known as an objective method for evaluating the motility of the colon [15]. This study used it as comparison criteria for various evaluation methods of bowel dysfunction. The easiest and most widely used method is clinical assessment of the bowel pattern, which is usually conducted by history taking. However, assessment of the bowel pattern by history taking depends on subjective symptoms and the reports of patients. Furthermore there are reports [3] that people's memory of their bowel habit is sometimes inaccurate and is less related to the colon transit time, which has been proved to be an objective evaluation method. Thus, this method has limitations and the possibility of confounding by the inspector's subjective interpretation. Plain abdominal radiography is another method to evaluate bowel dysfunction, and is an inexpensive method and easy to use as a supplement to medical history taking and physical examination. It is also known through many studies that plain abdominal radiography is useful in evaluating bowel dysfunction. However, the studies on the usefulness of plain abdominal radiography in evaluating bowel dysfunction have been conducted on children. Although Starreveld et al. [4] reported that plain abdominal radiography is as useful as the colon transit time in adult patients with functional constipation in 1990, there has been no report on the usefulness of plain abdominal radiography in patients with SCI.
This study examined the constipation score using Rome II Diagnostic Criteria and the morphological stool characteristics using the Bristol stool form scale, analyzed the degree of stool retention using plain abdominal radiographs and measured the colon transit time, and evaluated the correlations among the these evaluation methods in order to assess the usefulness of plain abdominal radiography compared to other methods and to investigate its convenience in clinical application.
Plain abdominal radiography is a simple and less time-consuming evaluation method than others for evaluating the distribution of feces in the colon and the presence of megacolon. However, despite such advantages, the quantitative assessment of plain abdominal radiography has limitations, and the colon transit time is known as the most objective method for evaluating the motility of the colon.
The colon transit time has the advantage that it can evaluate total colon motility as well as segmental colon motility so it is used as an objective evaluation method of colonic motility in patients with SCI. However, it has the limitations of being complicated and time-consuming to perform.
This study found that the colon transit time was 19.3±16.17 for the right colon, 19.3±13.45 for the left colon, and 15.32±13.15 for the rectosigmoid colon. The total colon transit time was 52.42±19.14, which was long compared to the colon transit time of normal persons. There is a statistically significant correlation between the total colon transit time, the Starreveld score and the Leech score as measured by plain abdominal radiography. This study also found that there was a statistically significant correlation between the segmental colon transit time and the segmental stool retention score. These results suggest that not only the total colon transit time but also the segmental colon transit time may be inferred from plain abdominal radiographs which are as useful as the colon transit time for evaluating bowel dysfunction in patients with SCI.
But the rectosigmoid colon transit time was measured to be shorter than right colon and left colon. The rectosigmoid transit time showed a negative correlation with the transverse colon stool retention Starreveld score. However, for the Leech score, the rectosigmoid transit time showed no significant correlation with the stool retention score.
The reason may be that the subjects received bowel management and proper education about bowel control during the study period. At least once every two to three days of the bowel program, osmotic laxatives, enemas, suppositories, and digital disimpaction were used in order to induce a bowel movement. This is thought to have affected the rectosigmoid colon transit time, and further studies should exclude such bowel management.
In 2000, Harari and Minaker [16] reported on a study on patients with chronic SCI using plain abdominal radiography, and found that 73% of the patients had megacolon, and among them, 52% showed radiographical constipation. They also reported that megacolon was more frequently observed among patients who were elderly, had chronic SCI and abdominal distension, were taking anticholinergic medications or antacids containing calcium. This study found that 14 patients (31.8%) had megacolon and 11 patients (25%) had megarectum. All the cases of megacolon were found in the ascending colon. The reason that the incidence rate of megacolon was less in this study than in the study of Harari and Minaker [16] may be attributed to the fact that the subjects in this study were younger (average, 50.2 years), their prevalence period was shorter (average, 32 months), and most of them had received proper education on bowel control during their admission period.
Since the ability to perform activities of daily living is lower in patients with SCI than in normal persons, the convenience and simplicity of the evaluation method should be taken into consideration when selecting the evaluation method. For patients whose progress is monitored on an outpatient basis, it is not easy to assess the colon transit time due to the technique used or the time involved. Therefore, in order to evaluate bowel dysfunction on an outpatient basis, performing plain abdominal radiography in addition to doing a medical examination, instead of conducting a complicated colon transit time assessment, would provide information on total colonic motility and segmental colonic motility, especially on the examination day. Thus, it is very useful in terms of the patient's convenience. In addition, when severe stool retention or megacolon is observed on plain abdominal radiography, more active induction of bowel movements including the use of osmotic laxatives, and a variety of enemas and suppositories and performing digital disimpaction, should be employed.
When examining the degree of stool retention through plain abdominal radiography, there might be differences in the inspectors' interpretations. Therefore, 2 skilled radiologists familiar with this study's methods and procedures read the plain abdominal radiographs in our study. The observer variation between these 2 inspectors was assessed. The results showed that the 2 inspectors showed consistency in their evaluation of the degree of stool retention, and the presence/absence of megacolon or megarectum (p<0.01), which suggests that plain radiography may be useful as an objective test method if the inspectors are familiar with the reading criteria and receive proper training in interpreting the degree of stool retention. However, for the Starreveld score which analyzes the total colon after it is divided into 4 segments, there can be a case where the transverse colon overlaps with the ascending or descending colon when there is excessive stool in the transverse colon and this may produce judgment errors. Therefore, it may be easier to use the Leech score which uses 3 segments of the colon for the analysis.
And bowel management, such as the use of osmotic laxatives, enemas, suppositories, and digital disimpaction, affects primarily the rectosigmoid colon. Thus, there may be an error in measuring the rectosigmoid colon transit time and assessing the stool retention score. Colon transit time and stool retention score are measured by referring to the plain abdominal radiographs at 9:00 AM on the 4th day. Thus, the defecation time should be considered when evaluating plain abdominal radiographs of the rectosigmoid colon especially when defecation occurs just before the evaluation, as this affects the evaluation of the rectosigmoid colon greatly, compared to other parts of the colon.
The limitations of this study are that this study did not consider the dietary patterns of patients with SCI or other diseases that may affect bowel dysfunction, and it did not consider the medications used to control bowel dysfunction. This study also did not examine the correlations among evaluation methods using a control group. Finally, there was no statistical correlation between the bowel pattern identified by the constipation score and plain abdominal radiography. Further studies should address these limitations and use more subjects.
In conclusion, this study examined the usefulness of plain abdominal radiography in evaluating bowel dysfunction of patients with SCI. The study results showed that there were statistical correlations among the colon transit time, which is known as the most objective test to evaluate motility of colon, the Starreveld score and the Leech score as measured by plain abdominal radiography. Since plain abdominal radiography is simple and less time-consuming and involves less radiation than other radiological techniques, it is a useful method in evaluating bowel dysfunction, managing the bowel and establishing a treatment plan for patients with SCI. It is also a highly convenient method to use for patients with SCI, and can be easily applied in clinical practice.
References
1. Coggrave M, Norton C, Wilson-Barnett J. Management of neurogenic bowel dysfunction in the community after spinal cord injury: a postal survey in the United Kingdom. Spinal Cord. 2009; 47:323–330. PMID: 19015665.

2. Seo JH, Song KS, Ko MH, Park SH. The change of neurogenic bowel dysfunction in spinal cord injury patients during admission. J Korean Acad Rehabil Med. 2009; 33:441–447.
3. Ashraf W, Park F, Lof J, Quigley EM. An examination of the reliability of reported stool frequency in the diagnosis of idiopathic constipation. Am J Gastroenterol. 1996; 91:26–32. PMID: 8561138.
4. Starreveld JS, Pols MA, Van Wijk HJ, Bogaard JW, Poen H, Smout AJ. The plain abdominal radiograph in the assessment of constipation. Z Gastroenterol. 1990; 28:335–338. PMID: 2238762.
5. Halligan S, Bartram CI. The radiological investigation of constipation. Clin Radiol. 1995; 50:429–435. PMID: 7614787.

6. Leech SC, McHugh K, Sullivan PB. Evaluation of a method of assessing faecal loading on plain abdominal radiographs in children. Pediatr Radiol. 1999; 29:255–258. PMID: 10199902.

7. Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Muller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999; 45(Suppl 2):II43–II47. PMID: 10457044.

8. Heaton KW, Radvan J, Cripps H, Mountford RA, Braddon FE, Hughes AO. Defecation frequency and timing, and stool form in the general population: a prospective study. Gut. 1992; 33:818–824. PMID: 1624166.

9. Arhan P, Devroede G, Jehannin B, Lanza M, Faverdin C, Dornic C, et al. Segmental colonic transit time. Dis Colon Rectum. 1981; 24:625–629. PMID: 7318630.

10. Margulis AR, Burhenne HJ. Practical alimentary tract radiology. Boston: Mosby Year Book;1993.
11. Glickman S, Kamm MA. Bowel dysfunction in spinal-cord-injury patients. Lancet. 1996; 347:1651–1653. PMID: 8642958.

12. Ng C, Prott G, Rutkowski S, Li Y, Hansen R, Kellow J, et al. Gastrointestinal symptoms in spinal cord injury: relationships with level of injury and psychologic factors. Dis Colon Rectum. 2005; 48:1562–1568. PMID: 15981066.

13. De Looze DA, De Muynck MC, Van Laere M, De Vos MM, Elewaut AG. Pelvic floor function in patients with clinically complete spinal cord injury and its relation to constipation. Dis Colon Rectum. 1998; 41:778–786. PMID: 9645749.

14. Keshavarzian A, Barnes WE, Bruninga K, Nemchausky B, Mermall H, Bushnell D. Delayed colonic transit in spinal cord-injured patients measured by indium-111 Amberlite scintigraphy. Am J Gastroenterol. 1995; 90:1295–1300. PMID: 7639233.
15. Keighley MR, Henry MM, Bartolo DC, Mortensen NJ. Anorectal physiology measurement: report of a working party. Br J Surg. 1989; 76:356–357. PMID: 2720345.

16. Harari D, Minaker KL. Megacolon in patients with chronic spinal cord injury. Spinal Cord. 2000; 38:331–339. PMID: 10889561.

Fig. 1
Starreveld score (A) and Leech score (B) for each segment were evaluated by plain abdominal radiographs.
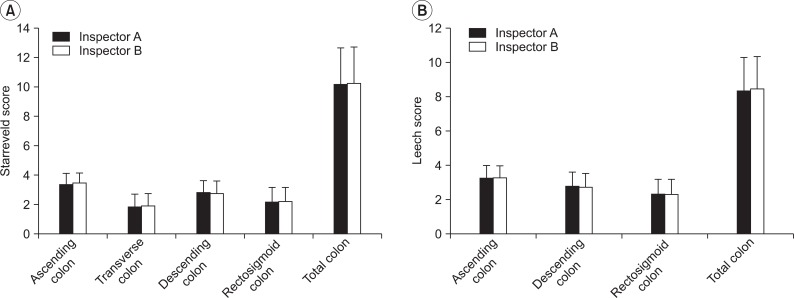
Fig. 2
The inter-inspector reliability for the Starreveld score (A) and Leech score (B). There was a statistically significant correlation between the interpretations of the inspectors (r=0.913, r=0.922).
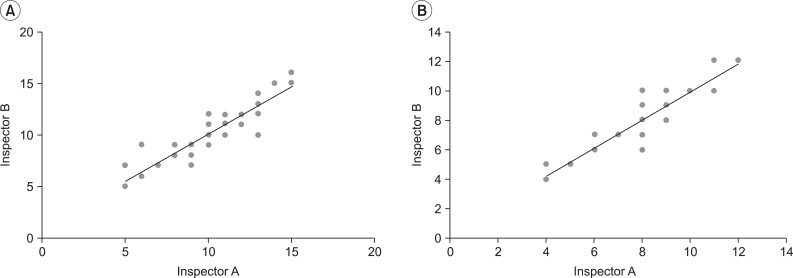
Fig. 3
The correlation of the total colon transit time (CTT) between Starreveld score (A) and Leech score (B). There was a statistically significant correlation between the methods (r=0.323, r=0.426).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download