Abstract
We report a case of a 44-year-old patient with paralysis of the left leg who had a thoracic epidural catheterization after general anesthesia for abdominal surgery. Sensory losses below T10 and motor weakness of the left leg occurred after the surgery. Magnetic resonance image study demonstrated a well-defined intramedullary linear high signal intensity lesion on T2-weighted image and low-signal intensity on T1-weighted image in the spinal cord between T9 and L1 vertebral level, and enhancements of the spinal cord below T8 vertebra and in the cauda equina. Electrodiagnostic examination revealed lumbosacral polyradiculopathy affecting nerve roots below L4 level on left side. We suggest that the intrinsic spinal cord lesion and nerve root lesion can be caused by an epidural catheterization with subsequent local anesthetic injection.
Epidural catheterization is widely used for postoperative pain controls, and is generally regarded as safe and effective [1]. Complications may occur, however, due to the induced epidural catheterization, including epidural hematoma, abscess, spinal cord infarction, neurotoxicity by the anesthetics, and direct spinal cord injury [2]. Persistent and severe paralysis resulting from these complications has rarely been reported, and especially reports of neurologic deficits resulting from direct injury to the spinal cords caused by needles or catheters have been extremely rare [2-4]. Nevertheless, direct injury to the spinal cord caused by needles or catheters used has been reported [5]; a case of intrinsic spinal cord lesion accompanied by nerve roots injury is being reported in South Korea. Reported herein is a case of a patient who was presumed to have intrinsic spinal cord lesion accompanied by nerve roots injury caused by thoracic epidural catheterization, together with literature review.
A 44-year-old woman (height, 162 cm; weight, 51 kg) was admitted to the Department of Surgery at this hospital for an extended right hemicolectomy due to colonic intussusceptions caused by cecal lipoma. Upon admission, the patient's vital signs were normal, and the patient had no history of any other diseases. Epidural catheterization was performed to achieve postoperative pain controls. As the patient was nervous and uncooperative, an epidural block was performed after general anesthesia. The median approach was used, and the epidural space was located using an 18-gauge Tuohy needle and the loss of resistance to air technique between the T12 and L1 spinous processes. On the first needle insertion attempt, increased resistance was felt as the needle entered the ligamentum flavum, followed by loss of resistance with injection of air as the needle was advanced to a depth of about 4 cm from the skin. After confirming that there was no cerebrospinal fluid (CSF), a 20-gauge epidural catheter (Perifix epidural catheterization set; B. Braun Melsungen AG, Melsungen, Germany) was inserted 5 cm further into the epidural space, and the catheter was placed with little resistance. An epinephrine injection was not conducted as the epidural catheter was being mislocated in the blood vessel. After the successful placement of the epidural catheter, a total volume of 20 mg of 0.5% levobupivacaine (Chirocaine; Abbott Korea Ltd., Seoul, Korea) and fentanyl (Fentanyl Citrate; Guju Pharm Co. Ltd., Seoul, Korea) 50 µg was administered, and a patient-controlled analgesia pump ambulatory infusion pump (Woo Young Medical Co. Ltd., Seoul, Korea) was connected to the epidural catheter. The pump was programmed to deliver 300 mg of 0.5% levobupivacaine with morphine (Highmol; BCworld Pharm Co. Ltd., Seoul, Korea) 20 mg, alfentanyl (Alfentanil; Hana Pharm Co. Ltd., Seoul, Korea) 6 mg, ondansetron (Onsetron; BoRyung Pharm, Seoul, Korea) 8 mg, and normal saline 47 mL at a rate of 2 mL/h.
Although the patient's postoperative vital signs were stable, she complained of feeling weakness, hypesthesia, and numbness of the lower left limb after gaining her conscious. The epidural pump infusion was thus discontinued, and the epidural catheter was removed as the symptoms persisted the following day. On postoperative day 9, the neurologic assessment that was performed in accordance with the consultation with the Department of Rehabilitation Medicine revealed decreased touch, pain, and temperature sensations as well as preservation of vibration sensation and proprioception in the dermatomes from T11 to S4-5, on the lower left limb. Although manual muscle testing showed that the muscle strengths of the upper and right lower extremities were normal, the muscle strength in the left lower extremities decreased to 4/5 in the hip flexors and extensors, 2/5 in the knee flexors, 4/5 in the knee extensors, and 0/5 in the ankle dorsiflexors and plantar flexors. The ankle jerk of both sides and the knee jerk on the left side also decreased, and Babinski reflex and ankle clonus were not observed on both sides. Although digital rectal examinations revealed that the construction of the anal sphincter had slightly diminished, the patient did not complain of changes in her bladder and bowel functions. No symptom of infection (e.g., fever) was seen, and no abnormal findings were reported according to the hematology, including blood test and liver function and urinalysis test.
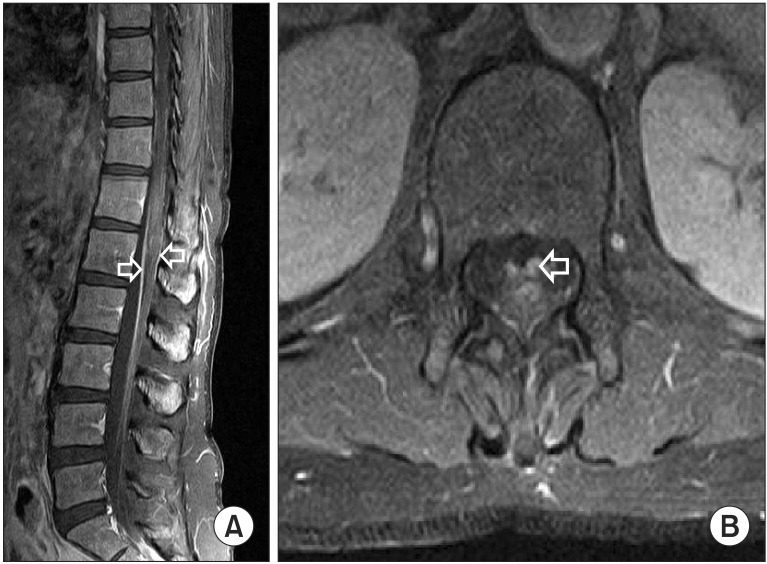
On the 9th postoperative day, the magnetic resonance imaging (MRI) of thoracolumbar spine was performed. It revealed well-defined intramedullary linear high-signal-intensity lesion at the sagittal T2-weighted images and low-signal-intensity lesion at the T1-weighted images, in the left spinal cord between T9 and the L1 vertebral level. Also, the T1-enhanced images showed minimal enhancements in the spinal cord between T9 and the L1 vertebral level, and diffuse enhancements in the spinal cord below the T12 vertebral level and in the cauda equina (Figs. 1, 2).
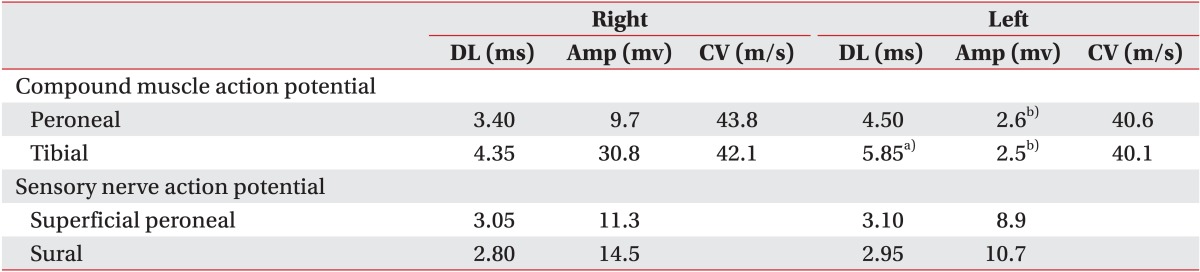
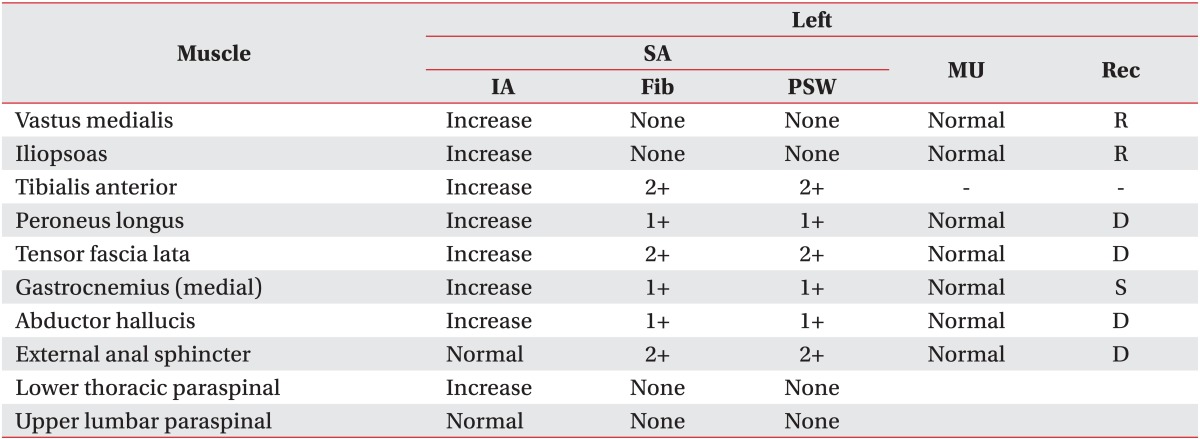
Electrodiagnostic examination was performed on postoperative day 22. Although the sensory-nerve conduction study of the lower extremities on both sides was normal, and the motor nerve conduction study of right peroneal and tibial nerves was normal, the amplitude of the compound motor action potentials in the left peroneal and tibial nerve decreased, and the latency of the left tibial nerve was delayed. The somatosensory-evoked potentials of both tibial nerves and the motor-evoked potentials of the lower right extremities were within the normal range while the motor-evoked potentials recorded in the left abductor hallucis muscle and tibialis anterior muscle were not evoked. Electromyography showed a finding of denervation below the L4 myotome, and consequently, electrodiagnostic examination demonstrated a finding that was consistent with the lumbosacral radiculopathy below L4 nerve roots on the left side (Tables 1, 2).
In review of the clinical findings, according to the outcomes of the imaging studies and electrodiagnostic examinations, it was supposed that the intrinsic spinal cord lesion caused by the epidural catheterization was accompanied by nerve roots injuries below L4 on the left side. The follow-up MRI of the thoracolumbar spine that was performed nine weeks later did not show new lesions, and the high-signal-intensity lesions on the previous T2-weighted images and the enhanced lesions on the T1-enhanced images were found to have decreased considerably. In addition, the nerve conduction study that was performed at postoperative week 10, revealed that the amplitude of the compound motor action potentials in the left peroneal nerve and tibial nerve increased as compared with that in the previous outcome. The motor-evoked potentials of the left abductor hallucis muscle and the left tibialis anterior muscle were evoked, and that the motor unit action potentials of the left tibialis anterior muscle which were not seen in the electromyography were being observed, demonstrating improvement of the lumbosacral radiculopathy below L4 nerve root on the left side.
After a period of about three months, with the muscle strengths of the hip flexor, extensor, and knee extensor, have recovered to normal levels, and those of the ankle dorsiflexor and plantar flexor, which have recovered to 2/5. The patient, who can now walk independently using an ankle-foot orthosis, is already getting strengthening exercises on lower muscular extremities in left side and gait trainings. Moreover, the patient is complaining of neuropathic pain in the left hip and dorsum of foot. A physical agent modalities and pharmacologic treatments are offered for pain control.
Epidural anesthesia may result in several complications, but persistent and severe neurological complications are rarely being reported, with an incidence rate of between 0.006% and 0.03% [2-4]. The causes of this injury include compression of the spinal cord or nerve root by an epidural hematoma or abscess, chemically-induced subarachnoiditis, spinal cord infarction, neurotoxicity of the infused anesthetic drugs, migration of the inserted catheters, and direct injury to the spinal cord caused by inappropriate needle or catheter insertion [2].
In this case report, the well-defined intramedullary left-sided linear lesion extended to many segments was observed on the T2-weighted MRI image of the thoracolumbar spine and could be differentiated from the bilateral hyperintense in the central gray matter (central "owl's eye" pattern) showing typical pattern observed in spinal cord infarction. The inflammatory diseases that display well-defined intramedullary linear high-signal-intensity lesions on the T2-weighted MRI images of the spine are multiple sclerosis, acute transverse myelitis, and acute disseminated encephalomyelitis. Although absolute exclusion is not feasible, the case reported herein can be differentiated from multiple sclerosis in that lesions were found in two or more vertebral segments, from acute transverse myelitis in that the symptoms developed unilaterally, and from acute disseminated encephalomyelitis in that there were no premonitory symptoms (e.g., fever, myalgia) or symptoms of brain intrusion. Furthermore, as symptoms developed after the surgery, the possibility of the existence of these inflammatory diseases was low. As there was no low back pain, and as thickening and clumping of the nerve roots and adhesion of the nerve roots to the dura ("empty sac sign") were not observed on the MRI images, the possibility of lumbar subarachnoiditis caused by blood after epidural anesthesia can be excluded. Moreover, as there were no findings suggesting infection, such as fever, chilling, or abnormal hematological findings, the possibility of infectious diseases existing can be excluded [6].
The intrinsic spinal cord lesion at the insertion site of the epidural catheter can be attributed due to the direct penetration into the spinal cord of the epidural catheter, and to the physicochemical impairment caused by the persistent infusion of drugs. Also, the intrinsic cord lesion with more wide segments than the point of catheter insertion in MRI is presumed to have occurred due to the high fluid pressures exerted on the spinal cord by the intraspinal cord infusion of drugs [3].
Considering the clinical observation of flaccid paralysis and the electrodiagnostic findings, it is presumed that the intracord lesion earlier mentioned was accompanied by nerve roots injury caused by the local anesthetics. The neurotoxic effects of local anesthetics depend on the dose and the time of exposure, and it has been reported that a high dose of a local anesthetic in greater volumes will result in neurotoxicity [7]. To date, the nerve injury caused by local anesthetics is supposed to have resulted from the permeability changes around the nerve, the swelling of nerve fascicles, and the dysfunction and injury to the nerve fibers caused by the increased pressure in the endometrium [8]. In this case report, together with the clinical observations and the electrodiagnostic findings, the T1-weighted MRI images revealed enhancement in the spinal cord below the T8 vertebral segment and in the cauda equine. It is believed that this resulted from the physical compressions caused by the persistent infusion of drugs after the insertion of the catheter, and from the inflammatory responses caused by the local anesthetics. Therefore, it is supposedly accompanied by nerve roots injury, which is also caused by such mechanism.
Assuming the pathogenesis of the patient, a catheter was inserted unilaterally into the left side during the procedure, resulting in partial injury to the left spinal cord. Yet, as the lateral spinothalamic tract of the left spinal cord was preserved, the patient did not complain of diminished pains and temperature sensations on the right. And, as the posterior column of the left spinal cord was also preserved, the vibration sensation and proprioception on the left were preserved. The symptoms of diminished touch, pain, and temperature sensations on the left side and the flaccid paralysis, can be attributed to the nerve roots injury caused by the swelling at the catheter insertion site, and by the infused drugs. Despite the fact that the damage to the left nerve roots can be attributed among the nerve fibers entering the left dorsal entry zone, and the damage to the large myelinated nerve fibers are associated with vibration sensation and proprioception, the preservation of the vibration sensation and proprioception on the lower left extremities are located in the medial division. Thus, being less than damage to the unmyelinated nerve fibers which are associated with pain and temperature sensations and located in the lateral divisions.
The optimal time for performing epidural anesthesia during combined epidural and general anesthesia has remained controversial [9]. Although, to date, there are insufficient data supporting the assumption of increased risks of epidural catheterization under general anesthesia for adults, it is believed that it is best to perform epidural catheterization in patients upon awakening [3-5]. When catheterization is performed in awoken patients, if the needle is found to have penetrated the spinal cord or nerve root, symptoms such as local or radiating pain, decreased sensation, or involuntary movements may occur during the epidural catheterization and then the procedure should be immediately be halted, with identification of the response, which may lead to the decreased incidence of complications.
High doses of methylprednisolone within eight hours of the injury occurrence in the treatment of spinal cord or nerve roots injury are known to improve the neurological outcome [10]. As no adverse findings such as CSF leak-age were reported during the epidural catheterization of the patient in this case report, it was predicted that direct injury to the spinal cord caused by needles or catheters would not occur. The MRI performed nine days after the development of neurologic deficits, however, revealed the finding of direct injury to the spinal cord caused by the needles or catheters used. If injuries of the spinal cord or nerve roots were considered following rapid radiologic evaluation, for findings of neurologic deficit, it is believed that methylprednisolone administration will help alleviate the patient's symptoms.
Although neurologic complications caused by epidural catheterization are rare, they may leave persistent and severe neurologic deficits in the patient. It is thus best to perform epidural catheterization in awoken patients to prevent these complications, and extra vigilance must be observed in the follow-up of the neurologic deficits after the procedure. In addition, if there are symptoms of neurologic deficits, possible injuries of the spinal cord or nerve roots should be considered, followed by rapid radiologic evaluation and the appropriate treatment.
References
1. Ahn JS, Kim SJ, Kim EG. A case of intrinsic spinal cord lesions complicating epidural anesthesia. J Korean Neurol Assoc. 2006; 24:181–183.
2. Wheatley RG, Schug SA, Watson D. Safety and efficacy of postoperative epidural analgesia. Br J Anaesth. 2001; 87:47–61. PMID: 11460813.

3. Wilkinson PA, Valentine A, Gibbs JM. Intrinsic spinal cord lesions complicating epidural anaesthesia and analgesia: report of three cases. J Neurol Neurosurg Psychiatry. 2002; 72:537–539. PMID: 11909921.
4. Kao MC, Tsai SK, Tsou MY, Lee HK, Guo WY, Hu JS. Paraplegia after delayed detection of inadvertent spinal cord injury during thoracic epidural catheterization in an anesthetized elderly patient. Anesth Analg. 2004; 99:580–583. PMID: 15271743.

5. Seo KC, Kim JE, Kim JH, Song SY, Chung JY, Roh WS. Injury to the spinal cord by a thoracic epidural catheter used to control postpneumonectomy pain: a case report. Korean J Anesthesiol. 2009; 56:720–724.
6. Ross JS, Moore KR, Shah LM, Borg B, Crim J. Diagnostic imaging: spine. 2nd ed. Altona: Amirsys;2010.
7. Jeong JS, Park KD, Lim OK. A case report of persistent cauda equina syndrome following epidural anesthesia. J Korean Assoc EMG Electrodiagn Med. 2009; 11:151–155.
8. Han KD, Jeong YJ, Lim SA. Cauda equina syndrome following epidural anesthesia: a case report. Korean J Anesthesiol. 1998; 35:786–790.

9. Fischer HB. Regional anaesthesia: before or after general anaesthesia? Anaesthesia. 1998; 53:727–729. PMID: 9797514.
10. Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med. 1990; 322:1405–1411. PMID: 2278545.
Fig. 1
Magnetic resonance T2-weighted imaging of the thoracolumbar spine. Sagittal T2-weighted image (A) and axial T2-weighted image (B) reveal well-defined intramedullary linear high signal intensity (arrow) on the left side between T9 and L1 vertebral level of spinal cord.
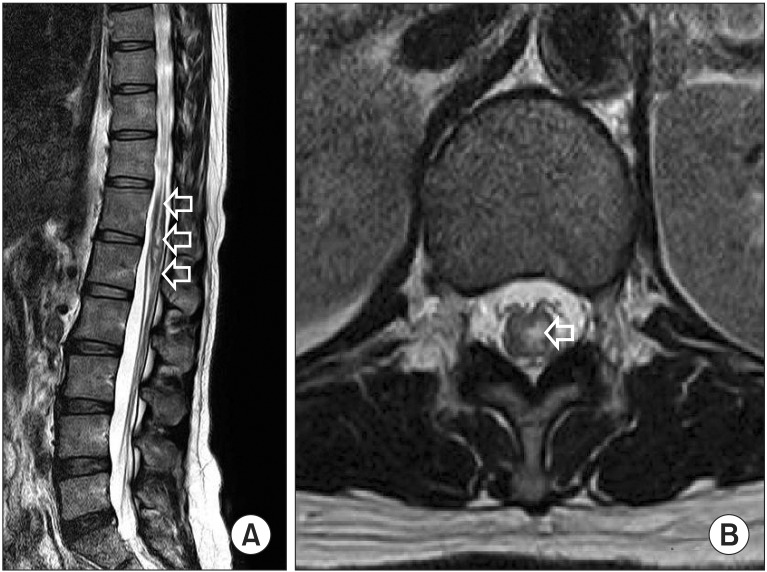
Fig. 2
Magnetic resonance T1-enhanced imaging of thoracolumbar spine. Sagittal T1-enhanced image (A) and axial T1-enhanced image (B) show enhancement (arrow) in the spinal cord between T9 and L1 vertebral level, and diffuse enhancement of the spinal cord below T12 vertebral level and in the cauda equine.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download