Abstract
Lofgren's syndrome is an acute form of sarcoidosis characterized by erythema nodosum, bilateral hilar lymphadenopathy (BHL), and polyarthralgia or polyarthritis. This syndrome is common among Caucasians but rare in the Korean population. A 44-year-old woman was admitted to our hospital complaining of polyarthralgia. A chest radiograph revealed BHL and nodular shadows. Angiotensin-converting enzyme levels were within the normal range. Tissue biopsy from a mediastinum lymph node showed noncaseating granulomas. We diagnosed her with Lofgren's syndrome, an acute form of sarcoidosis.
Go to : 
Sarcoidosis is a multi-systemic granulomatous disease with an unknown etiology characterized by its pathological hallmark [1]. The lungs are the most frequently affected organ (>90%), along with the skin, eyes, liver, and lymph nodes as other involved organs. Clinical features of joint involvement are found in 14% of cases at presentation and up to 38% during follow-up [2]. The frequency of muscle and bone involvement at presentation is low (1%) at initial diagnosis but is found in 5%-13% of patients during follow-up [2]. One particular type of joint involvement is acute sarcoid arthritis (Lofgren's syndrome) which is described as a symmetric polyarthritis associated with hilar adenopathy with or without erythema nodosum (EN) [3]. Case reports of Lofgren's syndrome often describe women of Northern European, Irish, and Japan descent. To our knowledge, there has been only one report of Korean patients with Lofgren's syndrome, and most of their symptoms involved the skin [4]. We herein present a case of a 44-year-old woman with polyarthralgia who was diagnosed with Lofgren's syndrome.
Go to : 
A 44-year-old woman was admitted to our hospital in June 2011 complaining of arthralgia in both knees, elbows, and ankles. She had been diagnosed with hepatic cysts 10 years ago but was healthy before the appearance of bilateral polyarthritis of the knees 1 month before admission. She went to a nearby orthopedic clinic and reported temporary alleviation of the knee pain upon taking non-steroidal anti-inflammatory drugs (NSAIDs).
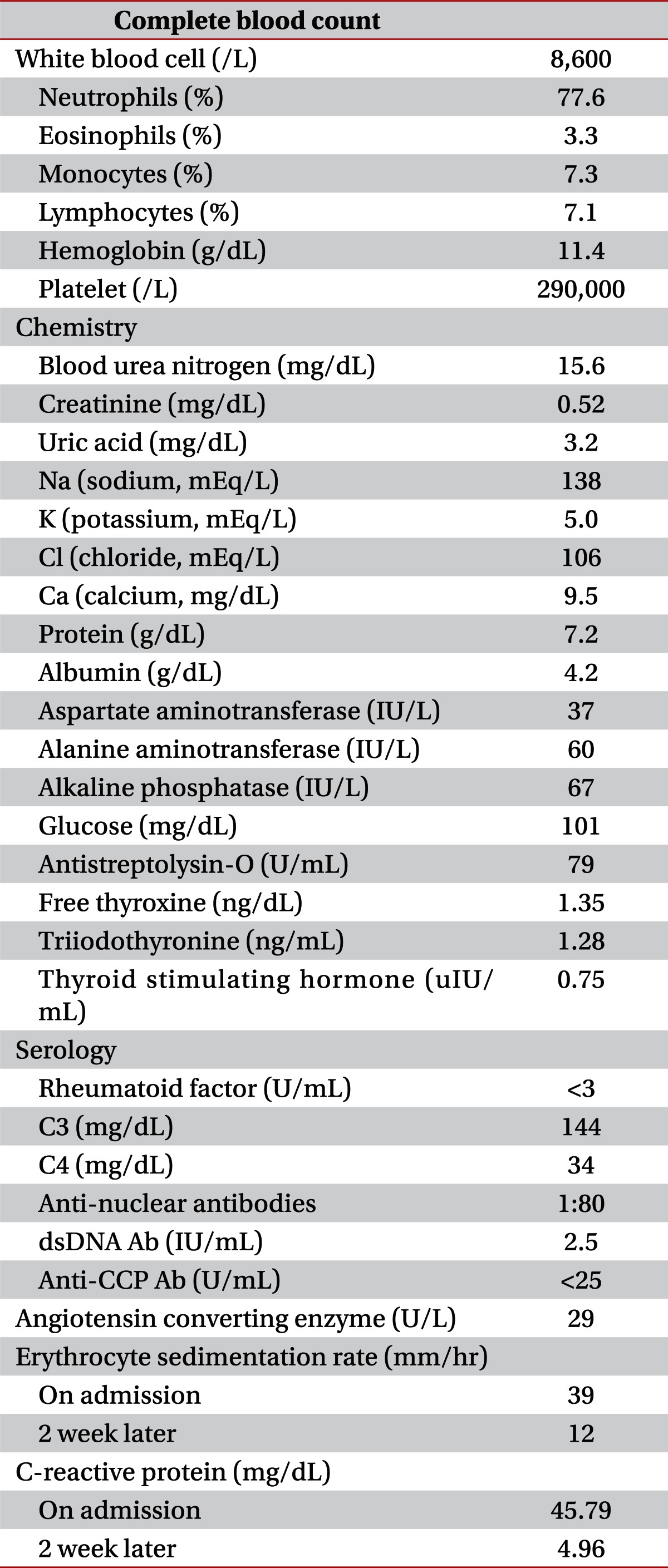
A physical examination showed mild swelling and tenderness in both ankles without limitation of range of motion. Laboratory studies showed elevated erythrocyte sedimentation rate (ESR, 39 mm/hr) and C-reactive protein level (CRP, 45.79 mg/L) (Table 1). White blood cell count was 8,600/L, blood hemoglobin was slightly low at 11.4 g/dL, and platelet count was 290,000/L. The serum angiotensin-converting enzyme (ACE) level was (29.0 IU/L; normal range, 7.7-29.4 IU/L). Aspartate aminotransferase (AST) and alanine transaminase (ALT) levels were slightly high at 37 IU/L and 60 IU/L, respectively. She was negative for rheumatoid factor and anti-cyclic citrullinated peptide (anti-CCP) antibody. Her C3 level was 144 mg/dL, C4 was 34 mg/dL, and antinuclear antibody was positive at a titer of 1:80 (homogeneous and fine cytoplasmic granules pattern), but specific antibodies were not detected (Table 1).
Knee, ankle, hip, and hand X-ray findings showed periarticular osteoporosis (Fig. 1). Ultrasonography findings suggested polyarticular inflammatory synovitis of both knees, elbows, ankles, with a combined partial tear of common extensor tendons in both elbows.
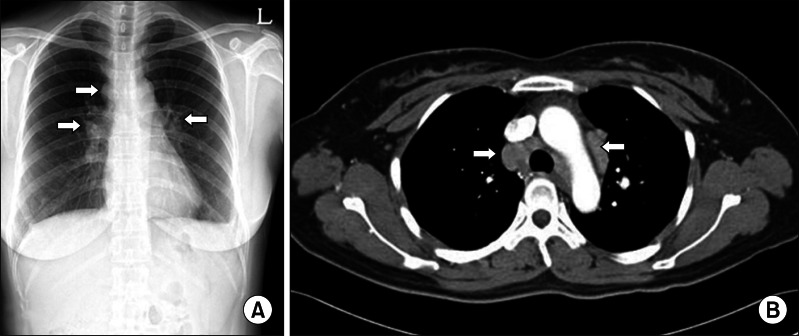
Chest X-ray findings showed focal mediastinal widening in both the hilum and the right upper trachea (Fig. 2A), and chest computed tomography scan indicated multiple enlarged lymph nodes of the mediastinum and both hila (Fig. 2B). The bone scan showed mildly increased uptake in bilateral hands, wrists, and other small joint areas (Fig. 3).
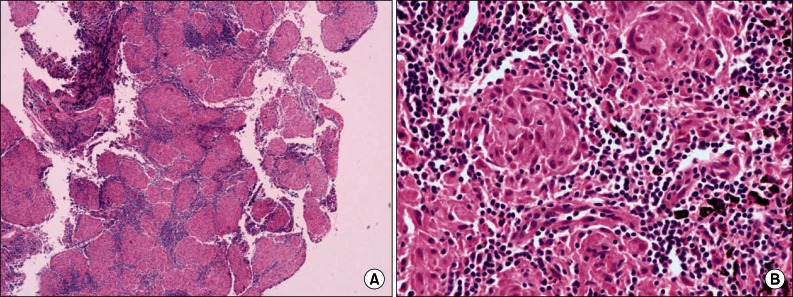
A mediastinoscopic lymph node biopsy was performed. The obtained tissues of mediastinal lymph nodes showed noncaseating granuloma of epithelioid cells and the presence of giant cells (Fig. 4).
Based on the bilateral hilar lymphadenopathy (BHL) with polyarthralgia, the patient was diagnosed with Lofgren's syndrome, although EN. NSAID treatment did not alleviate her symptoms for 1 week. Oral administration of prednisolone (10 mg/day) was initiated. The pain resolved within 1 week, and the levels of ESR and CRP were normalized after 2 weeks (12 mm/hr, 4.96 mg/L). The prednisolone dose was lowered 1 month later (5 mg/day). The pain and joint swelling were improved, but she sometimes felt mild pain in the joints, and BHL was still seen on simple chest radiography after 2 months. For these reasons, prednisolone administration has been continued for 8 months until now. No recurrence has been observed since then.
Go to : 
While sarcoidosis occurs worldwide, higher annual incidence rates have been reported among United States Blacks, the Irish, and Scandinavians [1]. On the basis of cumulative incidence estimates, the lifetime risk of sarcoidosis for United States Blacks is 2.4% and that for United States Whites 0.85% [1]. In Korea, sarcoidosis is a rare disease with the incidence rate being 0.125 per 100,000 and Lofgren's syndrome is even more rarely reported [4,5].
Acute polyarthritis occurs in 10% to 39% of patients with sarcoidosis, particularly in the early phases of the disease, which could be the presenting feature. BHL is almost invariably present in patients with acute sarcoid arthritis; fever and EN are present in 90% and 60% of the cases, respectively [6,7].
In 1953, Lofgren characterized 212 adult patients of BHL who were practically regarded as having sarcoidosis based on the absence of tuberculosis. Lofgren demonstrated that EN was present at the onset of the disease in 113 cases in which articular symptoms were common (101 cases, 89%). There was either pain only in the joints (20%), or pain accompanied by swelling (69%) [8].
Arthritis in sarcoidosis is usually symmetrical; the ankles are involved in more than 90% of the cases; the knees, small joints of the hands or feet, wrists, and elbows are involved in 15% to 40% [5,7,9]. Local pain, soft-tissue swelling, periarticular tenderness, edema, and joint effusion may be present [6]. Radiographs are normal or reveal only soft-tissue swelling [6]. ESR or CRP level is elevated in >80% of patients with acute sarcoid polyarthritis [6,7]. Serum ACE level is usually increased, and rheumatoid factor is negative. Synovial fluid in sarcoid arthritis reveals lymphocytosis and elevated protein levels [6,7].
Diagnosis of Lofgren's syndrome is not complicated but straightforward when the characteristic triad (BHL, polyarthritis, and EN) is present. Nevertheless, the disease may be somewhat difficult to diagnose because variant forms of this syndrome are often observed. In addition, uveitis and elevated levels of ACE, although useful clues for diagnosing sarcoidosis, are often absent in patients with Lofgren's syndrome (eye involvement, 5%; elevated ACE levels, 50%) [9].
Lofgren's syndrome is described as a symmetric polyarthritis associated with hilar adenopathy with or without EN. Regarding the case described herein, the patient showed polyarthritis, but not EN. Among 49 patients studied by Gran et el. [3], all patients had peripheral arthritis and hilar adenopathy, and 87.8% presented with EN. Sato et al. [10] summarized the reported 13 patients of Lofgren's syndrome in Japan. BHL was observed in almost all patients (85%), but EN was not observed in 38% of the patients. These facts underscore the difficulty of diagnosing Lofgren's syndrome. Biopsy must be done for differential diagnosis. Because peripheral lymphadenopathy was not found in this patient, biopsy of the lymph nodes by mediastinoscopy was necessary to support the diagnosis of sarcoidosis.
Lofgren's syndrome was regarded as a self-limiting disease that is generally resolved within the first year, with the mean duration ranging from 3 weeks to 3.7 months [3,9]. However, 8% of patients had active symptoms two years after the onset; 6% had episodes of recurrent sarcoidosis 2.20 years after the diagnosis [8]. NSAIDs or colchicine may be effective for mild cases. For more severe cases, oral corticosteroids are warranted [7]. In the present patient, acute manifestations of the musculoskeletal symptoms were refractory to NSAIDs initially but responded quickly to the later administration of prednisolone. The patient's CRP and ESR levels were normalized, showing a favorable therapeutic effect for Lofgren's syndrome.
Polyarthralgia and EN are often observed in various collagen diseases, including rheumatoid arthritis. Thus, Lofgren's syndrome, an acute form of sarcoidosis, must be differentially diagnosed. It is also noteworthy that, in Korean patients with Lofgren's syndrome, the characteristic triad is not always present. Biopsy from skin rash, lung nodules or lymph nodes should be considered in order to reach an early and precise diagnosis.
Go to : 
References
2. Jansen T, Geusens P. Sarcoidosis: joint, muscle and bone involvement. Eur Respir Monogr. 2005; 32:210–219.

3. Gran JT, Bohmer E. Acute sarcoid arthritis: a favourable outcome? a retrospective survey of 49 patients with review of the literature. Scand J Rheumatol. 1996; 25:70–73. PMID: 8614769.
4. Yang SG, Suh DH, Cho KH. A case of Lofgren's syndrome. Korean J Dermatol. 1995; 33:931–934.
6. James DG, Neville E, Carstairs LS. Bone and joint sarcoidosis. Semin Arthritis Rheum. 1976; 6:53–81. PMID: 785605.

7. Zisman DA, Shorr AF, Lynch JP 3rd. Sarcoidosis involving the musculoskeletal system. Semin Respir Crit Care Med. 2002; 23:555–570. PMID: 16088651.

8. Lofgren S, Lundback H. The bilateral hilar lymphoma syndrome; a study of the relation to tuberculosis and sarcoidosis in 212 cases. Acta Med Scand. 1952; 142:265–273. PMID: 14932794.
9. Mana J, Gormez-Vaquero C, Montero A, Salazar A, Marcoval J, Valverde J, et al. Lofgren's syndrome revisited: a study of 186 patients. Am J Med. 1999; 107:240–245. PMID: 10492317.
10. Sato T, Tsuru T, Hagiwara K, Miyashita K, Matsuno H, Goto A, et al. Sarcoidosis with acute recurrent polyarthritis and hypercalcemia. Intern Med. 2006; 45:363–368. PMID: 16617186.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download