Abstract
Myeloid sarcoma is a solid, extramedullary tumor comprising of immature myeloid cells. It may occur in any organ; however, the invasion of peripheral nervous system is rare. Herein, we report the case of myeloid sarcoma on the brachial plexus. A 37-year-old woman with acute myelogenous leukemia achieved complete remission after chemotherapy. One year later, she presented right shoulder pain, progressive weakness in the right upper extremity and hypesthesia. Based on magnetic resonance images (MRI) and electrophysiologic study, a provisional diagnosis of brachial plexus neuritis was done and hence steroid pulse therapy was carried out. Three months later the patient presented epigastric pain. After upper gastrointestinal endoscopy, myeloid sarcoma of gastrointestinal tract was confirmed pathologically. Moreover, 18-fluoride fluorodeoxyglucose positron emission tomography showed a fusiform shaped mass lesion at the brachial plexus overlapping with previous high signal lesion on the MRI. Therefore, we concluded the final diagnosis as brachial plexopathy due to myeloid sarcoma.
Myeloid sarcoma is one of the solid tumors comprising of malignant myeloid precursor cells that are myeloblasts and it is an extramedullary manifestation of myelogenous leukemia. Myeloid sarcoma is also called chloroma originating from 'chloros', a Greek word meaning 'green' because sometimes it becomes greenish due to the presence of myeloperoxidase and is also called as myeloblastoma or granulocytic sarcoma [1]. While myeloid sarcoma may occur at almost all the anatomical locations including the skin, lymph nodes, spine, gastrointestinal tract, orbit and breasts, it mostly occurs in bone and lymphatic tissues and its expression in nerves; in particular, in the nerve plexus is very rare [2].
The authors experienced a case of myeloid sarcoma expressing as brachial plexopathy and thus report it along with relevant literature review in the present work.
A 38-year-old female patient visited the hospital on February 19th, 2008 due to sub-acute radiating pain in the right upper extremity, which had occurred for continuous two or three days two months before the visit and right upper extremity weakness and sensory deficit, which had occurred around ten days before the visit as chief complaints. In the case history, she reported radiating pain that radiated from the right scapula along the medial surface of the right upper extremity and decrease in tactile senses in the right axilla, the medial surface of the right upper extremity, hypothenar in the hand and in the fifth finger as sensory symptoms. As motor symptoms, she reported weakness in her shoulders to the extent that she had difficulties in raising her arms and she could not use a spoon or chopsticks due to decreased hand muscle strength.
Based on her past history, she was treated by the department of gynecology and the department of internal medicine in another hospital in the early October 2006 due to profuse menstruation as a chief complaint, also she was diagnosed with acute monoblastic leukemia (AMoL or AML-M5) through a peripheral blood smear and a bone marrow biopsy smear examination. Thereafter, she was transferred to the internal medicine department of Samsung Medical Center. An immunohistochemical staining conducted again showed positive findings of CD13, CD14, CD15, CD33, CD54, CD64, CD117, and myeloperoxidase and a chromosomal study showed 46, XX, t(16;21), and positive findings of the translocated in liposarcoma/fused in sarcoma-ETS related gene (TLS/FUS-ERG). From October 29th, 2006, remission induction therapy was conducted along with idarubicin and cytarabine and from December 15th, 2006, consolidation therapy was conducted along with idarubicin and high dose of cytarabine. Subsequently, allogenic peripheral blood stem cells were transplanted on February 8th, 2007. From 21st day after the transplantation, there was occurrence of skin rashes on her entire body and diarrhea, thus skin biopsy and colonoscopy were conducted. Based on the examinations, occurrence of acute graft-versus-host disease was confirmed. FK506 (tacrolimus) was administered from one day before the transplantation and high-dose steroid therapy was conducted from one day after the expression of the acute graft-versus-host disease. At a later stage, the dose of prednisolone was reduced and the dose of prednisolone was maintained at 10 mg per day. Complete remission was shown in a bone marrow biopsy conducted three months after the transplantation. Four months after the transplantation, skin rashes and dyspnea occurred and the expression of chronic graft-versus-host disease was identified through skin biopsy. Thereafter, she had been using 8 mg of FK506 and 2.5 mg of prednisolone per day until her next visit to this department.
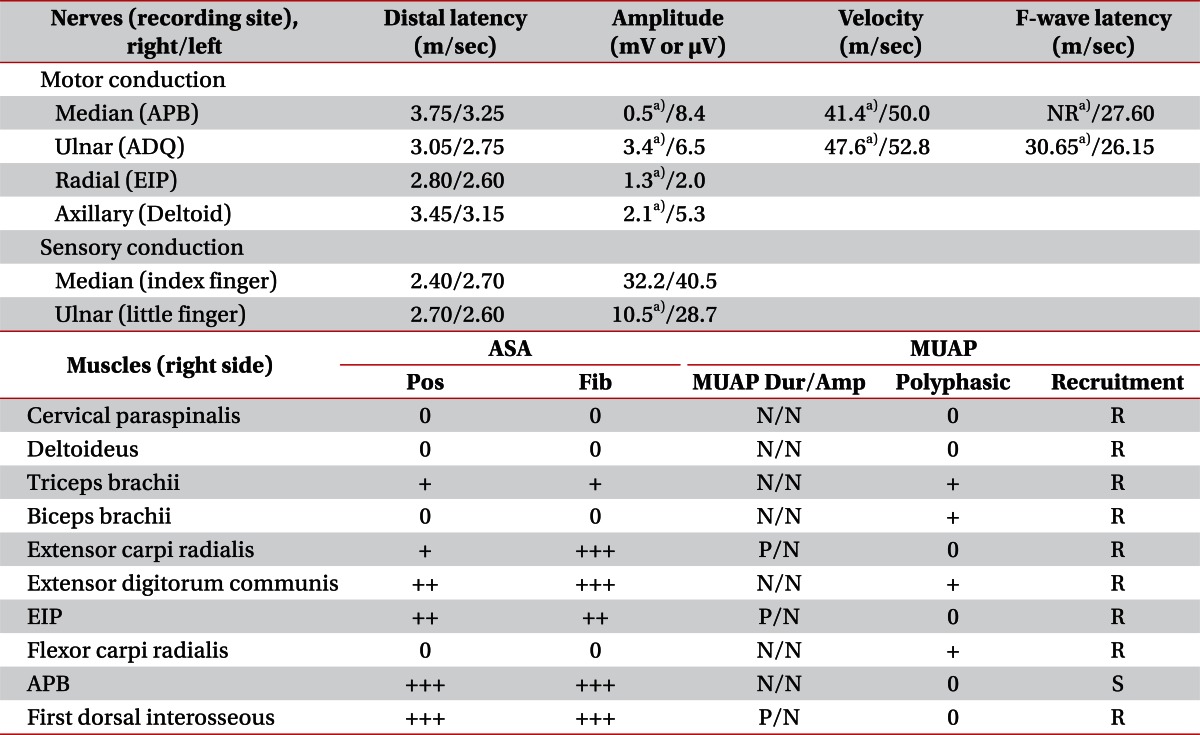
During her next visit to this department, in manual muscle test conducted as a part of physical examinations, the strength of the right shoulder joint and elbow joint muscles was 4/5-5/5, the strength of the right finger flexor and abductor was 1/5-2/5 and the opposition between the thumb and the little finger of the right hand was impossible. In visual inspection, muscular atrophy was observed in the right abductor pollicis brevis muscle. In sensory evaluations, reduced light touch and pain sensation were identified in the 8th cervical dermatome and the 1st thoracic dermatome. Both of the biceps and triceps tendon reflexes were normal and the degree of pain in the right shoulder and upper extremity was five points in the visual analogue scale (0 point, no pain; 10 points, maximal pain). In electrophysiologic study, findings of right brachial plexopathy that mainly involved the medial cord and posterior cord of the right brachial plexus were observed (Table 1). In magnetic resonance imaging conducted based on the results of the electrophysiologic study, diffuse high signal intensity lesions in an area ranging from the trunk level to the cord level of the right brachial plexus were observed in short tau inversion recovery (STIR) and mild swelling of brachial plexus was also observed. However, the nerve plexus did not show any mass lesions and no mass external to the nerve plexus that pressed the nerve plexus was observed. In enhanced T1 images, findings of contrast enhancement of the nerve plexus in the region appeared (Fig. 1). In addition, there was appearance of no mass lesions internal or external to the brachial plexus. Considering the fact that the expression of the symptoms is relatively sudden, steroid pulse therapy was conducted under the impression of brachial plexus neuritis. Methylprednisolone 1,000 mg was intravenously injected on the first day and methylprednisolone 500 mg was intravenously injected for two days thereafter. From the 4th day, prednisolone 40 mg was orally administered per day for one week and the dose was decreased by 10 mg per week. In a follow-up observation on the 7th day after the steroid therapy, the pain in the right upper extremity was relieved to visual analogue scale 1, the pain that had been induced by upper extremity movements disappeared and the hypesthesia in the medial surface of the right upper extremity was recovered. At this time point, the muscle strength of the finger abductor in manual muscle test was improved to 3/5 and the patient reported that she felt convenient in using the chopsticks. Thereafter, the patient was followed up until the end of April 2008 without any change in neurological findings. In April 2008, symptoms of the chronic acute graft-versus-host disease were aggravated such as the occurrence of pantothermia (38.5° or higher) and shortness of breath and thus the patient was re-admitted into the department of oncology. Three weeks after the hospitalization, pain in the left flank occurred and thus abdominal and pelvic computed tomography was conducted. In the computed tomography, gastric submucosal thickening, soft tissue lesions in the omentum, perihepatic space, and hydronephrosis were observed. In gastric and duodenal biopsies conducted under upper gastrointestinal endoscopy, negative findings of CD3, CD15, CD20, and CD117 (C-kit) and positive findings of CD13, CD56, lysozyme, leukocyte common antigen (LCA) and myeloperoxidase were observed in-immunohistochemical staining and thus myeloid sarcoma was pathologically diagnosed. In 18-fluoride fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) conducted at 6 months after the expression of brachial plexus symptoms during the hospitalization, high metabolism lesions judged to be myeloid sarcoma were identified in many organs including the brachial plexus, the stomach, the omentum, perihepatic space, the mediastinum, the right breast and the chest wall (Fig. 2). In PET/CT images, an egg shaped mass lesion with increased 18F-FDG uptake was observed in the cord level of the right brachial plexus and the maximum standardized uptake value (SUVmax) of the lesion was 3.7. This lesion was at the same location as the lesion that showed high signal intensity in the earlier magnetic resonance imaging of the brachial plexus. Under the diagnosis of myeloid sarcoma, re-induction therapy was conducted with amsacrine and high-dose of cytarabine, but the patient died two months after the beginning of treatment.
The incidence rate of myeloid sarcoma in acute myelogenous leukemia patients is reported as 3%-5% [3], and myeloid sarcoma can occur in any age (median age, 36 years; range, 0.5 to 89 years) regardless of sex. In addition to acute myelogenous leukemia patients, myeloid sarcoma can rarely appear as a complication in patients with chronic myelogenous leukemia, myelodysplastic syndrome or myeloproliferative disorders [1,3]. Cases demonstrating the occurrence of myeloid sarcoma in peripheral nerve system are rare and three cases where myeloid sarcoma has occurred in the brachial plexus have been reported [4-6]. When the present case is compared with other cases where myeloid sarcoma invaded the brachial plexus, the fact that allogenic peripheral blood stem cells were transplanted before the occurrence of symptoms and the fact that myeloid sarcoma occurred in many organs within a short time after the occurrence of myeloid sarcoma in the brachial plexus are characteristics of this case. As risk factors for the occurrence of myeloid sarcoma, AML-M4, AML-M5, CD56 positive blasts, 8:21 gene translocation, 16 gene inversion, impaired cellular immunity and allogenic stem cell transplantation are known to be closely associated with a higher incidence of myeloid sarcoma [3]. This case was too AML-M5 and allogenic peripheral blood stem cells were transplanted before the occurrence of myeloid sarcoma.
The occurrence of myeloid sarcoma is considered as an early herald of a systemic relapse because AML frequently recurs quickly after the expression of myeloid sarcoma, even though complete remission has been accomplished [2,3,7]. Myeloid sarcoma shows diffuse enlargement and signal intensity similar to that of the bone marrow in magnetic resonance imaging and shows fusiform shaped enhancement in gadolinium enhanced images [6,8,9]. However, in the present case, no mass lesion was observed in magnetic resonance imaging and although a biopsy of the brachial plexus was requested, the biopsy was not conducted due to the possibility of occurrence of muscle weakness and paresthesia that may occur in biopsies. Therefore, myeloid sarcoma could not be diagnosed until PET/CT and gastrointestinal biopsy were carried out.
As imaging techniques to diagnose myeloid sarcoma, 18F-FDG PET/CT images are reported to be useful and in the case of myeloid sarcoma of other organs, SUVmax has been demonstrated to be between 2.1 to 9.3 [10]. In case if focal neuropathy or plexopathy is suspected in a myelogenous leukemia patient, and in particular, if the patient has risk factors for myeloid sarcoma, it is important to suspect myeloid sarcoma and for early diagnoses, PET/CT images or biopsies are considered to be useful.
In conclusion, we report a case where brachial plexopathy was diagnosed due to myeloid sarcoma, although not pathologically diagnosed. This was possible since myeloid sarcoma was pathologically diagnosed definitely in other organs and the lesion progressed into a mass lesion in the brachial plexus in follow-up PET/CT images.
References
1. Campidelli C, Agostinelli C, Stitson R, Pileri SA. Myeloid sarcoma: extramedullary manifestation of myeloid disorders. Am J Clin Pathol. 2009; 132:426–437. PMID: 19687319.
2. Byrd JC, Edenfield WJ, Shields DJ, Dawson NA. Extramedullary myeloid cell tumors in acute nonlymphocytic leukemia: a clinical review. J Clin Oncol. 1995; 13:1800–1816. PMID: 7602369.

3. Paydas S, Zorludemir S, Ergin M. Granulocytic sarcoma: 32 cases and review of the literature. Leuk Lymphoma. 2006; 47:2527–2541. PMID: 17169797.

4. Bakst R, Jakubowski A, Yahalom J. Recurrent neurotropic chloroma: report of a case and review of the literature. Adv Hematol. 2011; 2011:85240.

5. Karam C, Khorsandi A, MacGowan DJ. Clinical reasoning: a 23-year-old woman with paresthesias and weakness. Neurology. 2009; 72:e5–e10. PMID: 19139360.

6. Mauermann ML, Angius D, Spinner RJ, Letendre LJ, Amrami KK, Dyck PJ. Isolated granulocytic sarcoma presenting as a brachial plexopathy. J Peripher Nerv Syst. 2008; 13:153–156. PMID: 18601661.
7. Byrd JC, Weiss RB. Recurrent granulocytic sarcoma: an unusual variation of acute myelogenous leukemia associated with 8;21 chromosomal translocation and blast expression of the neural cell adhesion molecule. Cancer. 1994; 73:2107–2112. PMID: 7512442.

8. Lekos A, Katirji MB, Cohen ML, Weisman R Jr, Harik SI. Mononeuritis multiplex: a harbinger of acute leukemia in relapse. Arch Neurol. 1994; 51:618–622. PMID: 8198473.
9. Pui MH, Fletcher BD, Langston JW. Granulocytic sarcoma in childhood leukemia: imaging features. Radiology. 1994; 190:698–702. PMID: 8115614.

10. Stolzel F, Rollig C, Radke J, Mohr B, Platzbecker U, Bornhauser M, et al. 18F-FDG-PET/CT for detection of extramedullary acute myeloid leukemia. Haematologica. 2011; 96:1552–1556. PMID: 21685468.

Fig. 1
Magnetic resonance images (coronal, short tau inversion recovery image) from ventral (A) towards dorsal (D) surfaces of the brachial plexus shows diffuse high signal intensity and mild swelling of the right brachial plexus (arrow) from trunk level to cord level. No definite mass lesion was noted within or outside the brachial plexus.
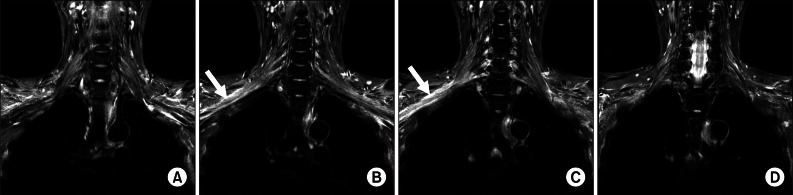
Fig. 2
18-Fluoride fluorodeoxyglucose positron emission tomography (PET) findings. Three-dimensional projection image (A, B) PET/computed tomography fusion axial image (C) reveal hot uptake in stomach, transverse colon, right perihepatic space, right cardiophrenic angle, anterior mediastinum and right brachial plexus. Fusiform shaped mass lesions can be seen at the cord level of right brachial plexus (black and white arrow).

Table 1
Findings of electrophysiologic study
APB, abductor pollicis brevis; NR, no response; ADQ, abductor digiti quinti; EIP, extensor indicis proprius; ASA, abnormal spontaneous activity; MUAP, motor unit action potentials; Pos, positive sharp wave; Fib, fibrillation potentials; Dur/Amp, duration/amplitude; N, normal; P, prolonged duration; R, reduced MUAP recruitment; S, single MUAP recruitment.
a)Abnormal finding based on reference value of our laboratory.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download