INTRODUCTION
Carpal tunnel syndrome (CTS) is a neuropathy caused by entrapment of the median nerve at the wrist, which leads to pain, hypesthesia at the dermatome area and weakness of the abductor pollicis brevis (APB) muscle [
1]. It is the most common peripheral neuropathy and Atroshi et al. [
2] reported that it occurs in 5.8% of women and 0.6% of men.
Diagnosis of CTS is made with clinical symptoms, physical examination and electrodiagnostic study, of which, electrodiagnostic study is known to be the most accurate and useful method of diagnosis [
3,
4]. However, a variety of study methods exist to increase the sensitivity, and every physician has his own preferred method. Measuring the differences in peak, onset latency and baseline to peak amplitude between stimulation at the wrist, where a 14 cm proximal to the recording electrode and at the palm, 7 cm proximal to the electrode, and comparing latencies with ulnar and radial sensory nerve are the general methods recommended by the American Association of Neuromuscular Electrodiagnostic Medicine [
5,
6]. In most cases, the 2nd or 3rd finger is used for recording electrodes in a median nerve sensory conduction study [
3,
5]. However, the debate in which the finger is most sensitive for the diagnosis of CTS is still ongoing [
7-
9].
Sheean et al. [
6] reported that the onset latency of median motor conduction studies recorded on APB is less sensitive than other electrodiagnostic parameters in CTS diagnosis, and that it would be useful to compare the onset latencies of compound muscle action potentials (CMAP) of the median innervated lumbrical muscles and ulnar innervated interosseous muscles in the palm. Boonyapisit et al. [
10] also reported that for a moderate degree of CTS, it is helpful to use a lumbrical recording for localization of the lesion and differential diagnosis from other conditions, such as polyneuropathy, when action potential is not evoked due to atrophy of APB.
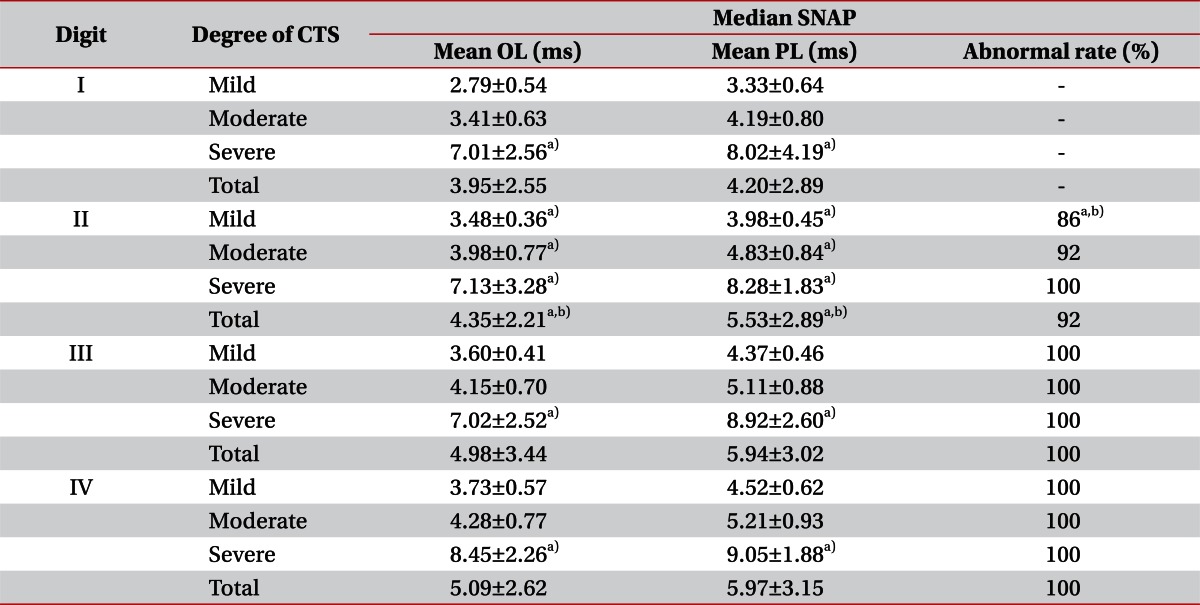
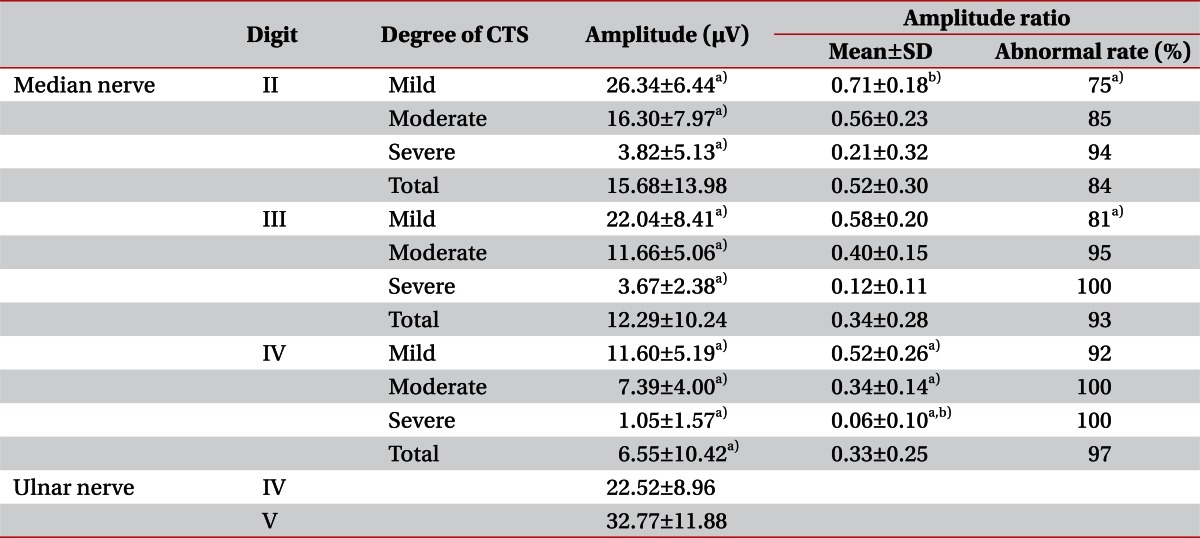
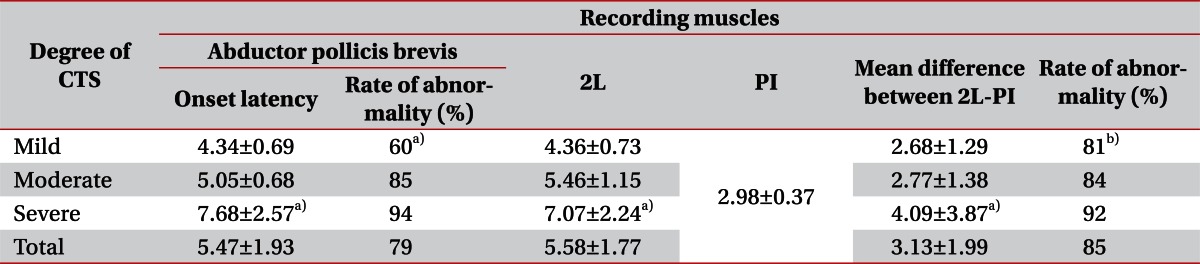
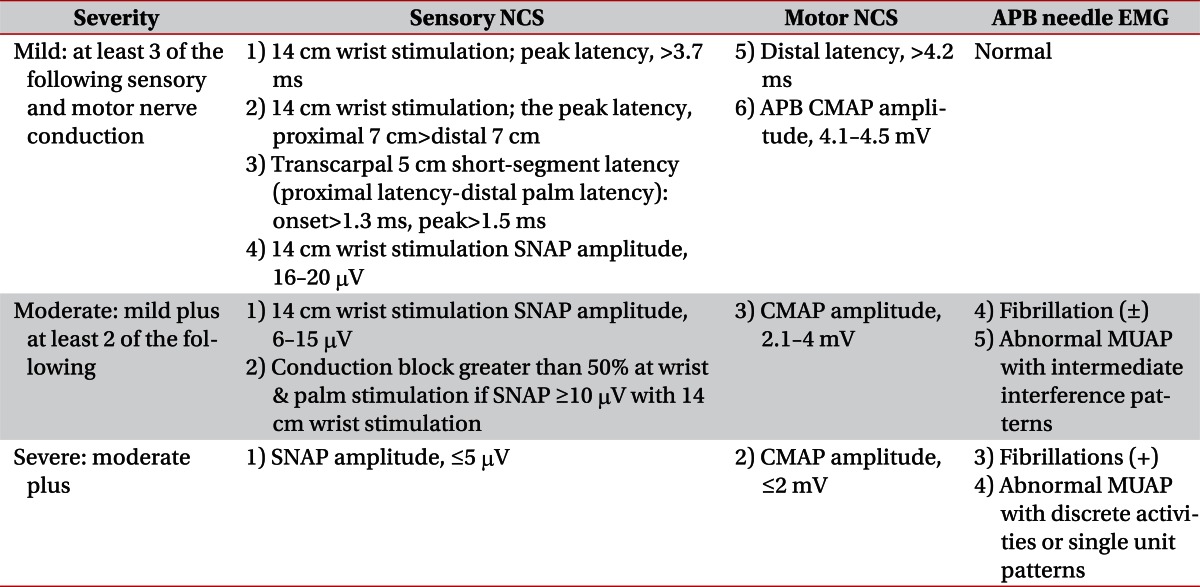
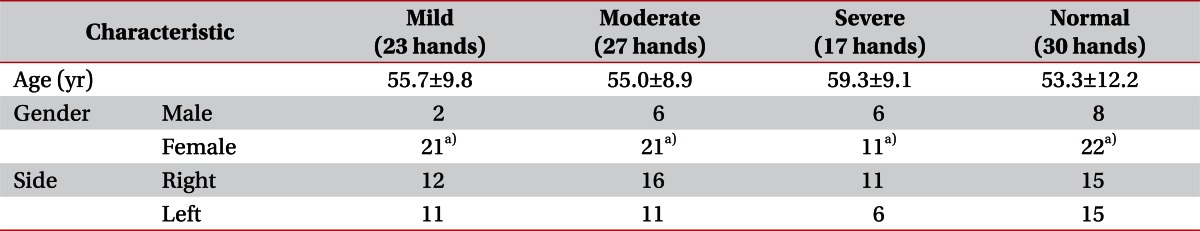
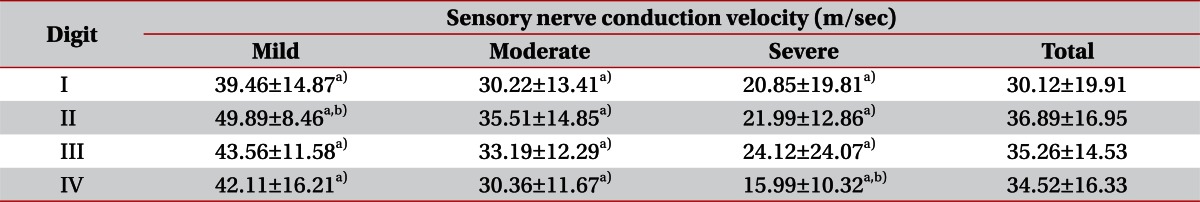
In this study, we evaluated the median sensory nerve action potentials (SNAP) from each digit and CMAP onset latency differences between the 2nd lumbrical muscle and interosseous muscle for each CTS severity to observe the involvement of median sensory and motor nerve branches, according to disease progression.
Go to :

DISCUSSION
An electrodiagnostic study is used as an objective and accurate tool in diagnosing CTS; the sensory conduction study is known to be more sensitive than the motor conduction study in the early stage of the disease [
7,
15]. However, various studies reported controversial results, regarding which digit should be tested in order to increase the sensitivity and accuracy of the test. Aydin et al. [
7] performed studies in comparing the median nerve conduction velocities of the 1st, 2nd, 3rd, and 4th digits on 818 hands of 525 CTS patients. This study reports that the 1st digit showed the highest frequency of decreased conduction velocity and that the 2nd digit conduction velocity was relatively preserved. A study by Tsaiweichao-Shozawa et al. [
15] states that the sensory branch of the median nerve to the 2nd digit and motor branch to the lumbrical muscle is relatively preserved in the late course of the disease. In the study performed with 55 CTS patients, Macdonell et al. [
16] reported that the decrease in median conduction velocity was most prominent with the 1st digit and was less frequent with the 2nd digit. However, Padua et al. [
17] reported that there are significant decreases in conduction velocity at the 1st and 3rd digits without a significant difference between the two digits. Lauritzen et al. [
18] also reported that there is no difference in the sensitivity of the test between the 1st and 3rd digit in a mild degree CTS. In a study by Terzis et al. [
8] with 72 patients with mild degree CTS whose onset latency was shorter than 4.2 ms with APB recording, reported that the sensitivity of conduction studies on the 1st, 2nd, 3rd, and 4th digits were be 61%, 22%, 50%, and 88%, respectively-the 4th digit being the most useful in CTS diagnosis. Cioni et al. [
19] compared the frequency of lowered conduction velocities between the digits, in a group of patients with clinical symptoms of CTS, where the frequencies were 64%, 80%, and 92% in the 1st, 2nd, and 3rd digits, respectively. Conduction velocity was lowered in all of the patients in the 4th digit.
In this study, comparisons of each digit according to the disease severity showed significant differences in the 2nd digit compared to the 1st, 3rd, and 4th digits for the mild, moderate, and severe groups. It seems that such a difference is due to the well preserved sensory branch to the 2nd digit in the mild degree group, which showed a difference even with the moderate group. Frequency of latency prolongation was significantly lower with the 2nd digit and SNAP amplitude ratio was also significantly higher compared to the 3rd and 4th digits. Frequency of abnormal values was also lower compared to the control group, though without statistical significance. The fact that among the 8 hands whose SNAPs were not evoked with the 1st, 3rd, and 4th digits, the fact that 2 showed preserved SNAPs with the 2nd digit also supports these results. By contrast, the amplitude ratio was significantly low with the 4th digit, and the frequency of abnormal value was higher compared to the other digits in all the severities without statistical significance. An evaluation on the conduction velocity showed similar results. In the mild degree group, conduction velocity was relatively preserved with the 2nd digit, and in the severe group, it was significantly decreased with the 4th digit. In comparison of the conduction velocities despite the severity degree, it was decreased with the 1st digit, compared to the other digits.
Considering all the results from this study, it can be said that in the early stage of CTS, the 2nd digit is preserved. Differences in the degree of impairment between the digits according to the disease progression can be explained by fascicular arrangement of the median nerve under carpal tunnel [
16,
20]. In CTS, the median nerve injury occurs most severely at the distal end of carpal tunnel, just proximal to which the motor and sensory branches divide. In carpal tunnel, the median sensory branches to the 1st and 3rd digits lie in the antero-lateral side, branches to the 4th digit lie in the antero-medial side, and to the 2nd digit lie in the postero-medial side. Due to such a fascicular arrangement, sensory branches to the 2nd digit, located in the posterior side, are less vulnerable to injury compared to other digits. Moreover, conduction study values are more preserved in the early stage, when compression or ischemia occurs in the carpal tunnel [
7].
Despite the fact that the 4th digit is severely affected by the disease progression, in clinical practice, physicians prefer to use the 2nd and 3rd digits over the 4th digit in median sensory conduction studies, due to small SNAPs caused by dual innervation of the median and ulnar nerve. However, considering the fact that the sensitivity of the 2nd digit in CTS diagnosis is not high [
7,
15,
16], and a study by Padua et al. [
17] reported that the distal-proximal distance ratios of the elbow and hand according to the course of the median nerves is most ideal in the 2nd and 3rd digits, it is most appropriate to use the 3rd digit for the active recording electrode in CTS diagnosis. In this study, diagnostic criteria for the peak latency was set to 3.7 ms for the 2nd, 3rd, and 4th digits considering the same distance applied between the electrode and the stimulator. Considering different degrees of disease involvement in each digit, according to the disease progression, applying the same criteria can be a limitation of this study.
We also performed evaluations on the median motor conduction study. Among the median motor branches, the recurrent branch to the APB muscle is in a position to be more vulnerable to carpal tunnel compression than branches to the 1st and 2nd lumbrical muscles. Sunderland [
21] discovered that branch to the lumbrical muscle is positioned postero-medially to the APB branch at 37 mm distal to the radial styloid process of the wrist, and at the 20 mm distal point, it is positioned relatively anterior compared to the distal part, yet still posterior to the APB branch. They also reported that the sensory branch to the 2nd digit is positioned relatively posterior to the lumbrical muscle motor branches. Tsaiweichao-Shozawa et al. [
15] reported that due to such arrangements of nerve fascicles, branches to the 2nd digit and lumbrical muscle are relatively more preserved in carpal tunnel compression, and that a correlation exists between the conduction study values of the two branches. Therefore, various studies exist on the clinical usefulness of lumbrical muscle recording for CTS diagnosis. Sheean et al. [
6] claimed that though using lumbrical muscle may not increase the sensitivity of electrodiagnostic study, measuring lumbrical-interosseous muscle latency differences can be useful. Boonyapisit et al. [
10] reported that in moderate degree CTS, a lumbrical muscle recording conduction study is useful in the dfferential and accurate diagnoses.
In this study, latency prolongation with APB muscle recording was significantly lower in frequency than lumbrical-interosseous latency differences in the mild degree group, which is similar to a previous study by Sheean et al. [
6] The reason for such result is that in the early process of CTS, demyelination is the main pathology of the disease, so when the damage is minimal, latency may appear within normal range. However, compared to the latency of the ulnar nerve, which does not pass through the carpal tunnel, latencies of the median nerve is relatively prolonged and the latency difference can be significant, which makes lumbrical-interosseous latency differences more sensitive than the latency recorded from the APB muscle. As the disease progresses, the pathophysiology of the disease changes and due to its anatomically favorable position, the branch to the lumbrical muscle is less affected by the conduction block or axonal injury, and is relatively preserved in the conduction study. In this study, from the 4 digits with unevoked APB recorded CMAPs, and from the 8 digits with unevoked SNAPs, lumbrical muscle recording CMAPs were all obtained. These results show that the lumbrical-interosseous latency difference is a tool for increasing sensitivity in CTS diagnosis, and consistent with previous studies, as the disease progress, lumbrical muscle is relatively preserved in severe degree CTS.
In conclusion, this study shows that the 4th digit SNAP is the most severely affected in CTS, but the 2nd digit SNAP is relatively spared, and that lumbrical recorded median CMAP is spared in the severe degree CTS group. Considering its sensitivity and specificity, the 3rd digit is commonly used in clinical practice for electrodiagnostic study in CTS. However, in severe patients, using the SNAP recorded on the 2nd digit or the CMAP recorded on the lumbrical muscle, which are relatively spared even in the late stage of the disease, may help in diagnosing CTS.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download