1. Bernstein J, Lane JM. Rothman RH, Siemone FA, editors. Metabolic disorders of the spine. The spine. 1992. 3rd ed. Philadelphia: WB Saunders;p. 1393–1394.
2. Rapado A. General management of vertebral fractures. Bone. 1996; 18(3 Suppl):191S–196S. PMID:
8777087.

3. Watts NB, Harris ST, Genant HK. Treatment of painful osteoporotic vertebral fractures with percutaneous vertebroplasty or kyphoplasty. Osteoporos Int. 2001; 12:429–437. PMID:
11446557.

4. Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976). 2001; 26:1511–1515. PMID:
11462078.
5. Mitra R, Do H, Alamin T, Cheng I. Facet pain in thoracic compression fractures. Pain Med. 2010; 11:1674–1677. PMID:
21029349.

6. Georgy BA. Interventional techniques in managing persistent pain after vertebral augmentation procedures: a retrospective evaluation. Pain Physician. 2007; 10:673–676. PMID:
17876364.
7. Bogduk N. Evidence-informed management of chronic low back pain with facet injections and radiofrequency neurotomy. Spine J. 2008; 8:56–64. PMID:
18164454.

8. Bogduk N. Practice guidelines for spinal diagnostic and treatment procedures. 2004. 1st ed. San Francisco: International Spinal Intervention Society;p. 47–65.
9. Bogduk N, Wilson AS, Tynan W. The human lumbar dorsal rami. J Anat. 1982; 134(Pt 2):383–397. PMID:
7076562.
10. Bogduk N. The innervation of the lumbar spine. Spine (Phila Pa 1976). 1983; 8:286–293. PMID:
6226119.

11. Boswell MV, Shah RV, Everett CR, Sehgal N, McKenzie Brown AM, Abdi S, et al. Interventional techniques in the management of chronic spinal pain: evidence-based practice guidelines. Pain Physician. 2005; 8:1–47. PMID:
16850041.
12. Manchikanti L, Staats PS, Singh V, Schultz DM, Vilims BD, Jasper JF, et al. Evidence-based practice guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2003; 6:3–81. PMID:
16878163.
13. Manchikanti L, Manchikanti KN, Manchukonda R, Pampati V, Cash KA. Evaluation of therapeutic thoracic medial branch block effectiveness in chronic thoracic pain: a prospective outcome study with minimum 1-year follow up. Pain Physician. 2006; 9:97–105. PMID:
16703969.
14. Kim KT, Lee SH, Suk KS, Lee JH, Im YS, Seo EM. Loss of sagittal balance and clinical outcomes following corrective osteotomy for lumbar degenerative kyphosis. J Korean Orthop Assoc. 2009; 44:83–92.

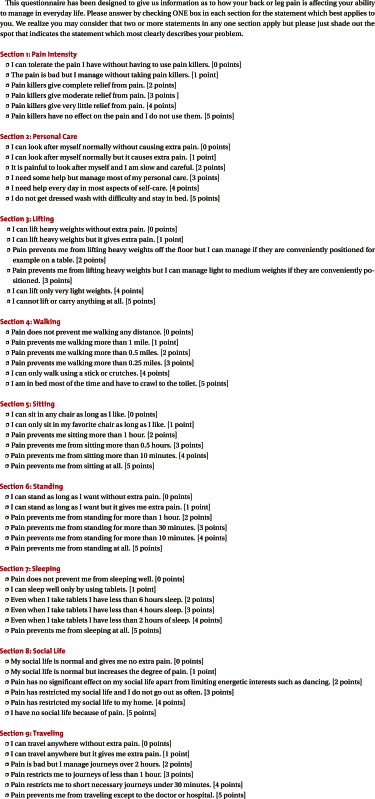
15. Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980; 66:271–273. PMID:
6450426.
16. Lee IS, Kim SH, Lee JW, Hong SH, Choi JY, Kang HS, et al. Comparison of the temporary diagnostic relief of transforaminal epidural steroid injection approaches: conventional versus posterolateral technique. AJNR Am J Neuroradiol. 2007; 28:204–208. PMID:
17296980.
17. Ng L, Chaudhary N, Sell P. The efficacy of corticosteroids in periradicular infiltration for chronic radicular pain: a randomized, double-blind, controlled trial. Spine (Phila Pa 1976). 2005; 30:857–862. PMID:
15834326.
18. Campbell WI, Kendrick RW. Pre-emptive analgesia using local anaesthesia: a study in bilaterally symmetrical surgery. Br J Anaesth. 1997; 79:657–659. PMID:
9422907.

19. Nam HS, Park YB. Effects of transforaminal injection for degenerative lumbar scoliosis combined with spinal stenosis. Ann Rehabil Med. 2011; 35:514–523. PMID:
22506167.

20. Ledlie JT, Renfro M. Balloon kyphoplasty: one-year outcomes in vertebral body height restoration, chronic pain, and activity levels. J Neurosurg. 2003; 98(1 Suppl):36–42. PMID:
12546386.

21. Beaman DN, Graziano GP, Glover RA, Wojtys EM, Chang V. Substance P innervation of lumbar spine facet joints. Spine (Phila Pa 1976). 1993; 18:1044–1049. PMID:
7690159.

22. Kim TK, Kim KH, Kim CH, Shin SW, Kwon JY, Kim HK, et al. Percutaneous vertebroplasty and facet joint block. J Korean Med Sci. 2005; 20:1023–1028. PMID:
16361816.

23. Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Lumbar facet joint nerve blocks in managing chronic facet joint pain: one-year follow-up of a randomized, double-blind controlled trial: Clinical Trial NCT00355914. Pain Physician. 2008; 11:121–132. PMID:
18354721.
24. Lee HM, Weinstein JN, Meller ST, Hayashi N, Spratt KF, Gebhart GF. The role of steroids and their effects on phospholipase A2: an animal model of radiculopathy. Spine (Phila Pa 1976). 1998; 23:1191–1196. PMID:
9636970.
25. Johansson A, Hao J, Sjolund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand. 1990; 34:335–338. PMID:
2167604.

26. Arner S, Lindblom U, Meyerson BA, Molander C. Prolonged relief of neuralgia after regional anesthetic blocks: a call for further experimental and systematic clinical studies. Pain. 1990; 43:287–297. PMID:
1705693.

27. Benzon HT. Epidural steroid injections for low back pain and lumbosacral radiculopathy. Pain. 1986; 24:277–295. PMID:
3008063.

28. Lavoie PA, Khazen T, Filion PR. Mechanisms of the inhibition of fast axonal transport by local anesthetics. Neuropharmacology. 1989; 28:175–181. PMID:
2469989.

29. Katz WA, Rothenberg R. Section 3: The nature of pain: pathophysiology. J Clin Rheumatol. 2005; 11(2 Suppl):S11–S15. PMID:
16357723.
30. Cassuto J, Sinclair R, Bonderovic M. Anti-inflammatory properties of local anesthetics and their present and potential clinical implications. Acta Anaesthesiol Scand. 2006; 50:265–282. PMID:
16480459.

31. Weinstein JN, Collalto P, Lehmann TR. Thoracolumbar "burst" fractures treated conservatively: a long-term follow-up. Spine (Phila Pa 1976). 1988; 13:33–38. PMID:
3381135.

32. Willen J, Lindahl S, Nordwall A. Unstable thoracolumbar fractures: a comparative clinical study of conservative treatment and Harrington instrumentation. Spine (Phila Pa 1976). 1985; 10:111–122. PMID:
4002035.
33. Reid DC, Hu R, Davis LA, Saboe LA. The nonoperative treatment of burst fractures of the thoracolumbar junction. J Trauma. 1988; 28:1188–1194. PMID:
3411642.

34. Day B, Kokan P. Compression fractures of the thoracic and lumbar spine from compensable injuries. Clin Orthop Relat Res. 1977; (124):173–176. PMID:
598072.

35. Aglietti P, Di Muria GV, Taylor TK, Ruff SJ, Marcucci M, Novembri A, et al. Conservative treatment of thoracic and lumbar vertebral fractures. Ital J Orthop Traumatol. 1983; 9(Suppl):83–105. PMID:
6679850.
36. Shin BJ, Kim SK, Lee BI, Kim YI, Rah SK, Choi CU. Posterior column injuries in thoracolumbar and lumbar burst fractures. J Korean Soc Spine Surg. 1997; 4:67–73.
37. Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The false-positive rate of uncontrolled diagnostic blocks of the lumbar zygapophysial joints. Pain. 1994; 58:195–200. PMID:
7816487.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download