This article has been
cited by other articles in ScienceCentral.
Abstract
Blind intramuscular injection might cause severe neurovascular injury if it would be performed with insufficient knowledge of anatomy around the injection area. We report a case of pseudo-anterior interosseous syndrome caused by multiple intramuscular steroid injections around the antecubital area. The patient had weakness of the 1st to 3rd digits flexion with typical OK sign. Muscle atrophy was noted on the proximal medial forearm, and sensation was intact. The electrophysiologic studies showed anterior interosseous nerve compromise, accompanying with injury of the other muscles innervated by the median nerve proximal to anterior interosseous nerve. Magnetic resonance imaging of the left proximal forearm revealed abnormally increased signal intensity of the pronator teres, flexor carpi radialis, proximal portion of flexor digitorum superficialis, and flexor digitorum profundus innervated by the median nerve on the T2-weighted images. This case shows the importance of knowledge about anatomic structures in considering intramuscular injection.
Go to :

Keywords: Pseudo-anterior interosseous nerve syndrome, Intramuscular injections
INTRODUCTION
Pseudo-anterior interosseous nerve syndrome (pseudo-AINS) is often mistaken as the paralysis of the anterior interosseous nerve (AIN) lesion, but it actually has a lesion in the proximal median nerve before the AIN branch arises. Clinically, the paralysis of the muscles innervated by the AIN is accompanied with some involvement of the other muscles innervated by the proximal median nerve, with or without sensory symptoms [
1].
We report a case of pseudo-AINS, following multiple intramuscular injections around the antecubital area. It shows that the injuries can be developed during injection using the blind technique without accurate knowledge of anatomic structure.
Go to :

CASE REPORT
A 37-year-old healthy man was presented with a two-week history of weakness of the left 1st to 3rd digits flexion. Prior to the symptoms, he had visited a local orthopedic clinic with sharp pain in the left medial forearm area and had received multiple intramuscular steroid injections around the left proximal medial forearm. The pain was alleviated after injections, but the patient noted flexion weakness of the left 1st to 3rd digits. There was no numbness or tingling sensation. He had no history of systemic symptoms, including fever, weight loss or bowel and bladder symptoms.
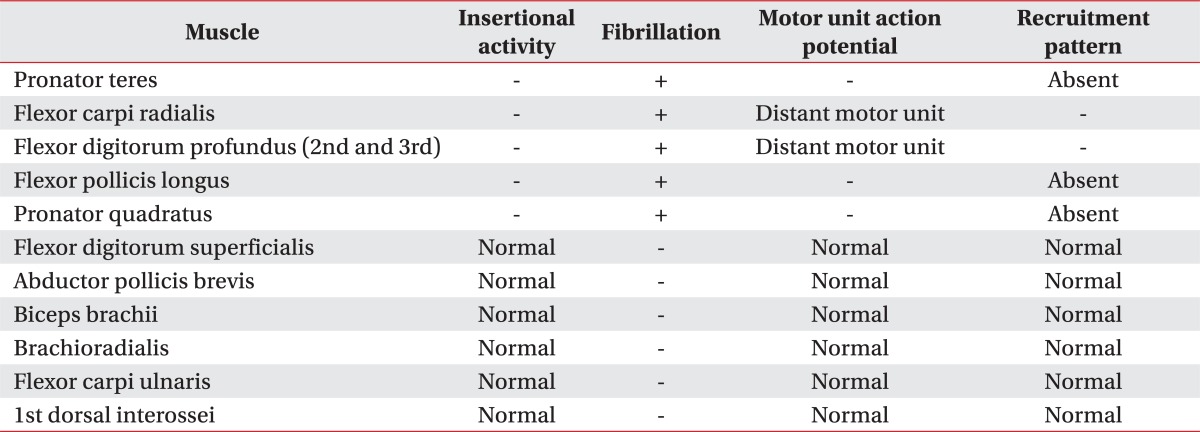
Muscle strength was measured using the Medical Research Council (MRC) scale. It was MRC grade 0 to1 in flexors of the interphalangeal joint of the left thumb, MRC grade 2 in the flexors of the distal phalanx of the left index and middle finger, MRC grade 0 to 1 in the forearm pronators, and MRC grade 4 in the left elbow and wrist flexors. However, the other muscles of the left upper extremity had normal strength. There was muscle atrophy prominent on the left proximal medial forearm, compared to that of the right side. Typical "OK" sign was present (
Fig. 1). Deep tendon reflexes of the bilateral upper extremities were within normal limits. There was no sensory abnormality. The plane radiographs of the cervical spine and left elbow showed normal findings. Also, the ultrasound of the elbow showed no abnormality. Therefore, we excluded the possibility of the cervical root lesion or elbow joint pathology.
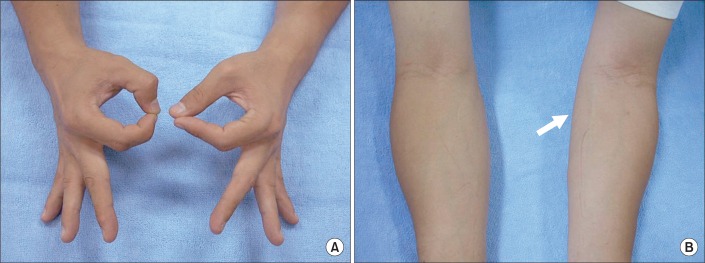 | Fig. 1OK sign was present in the left hand (A) and muscle atrophy (arrow) was observed in the medial side of the proximal forearm (B). 
|
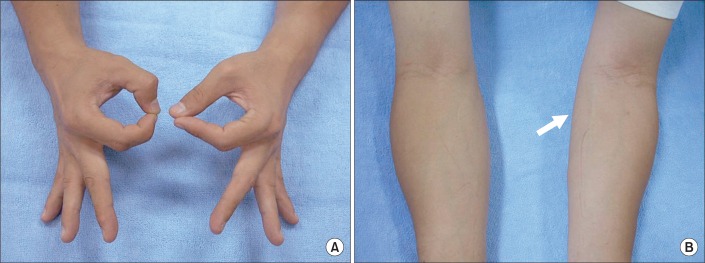
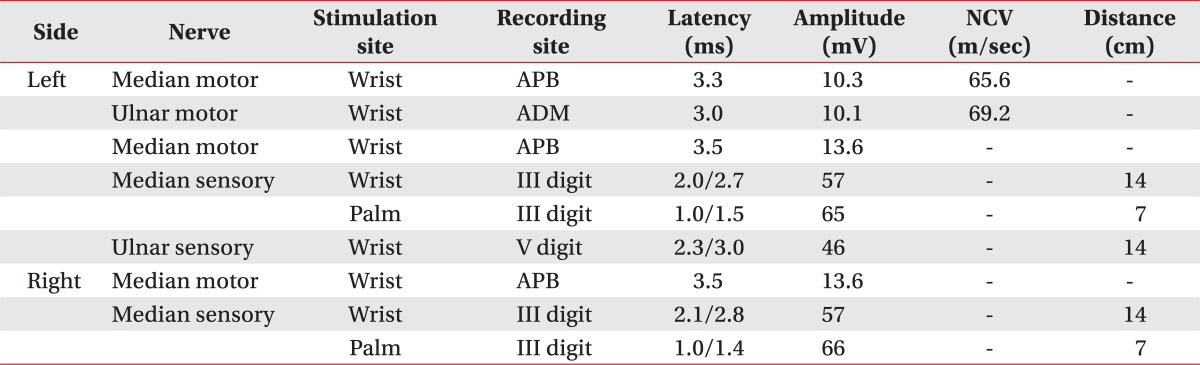
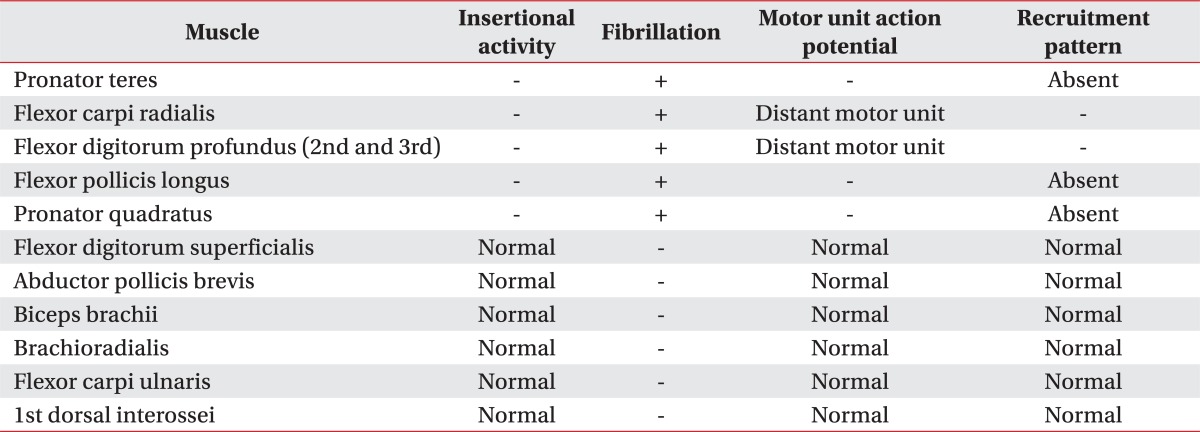
Electrodiagnostic studies were performed. Motor and sensory nerve conduction studies of the median and ulnar nerves were normal (
Table 1). Needle electromyographic examination revealed abnormal spontaneous activities and no motor unit or distant motor unit potentials in the left pronator teres, flexor carpi radialis, flexor digitorum profundus to 2nd and 3rd digits, flexor pollicis longus, and pronator quadratus muscles. The other muscles, including flexor digitorum superficialis and abductor pollicis brevis, were normal (
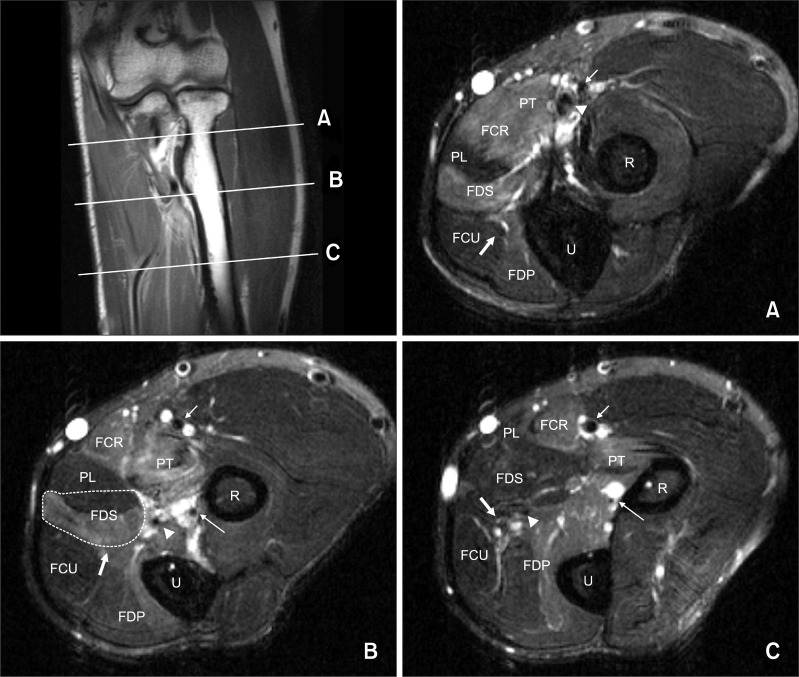
Table 2). T2-weighted magnetic resonance imaging (MRI) study of the left proximal forearm showed abnormally increased signal intensity in the pronator teres, flexor carpi radialis, proximal portion of flexor digitorum superficialis, and flexor digitorum profundus innervated by the median nerve. Palmaris longus was spared (
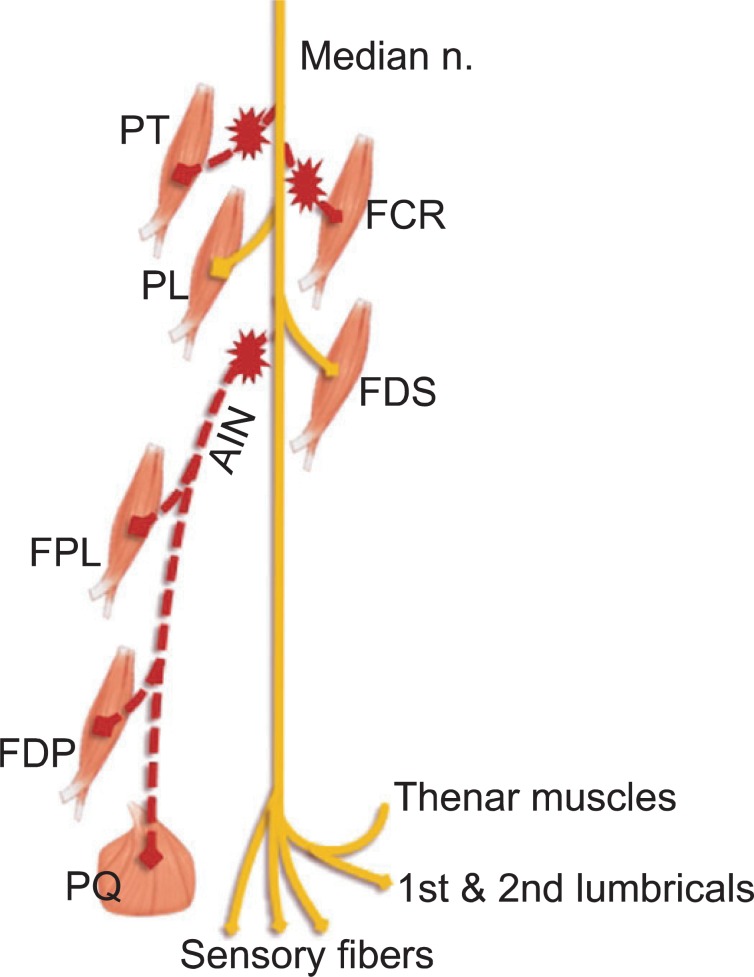
Fig. 2). We supposed that the patient's symptom was the result of the injury of AIN branch, accompanied by the muscular branch injury of the proximal median nerve in multiple sites on the antecubital area (
Fig. 3). We cannot exclude the possibility of partial injury of the proximal median nerve, which causes damage to the specific fascicular component. These conditions can be considered as pseudo-AINS. During 2 months, He take thiotic acid and got a physical therapy, including electrical stimulation. However, there was no significant improvement in muscle strength and the patient stopped the treatment.
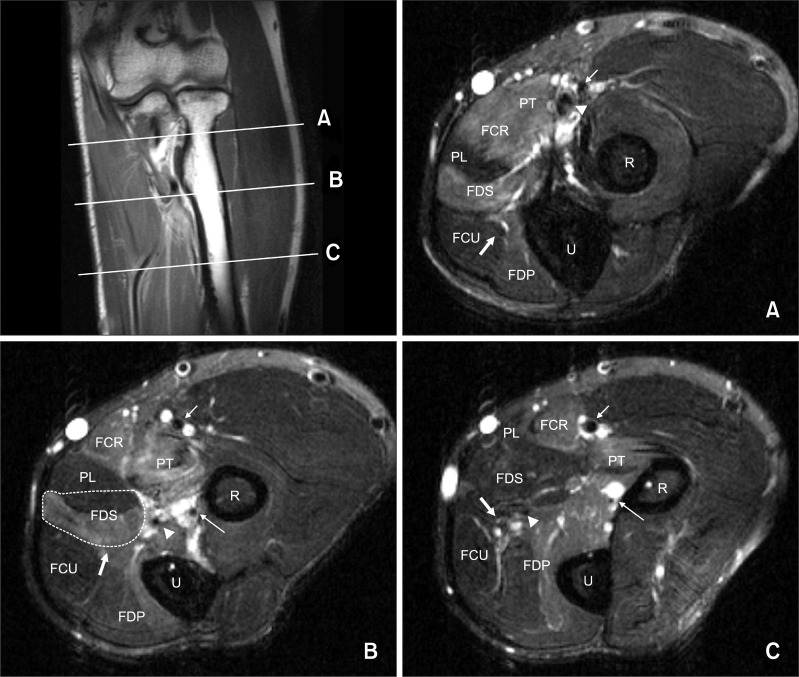 | Fig. 2Fat-suppressed T2-weighted magnetic resonance imaging of the left proximal forearm showed increased signal intensity in the PT, FCR, some portion of FDS, and deep portion of FDP. PT, pronator teres; FCR, flexor carpi radialis; FDS, flexor digitorum superficialis; FDP, flexor digitorum profundus; FCU, flexor carpi ulnaris; PL, palmaris longus; R, radius; U, ulna; arrowhead, median nerve; short arrow, superficial radial nerve; long arrow, anterior interosseous nerve; thick arrow, ulnar nerve. 
|
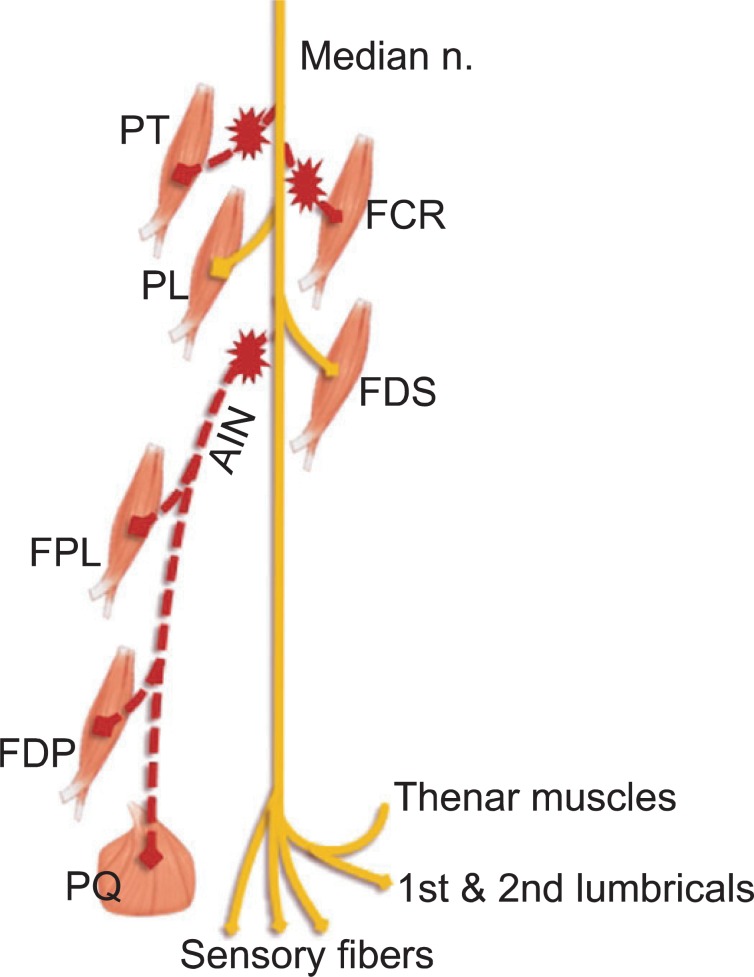 | Fig. 3Schematic diagram of possible injury mechanism of this case demonstrates injury of anterior interosseous nerve (AIN) branch accompanied by muscular branch injury of proximal median nerve in multiple sites on the antecubital area. FCR, flexor carpi radialis; FDP, flexor digitorum profundus to 2nd and 3rd digits; FDS, flexor digitorum superficialis; FPL, flexor pollicis longus; PL, palmaris longus; PQ, pronator quadratus; PT, pronator teres. 
|
Table 1
Nerve conduction study findings
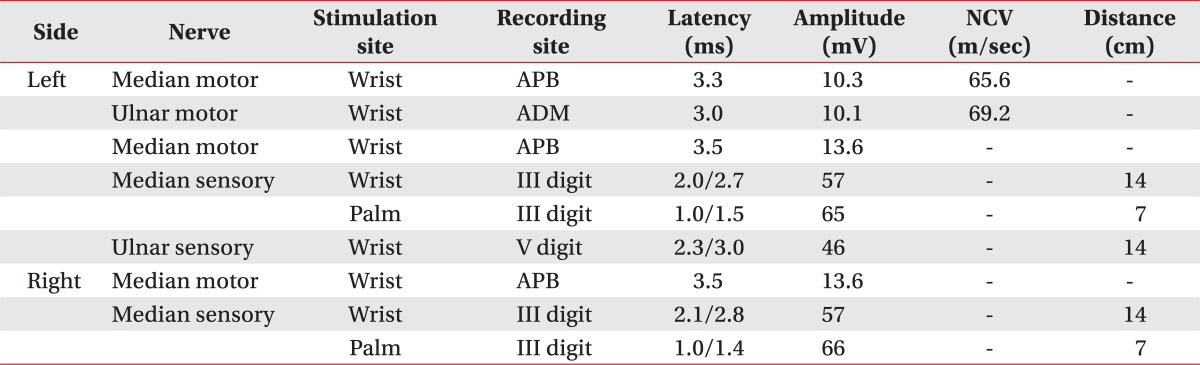

Table 2
Needle electromyographic findings

Go to :

DISCUSSION
Pseudo-AINS is a syndrome that presents clinically with findings suggestive of an AIN lesion, but actually has a median nerve lesion in the antecubital fossa, proximal to the AIN.
The classic AINS is a pure motor neuropathy with weakness of flexor pollicis longus, flexor digitorum profundus to the 2nd and 3rd digits, and pronator quadratus muscles without sensory involvement [
2]. Various etiologies causing AINS have been identified, including spontaneous, neuralgic amyotrophy, forearm muscles injection injuries, gunshot wounds, elbow arthroscopy, lacerations, pregnancy, and anomalous fibrous band [
3,
4]. The AIN is a pure motor branch of the median nerve. After the median nerve arises from the brachial plexus and passes distal to the elbow, the anterior interosseous nerve arises 5 to 8 cm distal to the lateral epicondyle. The nerve passes between the flexor digitorum profundus and flexor pollicis longus muscle, and passes along the anterior aspect of the interosseous membrane to the wrist. There are three muscles innervated by AIN; the radial portion of the flexor digitorum profundus, flexor pollicis longus, pronator quadratus in the sequence. Anatomical variations of AIN or abnormal relationship with the adjacent muscles have been reported in some cases [
5].
Injury of the AIN manifests weakness in flexion of the interphalangeal joint of the thumb or of the distal interphalangeal joints of the index and long fingers. Clinically, the patients with the nerve injury are not able to make an "O" shape using their thumb and index finger (positive "OK" sign).
In the case of pseudo-AINS, the injury site of nerve is proximal to the AIN. Therefore, the other abnormalities can be additionally shown besides the general findings according to the AIN injury during the physical exam or the electrodiagnosis. Intraneural topography of the median nerve may explain the reasons of the various symptoms and signs, including pseudo-AINS as a result of partial median nerve lesion.
This case is about the iatrogenic nerve injuries caused by multiple intramuscular steroid injections. Many clinicians use lidocaine mixed with corticosteroids to treat musculoskeletal problems. However, the adverse effects of steroids related to the nerves may be easily overlooked. Some cases have been reported that iatrogenic neuropathies were caused by steroid injection; injection at the ulnar nerve to treat medial epicondylitis and at the lateral plantar nerve to treat plantar fasciitis [
6,
7]. In our case, the mechanical and chemical injuries to AIN and muscular branches of the median nerve would be suspected as the etiologies of pseudo-AINS.
There are a few practical methods to identify nerve pathology or muscle change caused by nerve injury. The nerves that are deeply located can be identified by an MRI and the superficial nerves can be easily detected in the ultrasonography. Grainger et al. [
8] reported a case that proved an increased signal intensity and atrophic change of the muscle groups innervated by the AIN using an MRI. Hide et al. [
9] reported the sonographic findings in AINS, and found loss of muscle mass, increased reflectivity with reduction of perfusion of the affected muscle on Doppler sonography. This case demonstrated the signal change of the muscles, including pronator teres, flexor carpi radialis, partial area of flexor digitorum superficial, and flexor digitorum profundus. The palmaris longus was spared on an MRI. We concluded that the patient's symptom was caused by the injury of AIN and the muscular branch injury of the proximal median nerve, following multiple intramuscular injection around the antecubital area.
In conclusion, this case reminds us the importance of knowledge of the anatomic structures, especially the anatomical relationship between neurovascular bundle and muscles.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download