INTRODUCTION
Adhesive capsulitis is described as synovial hypertrophy and contraction,along with chronic inflammation of synovium with a relatively small amount of synovial fluid around the humeral head. More than 2% of the general population is known to have the disease; women over 50 years of age are more likely to present with this condition.
1,
2 Currently, several methods of treatment, such as physical therapy, pharmaceutical intervention, intra-articular injections, and exercise therapy are in clinical use, although the different methods show no differences in efficacy.
3-
5 The capsular distension method has a therapeutic effect, via rupture of the stiffened capsule, by hydropressure.
6
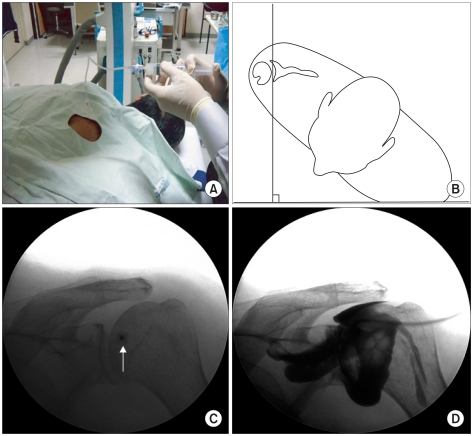
Under fluoroscopic guidance with contrast media injection, capsular distension was performed. After confirming the spinal needle's intra-articular placement in the articular cavity, contrast-mixed saline was injected until the pressure was sufficiently reduced to rupture the capsule. The rupture can be confirmed by the leakage of contrast media outside the capsule, and thisrupture usually takes place below the supscapular muscles and in the biceps' tendon sheath. The success rate of the procedure is reported at 52-82%.
5-
8
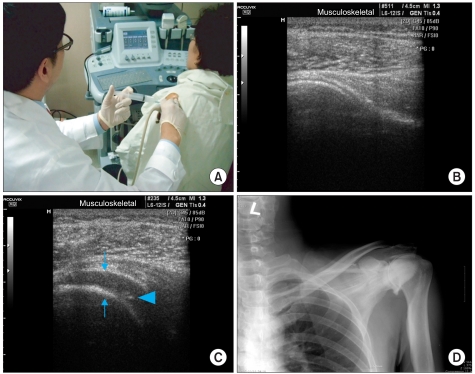
Recently, ultra-sonography is more widely used in the diagnosis and treatment of musculoskeletal disease. The injection method, using a blind anatomical marker, when previously performed, had the limitation of delivering the drug into precisely the expected space. This method also leads to limitations in evaluating treatment efficacy. The X-ray guided injection method has the advantage of delivering drugs to the targeted space but the disadvantage of radiological exposure for both patients and clinicians. Additionally, this method can only be performed in a well-equipped healthcare service. On the other hand, ultra-sonography can be easily used in an outpatient setting, without the fear of radiological exposure.
Gam et al.
5 compared the efficacy of the capsular distension method with the glucocorticoid injection to glucocorticoid alone. Their results showed a definite improvement in range of motion along with the actual capsular distension seen in US.
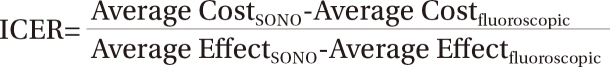
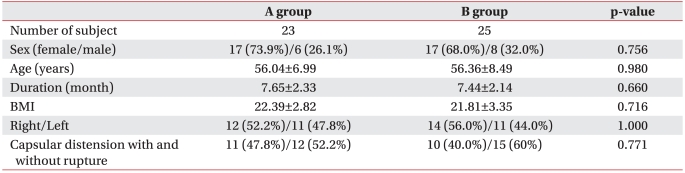
5 However, few studies have been conducted to investigate the pros and cons of sono-guided capsular distension, compared with fluoroscopically guided capsular distension in patients. This study aims to evaluate this very issue.
Go to :

DISCUSSION
The capsular distension method separates adherent synovium by hydropressure caused by injection of a large amount of fluid mixture. Since Salter had reported its effectiveness in 1970, it is widely used for its low cost, safety, and immediate effect in ROM, in patients with adhesive capsulitis.
14 Rizk et al.
6 explained that capsular distension shares a similar mechanism with manual reduction under anesthesia, and patients with no improvement after 3 months of conservative management should be treated.
Although controversy still exists regarding whether the primary pathology of adhesive capsulitis is inflammation or fibrosis, it is thought that its development is limited to the capsule with the synovial inner layer and synovial fluid.
15 Rodeo et al.
16 reported that cytokines such as Transforming Growth Factor-β (TGF-β) and Platelet-Derived Growth Factor (PDGF) play critical roles in the inflammatory reaction and fibrosis, and the differentiation process of fibroblasts was observed. Steroid injection was started as treatment based on the hypothesis that the main pathophysiology of capsulitis is an inflammatory response.
Neviaser
17 reported mild synovial inflammation accompanied by edema, vasodilation, and the deposition of mononuclear cells in some patients with adhesive capsulitis.
As inflammation also plays an important role in the process of synovial fibrosis, anti-inflammatory treatment is necessary for symptom improvement and prevention of further fibrosis. Thus, intracapsular steroid injection in adhesive capsulitis shows efficacy by reducing inflammatory response in the pathological process.
18 Additionally, if performed accurately, it produces faster pain control and ROM improvement with lower cost compared to conservative physiotherapy; thus, it has recently been widely used for outpatients.
19-
21
In 1989, Fareed and Gallivan
8 showed excellent efficacy of 40 ml steroid and saline mixture injection treatment, without individuals needing to be admitted to the hospital or needing to use arthroscope. Gam et al.
5 reported that patients who received capsular distension with steroids, via a US-guided posterior approach, showed more ROM improvement and reduced use of painkillers compared with patients who received intra-articular steroid injections. The initial mechanisms of hydraulic distension are capsular rupture and pressure-lowering by capsular volume extension, then anti-inflammatory effects produced by administration of steroid, local anesthetics, and contrast media.
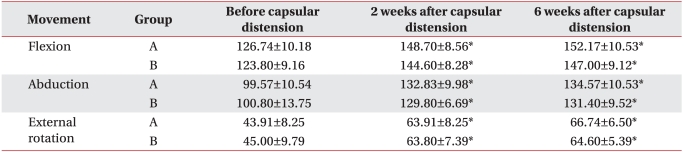
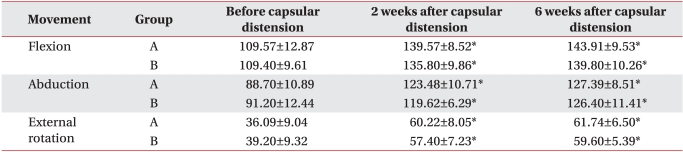
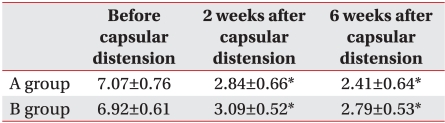
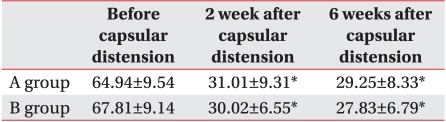
6 In this study, additional steroid injection with capsular distension showed improvement in ROM, pain, and functional ability.
Several studies have investigated injection-targeting accuracy in blind trials. Yamakado
22 reported that, when evaluated with arthrography, targeting accuracy of reaching the subacromial bursa was judged to be about 70%. Partington and Broome.
23 reported the targeting accuracy to be about 83% in reaching the subacromial bursa and 60% in reaching the acromioclavicular joint with blind injection on cadavers. Erroneous decisions in diagnosis and treatment efficacy evaluation can be made with inaccurate injection. The US-guided and fluoroscopic methods used in this study can reduce such errors.
Diagnostic tools for adhesive capsulitis are: arthrography, magnetic resonance imaging (MRI), arthroscopy, and musculoskeletal ultra-sonography. Arthrography displays loss of axillary folds and biceps and reduction of articular volume below 10 ml. It is usually introduced as the examination of choice,
1,
24 but has the disadvantage of being too invasive to be easily clinically applicable; it also has diagnostic limitations in patients whose articular volume has not decreased below 10 ml. Additionally, the risk of radiological exposure to both patients and examiner is high. Additional radiological studies may be necessary in order to rule out other rotator cuff diseases.
Holsebeeck and Introcaso.
25 reported sonographic findings of adhesive capsulitis as continuous limitations of subacromial suprasinatus sliding movements in shoulder abduction and the lateral view of supraspinatus. Sonography enables diagnosis during direct monitoring of patients' movements, without risk of radiological exposure. Furthermore, sonographic measurement of the coracohumeral ligament's thickness in the girdle band is useful in diagnosing adhesive capsulitis.
26
In performing sonographic capsular distension, it was difficult to access the full view of the capsule, as in fluoroscopy. To compensate for this defect, distension was confirmed during drug injection, and an additional fluoroscopic exam using contrast media was performed in order to check the shoulder capsule following drug injection.
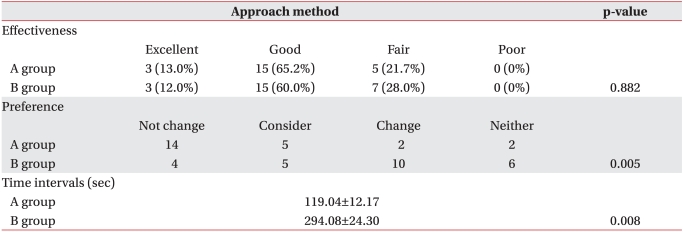
Efficacy for the two groups showed no statistical differences but with regard to preference, 24 patients (50%) of the total study population chose sonographic capsular distension and had higher preferences for it than fluoroscopic distension, which was chosen by only 6 patients (12.5%).
The main reason patients preferred sonographic distension was lack of radiological exposure. X-rays during fluoroscopic distension mean a type of ionizing radiation and have potent biological effects. Even a small amount can cause molecular damage and be carcinogenic in the future.
27 The International Commission of Radiological Protection estimates the annual maximal permissible dose on several organs and recommends that an examiner or patient not be exposed to more than 10% of the permissible dose.
28 The usual incidental skin dose during a one-minute fluoroscopic interventional procedure is 1-10 R (Roentgen) with a 2R per minute ray, equal to a radiological exposure of 130 times a chest radiograph, as an incidental skin dose of a typical chest X-ray is 15 mR (milliroentgen).
25 Thus, a procedure without risk of radiological exposure is preferred.
A total of 8 patients, 2 in group A and 6 in group B, refused both procedures because of pain during involved in them. As pain can reduce patients' compliance to procedures, further studies ought to be performed in this field.
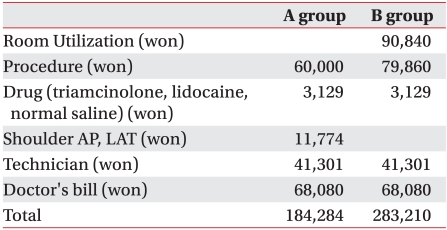
The limitations of this study were the small number of patients and the short (6-week) follow-up period. Enrollment criteria included patients of 1 and 2 grade adhesive capsulitis, with symptom duration lasting between 3 months and 2 years, but grade 3 patients could have been included for period overlap. Additionally, the cost was calculated for four different hospitals, for reliable results in evaluating cost-effectiveness. However, the part of the cost not covered by insurance differed among hospitals and was a limitation in analysis of cost-effectiveness. Even though individuals were examined by an expert with 5 years of experience in musculoskeletal ultrasonography and C-arm, the procedure time differences according to inter-examiners' performance abilities remains a limitation.
A larger number of subjects, with a longer follow-up period comparing multiple methods of capsular distension, are needed in order to fully assess efficacy and cost-effectiveness in the future.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download