A 49-year old female patient was admitted to the department of neurosurgery at another hospital under the diagnosis of a subarachnoid hemorrhage. She underwent a decompressive craniectomy, surgical neck clipping of ruptured aneurysm and hematoma removal. The patient was treated in the intensive care unit for three weeks. The patient had no prior operative history of tracheostomy, and a cranioplasty was performed. Following the completion of intensive care, the patient was moved to a general ward, and transferred to the department of rehabilitation medicine. At the time of the transfer, the patient was alert and conscious with motor power in the right upper and lower extremities that presented at a grade one on examination. To independently turn-over in bed was possible, but sitting-up required moderate assistance. The patient showed difficulty in maintaining balance while seated and generally required moderate assistance in daily activities. The patient was on Levin tube feeding, and treatment for dysphagia was carried out. The patient was transferred to our department of rehabilitation medicine at ten weeks after the onset of a hemorrhagic stroke. On admission to our hospital, the patient presented with persistent dysphagia, and was still receiving Levin tube feeding. Cervical pain with severity of grade four to five according to visual analogue scale was rated by the patient. The exact onset of diabetes mellitus was uncertain but HbA1c was 5.5% on laboratory examination, and the patient had no family history of diabetes mellitus. The patient was on insulin therapy, but the medication regimen was modified to the administration of Metformin Hydrochloride 500 mg two times a day owing to adequate control of blood glucose level, and afterward, the patient had a favorable blood glucose level. The vital signs were stable on admission with a blood pressure at 106/73 mmHg, heart rate 98/minute, respiratory rate 19/minute and body temperature of 36.3℃, and the patient did not present with respiratory distress. Motor power examination showed normal findings on the left side, but the right upper extremity presented with a grade one and the right lower extremity presented with grade two. Her cognitive function was rated with score of 22 according to Korean Mini-Mental State Examination (K-MMSE). Blood test results showed no remarkable abnormal findings other than a mildly elevated ESR level of ESR 36 mm/hr. Other results revealed WBC 8,410/µl and CRP 0.04 mg/dl. On a video fluoroscopy swallowing test for the evaluation of dysphagia, retropharyngeal edema was identified, which lead to impairment of a migration of bolus into the esophagus, and the aspiration occurred due to residual contents (
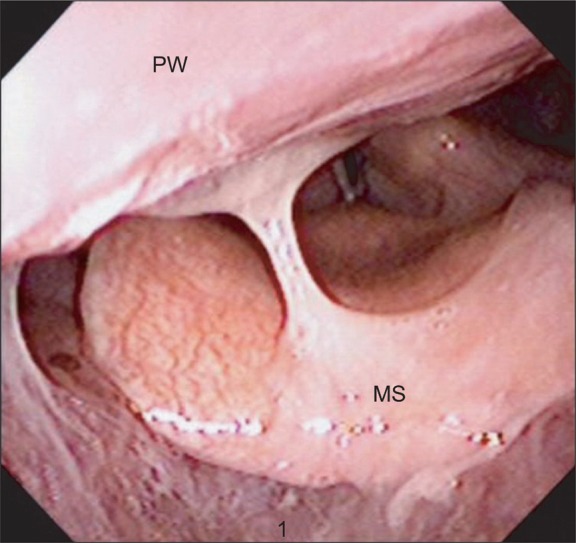
Fig. 1-A). With a consultation to the department of otolaryngology, a laryngoscopy was performed and retropharyngeal edema and profuse discharge were identified (
Fig. 2). A cervical computed tomography examination showed generalized retropharyngeal edema and cortical contrast enhancement of the fourth cervical spine along with partial osteoclastic findings (
Fig. 3). An additional differential diagnosis of retropharyngeal abscess, malignant tumor and tuberculous spondylitis, cervical magnetic resonance imaging (MRI) was carried out, and revealed a signal change at the medulla from the second to the fourth cervical spine along with generalized retropharyngeal edema. At the anterior portion of the second to fourth cervical spine, a soft tissue lesion of low signal intensity on T1, high signal intensity on T2, and contrast enhancement was identified (
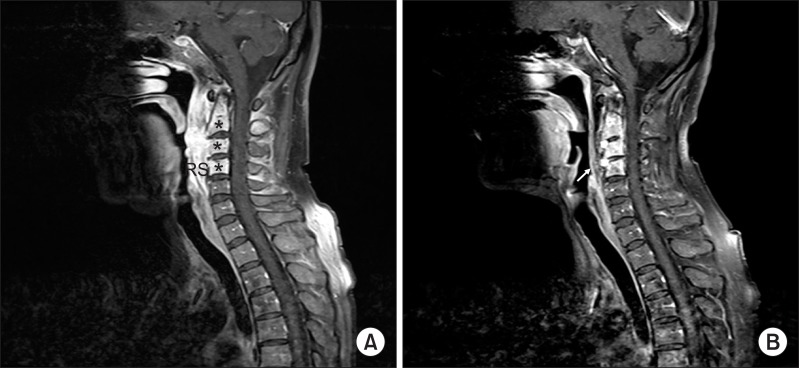
Fig. 4-A). The marginal portion of the abscess did not show contrast enhancement, and the posterior portion of the vertebral body adjacent to the retropharyngeal space showed contrast enhancement. This lead to difficulty in excluding the malignant tumor, and a biopsy was planned. The location of the lesion was difficult to access for complete resection or incision and drainage. Since the trial of the incision and drainage does not affect the period of antibiotics administration, an excisional biopsy under local anesthesia was performed, and an acid-fast bacillus stain along with a culture study was carried out. Biopsy results revealed findings consistent with inflammatory granulation tissue and acid-fast bacillus staining which showed no specific findings. A culture study showed positive results for Staphylococcus aureus susceptible to methicillin. The lesion was concluded as a retropharyngeal abscess, and treatment with antibiotics was initiated with the administration of intravenous Cefazolin 2 g every 8 hours. The total treatment period with antibiotics was eight weeks. The follow-up evaluation with blood tests showed no abnormal findings regarding the WBC, ESR and CRP. Re-evaluation with cervical MRI after treatment with antibiotics showed improvement of a retropharyngeal abscess (
Fig. 4-B). On video fluoroscopic swallowing study, aspiration was not observed, and the residual contents were remarkably decreased leading to initiation of feeding with a regular diet (
Fig. 1-B). The cervical pain was managed with the administration of Tramadol HCL 18.75 mg/Acetaminophen 162.5 mg three times a day since admission but did not show improvement. However, the cervical pain started improving after the initiation of treatment with intravenous antibiotics. Medication with Tramadol HCL 18.75 mg/Acetaminophen 162.5 mg was administrated for a total period of four weeks, and the patient no longer complained of cervical pain.
 | Fig. 1Video fluoroscopic swallowing study. (A) On lateral radiographic image taken prior to administration of antibiotics, residual barium is visualized at the pyriform sinus and vallecular sinus of the pharynx (thick arrows). Extensive edema in the retropharyngeal space (RS) and some aspirated barium in the airway is seen (thin arrow). (B) A decreased amount of residual barium was identified at pyriform sinus and vallecular sinus following treatment with antibiotics for a period of 8 weeks (thick arrows), and there were no signs of aspiration (thin arrow). 
|
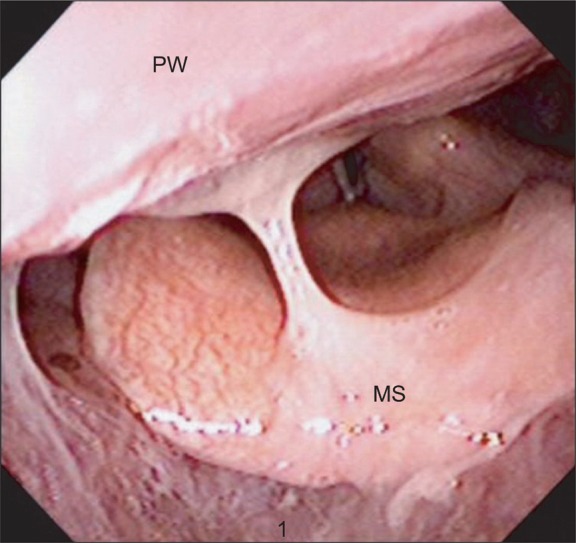 | Fig. 2The laryngoscopic finding. The features show edema of the posterior pharyngeal wall (PW) and a large amount of mucous secretion (MS). 
|
 | Fig. 3A CT of the neck with contras. Extensive edema of the retropharyngeal space (RS) and a focal patchy enhancing lesion (*) near osseous lesions (arrow) are identified. 
|
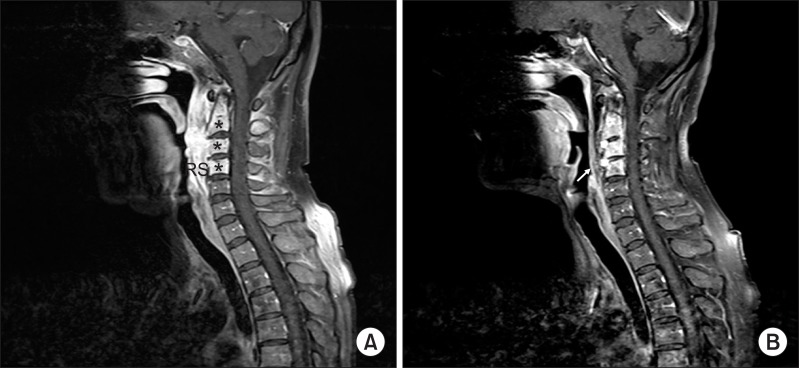 | Fig. 4A contrast cervical spine MRI. (A) Contrast-enhanced sagital T1-weighted fat suppression image (before administrating antibiotics). Alteration of signal intensity at medulla of C2-C4 cervical spine level (*). A well enhanced soft tissue lesion that suggests a retropharyngeal abscess at prevertebral space is identified (RS). (B) A well enhanced soft tissue lesion was improved following treatment with antibiotics for 8 weeks (arrow). 
|






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download