This article has been
cited by other articles in ScienceCentral.
Abstract
Thyroid carcinoma is the commonest endocrinological malignancy. After papillary thyroid carcinoma (PTC), follicular thyroid carcinoma (FTC) is the second most common histological subtype. Common presentations of FTC include a solitary thyroid nodule and cervical lymphadenopathy. The incidence of individuals diagnosed with thyroid cancer showing initially distant metastatic disease ranges from 1 to 9%. Also, the incidence of solitary bone metastasis from thyroid is only 2 to 3%. We report a case of a patient with FTC whose initial presentation was low back pain and right buttock pain due to vertebral metastasis rather than the usual neck lumps or symptoms of thyroid disease.
Go to :

Keywords: Follicular thyroid carcinoma, Spinal metastasis, Compression fracture
INTRODUCTION
Papillary and follicular carcinomas of the thyroid gland, often referred together as differentiated thyroid cancer (DTC), is one of the most curable cancers and has a good prognosis and only rarely presents with distant metastasis at initial diagnosis.
1 After papillary thyroid carcinoma (PTC), follicular thyroid carcinoma (FTC) is the second most common histological subtype. Common modes of initial presentation include a solitary thyroid nodule, a dominant nodule in a multinodular goiter and cervical lymphadenopathy.
2 There have been several reported cases of DTC presenting as a distant metastasis as an initial symptoms, but the initial presentation as a compression fracture due to metastasis is extremely rare and seldom reported in the literature. In this paper, we present a case of a patient with FTC that metastasized to the vertebral body causing a compression fracture and who presented without common thyroid symptoms, and with laboratory findings that did not suggest thyroid disease or metastatic bone tumor.
Go to :

CASE REPORT
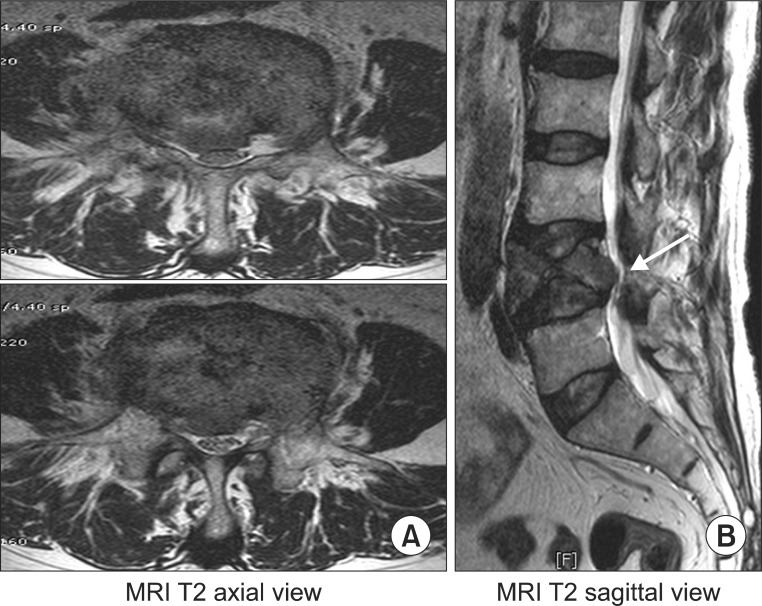
A 72-year-old male patient with low back and right buttock pain was examined. He could not walk more than 100 m because of the pain. He did not have any common symptoms of thyroid disease or malignancy such as weight loss. There were no abnormal laboratory findings. Neurologic evaluation revealed motor weakness in the right leg, especially weakness of big toe dorsiflexion and there was hypoesthesia in the right side below the L5 dermatome. A lumbar spine X-ray revealed only an L4 compression fracture, and the pedicles were preserved (
Fig. 1). The whole body bone scan showed an active bone lesion in L4 vertebra, only. MRI findings were suggestive of an infectious spondylitis such as tuberculous (TB) spondylitis associated with a pathologic fracture rather than a metastatic bone tumor because vertebral involvement by metastasis may occur without collapse or subligamentous spread and disks are usually preserved. Additionally, the imaging features that support TB spondylitis over spondylitis caused by other infections include larger paraspinal involvement, the presence of subligamentous spread, more bone destruction, a paucity of sclerosis and local periosteal reaction (
Fig. 2).
3
 | Fig. 1X-ray showed only L4 compression fracture, with preservation of the pedicles (arrow). (A) Anterior-posterior view. (B) Lateral view. 
|
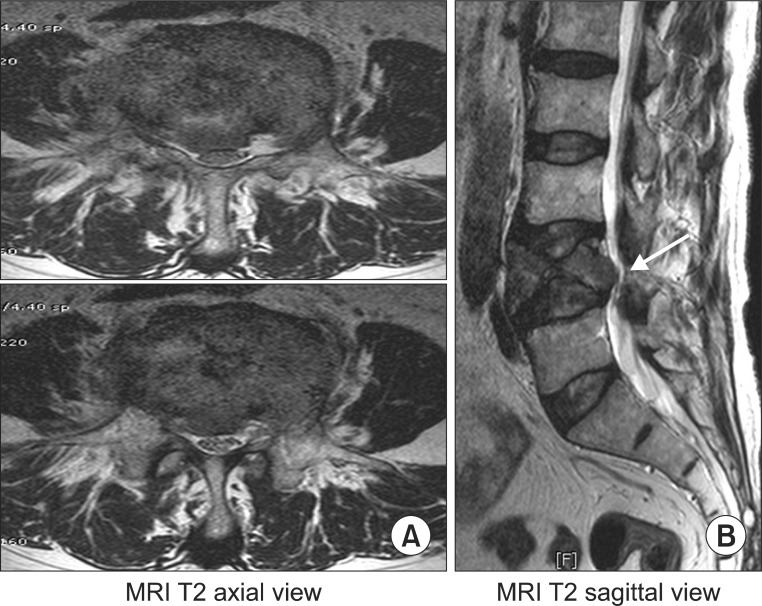 | Fig. 2MRI had appearances suggestive of an infectious spondylitis such as TB spondylitis associated with a pathologic fracture rather than a metastatic bone tumor (arrow), because vertebral involvement by metastasis may occur without collapse or subligamentous spread and disks are usually preserved. (A) T2 Axial view. (B) T2 Sagittal view. 
|
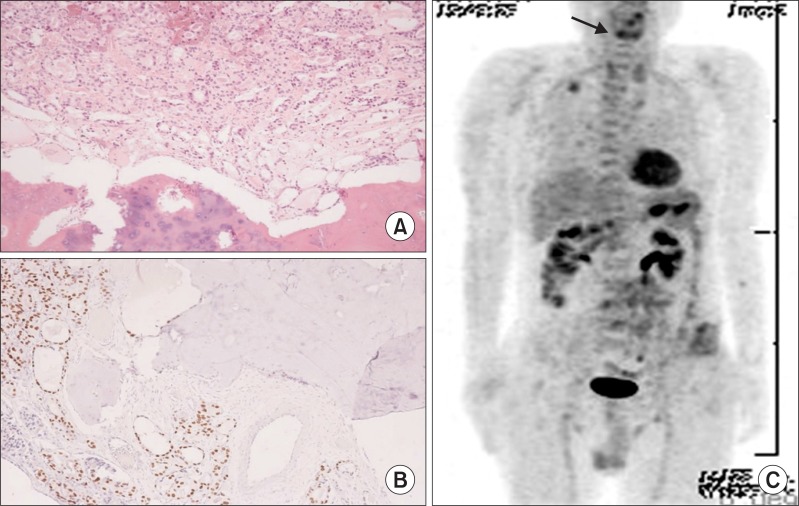
After the patient was transferred to the department of neurosurgery, a TB study was performed, showing no evidence of TB of any organ. The lumbar spine CT showed a markedly collapsed L4 body with an ill-defined intramedullary mass formation with cortical bone and bone marrow destruction, which suggested a malignant compression fracture with a large anterior epidural mass and perispinal extension. Investigations were performed to rule out multiple myeloma or metastasis. He went through L4 corpectomy with mass removal, and expandable cage insertion with posterior spinal fusion. A frozen biopsy during surgery revealed metastasis of the thyroid glands. Histologically, the mass in the vertebral body demonstrated well-differentiated follicles containing colloid invading the surrounding trabecular bone (
Fig. 3-A). The tumor showed positive immunoreactivity for a protein of thyroid origin (thyroid transcription factor-1 [TTF-1]) (
Fig. 3-B).
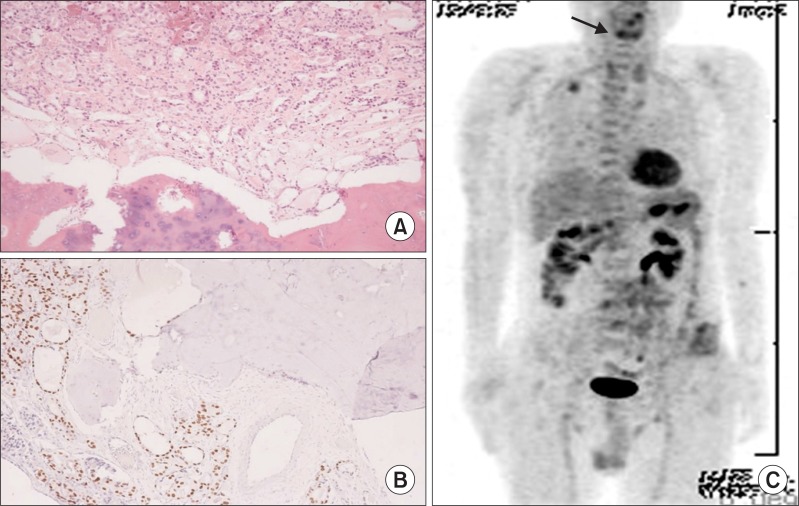 | Fig. 3(A) Frozen biopsy: The upper part of figure is tumor and the lower part is bone. Histologically, the mass in the vertebral body demonstrated well-differentiated follicles containing colloid invading the surrounding trabecular bone (H&E stain, ×40). (B) Immunochemistry staining: Positive immunoreactivity for the existence of proteins of thyroid origin (TTF-1) (H&E stain, ×40). (C) PET showed mildly increased FDG uptake in both thyroid glands (arrow). 
|
After the surgery, whole body fusion PET showed mildly increased FDG (fluorodeoxyglucose) uptake in both thyroid glands (
Fig. 3-C). Three weeks after the spinal surgery, he went through total thyroidectomy. The pathologic findings of the removed thyroid was minimal invasive follicular carcinoma, measuring 1.6×1.5×1.3 cm
3, with a negative resection margin and no metastasis out of 6 lymph nodes. Two months after thyroidectomy, treatment with radio-iodine (RI) therapy was begun and the right buttock pain and weakness of right leg resolved. He has not had any debilitating pain for 15 months since the surgery.
Go to :

DISCUSSION
DTC is one of the most curable cancers known, characterized by a slow progressive course and less invasiveness than most other cancers. This is thought to be due to the biological behavior of the tumor and the effectiveness of initial therapy, consisting in most patients of total thyroidectomy followed by RI treatment. Despite the good outcome level compared with other cancers, distant metastasis is the predominant cause of thyroid cancer-specific mortality.
4 The 10-year survival rate of DTC is as high as 80 to 95%, but when accompanied by distant metastasis, the 10-year survival rate decreases to 40%. According to the site of the distant metastasis, the reported 10-year survival rate is 62 to 86% in lung metastasis, 13 to 21% in bone metastasis, and less than 10% in brain metastasis.
5
In DTC, the presence of vascular invasion even in small tumors predicts the presence of distant metastases.
6 But in this case, although the pathologic study revealed no vascular invasion around the thyroid tumor, the FTC presented with distant metastasis. These metastatic lesions can be identified by histopathologic study with excisional biopsy or fine needle aspiration of lesions, systemic radiologic study, such as whole body fusion PET, followed by confirmation with an elevated thyroglobulin level. In this case, the metastasis of FTC was confirmed by both histopathologic study of the removed thyroid and whole body fusion PET, followed by investigation of the thyroglobulin level.
Distant metastasis has been reported in about 4-9% of DTC during its clinical course. Metastasis is frequently occurs in the lung (72-76%) and skeletal system (19-23%), but rarely occurs in the central nervous system (1%), liver or skin.
5 The skeletal system is the second most common systemic site of distant metastasis following the lung.
7-
9 However, the incidence of distant metastases at the time of initial presentation of well-differentiated thyroid cancer is only approximately 4%.
10 Therefore, if the first manifestation of clinical symptoms is the result of metastasis, the diagnosis of primary thyroid cancer is difficult, and unnecessary diagnostic tests may be performed or the diagnosis delayed.
In conclusion, patients presenting with lesions suspicious of secondary malignancy in the axial skeleton should be clinically evaluated for thyroid cancer.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download