Abstract
In herpes zoster infection, neurological complications may be overlooked because pain is a more prominent symptom and because peripheral polyneuropathy associated with weakness is rare. A 57-year-old male visited our hospital, complaining of pain and skin eruptions on the right flank. He was diagnosed as having herpes zoster and the symptoms were alleviated by administration of acyclovir for a week. After three weeks, the herpes zoster relapsed. He was re-admitted and diagnosed with chronic myeloid leukemia (CML), and imatinib mesylate was prescribed for five weeks. Ten weeks after the onset of herpes zoster, bilateral foot drops and numbness of the right foot dorsum developed. Through an electrodiagnostic study, he was diagnosed as having peripheral polyneuropathy that was suspected to be caused by neural invasion by varicella zoster virus. After administration of famciclovir, not only the pain but also the neurologic symptoms improved. We herein report a case of peripheral polyneuropathy that was supposed to be related to herpes zoster.
Herpes zoster is a viral disease characterized by pain and skin eruptions in specific dermatomes. It is caused by reactivation of varicella zoster virus that was dormant in the spinal dorsal root ganglion.1,2 Mostly, herpes zoster can be cured without any complications; yet various types of complications concerning the nervous system can occur.3 However, complications in the nervous system caused by herpes zoster are difficult to diagnose because neurological complications are uncommon.3 Besides, not only patients but also clinical practitioners fail to notice the complications because they usually focus only on severe pain.3 Motor paralysis occurring in herpes zoster can be categorized into segmental paresis and non-segmental paresis depending on whether the dermatome of the skin eruption matches relevant parts of the motor nervous system including the myotome and peripheral polyneuropathy can be classified in non-segmental paresis.4 Based on research, segmental paresis casuistics have been constantly reported domestically and internationally, but non-segmental paresis including peripheral polyneuropathy has not been reported domestically. A few herpes zoster peripheral polyneuropathy casuistics have been reported abroad, but a detailed explanation of electrodiagnostic findings is insufficient and the possibility of diabetic peripheral neuropathy has to be taken into consideration.5,6 We experienced a case of peripheral polyneuropathy with foot drop after herpes zoster infection in a CML patient without any other diseases including diabetes supposed to be related to peripheral polyneuropathy. So we herein report the case along with the electrodiagnostic findings.
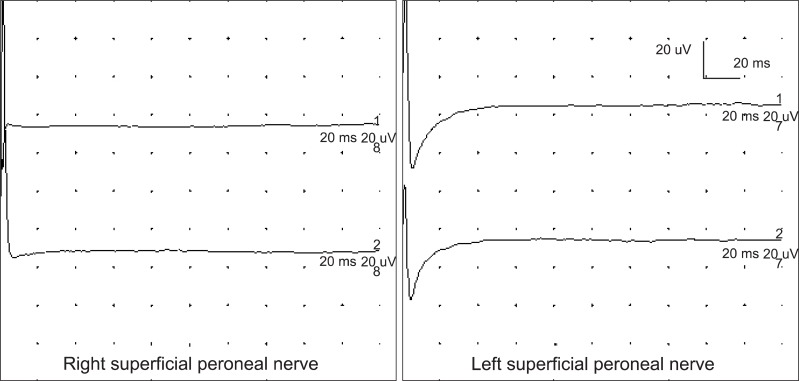
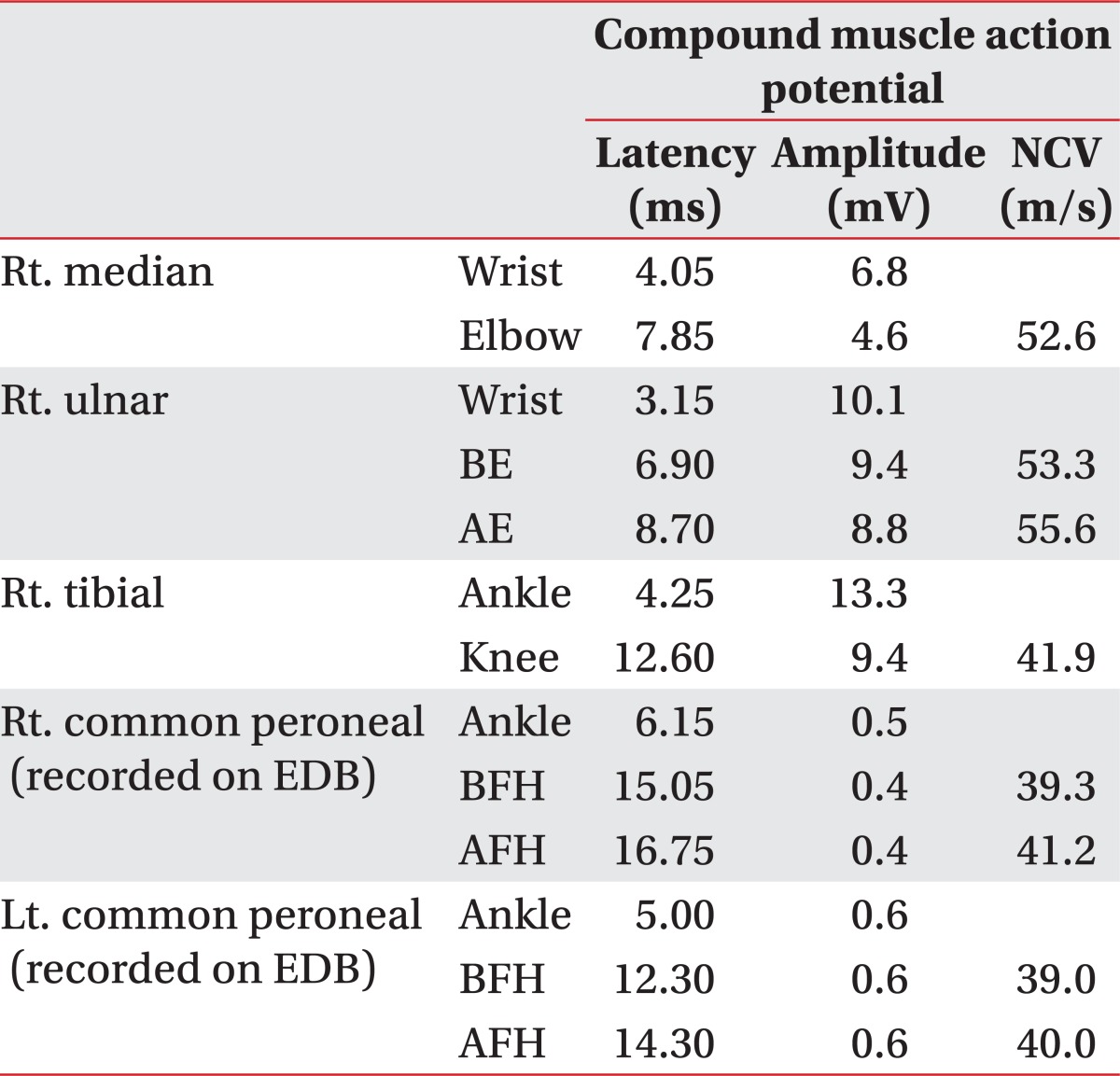
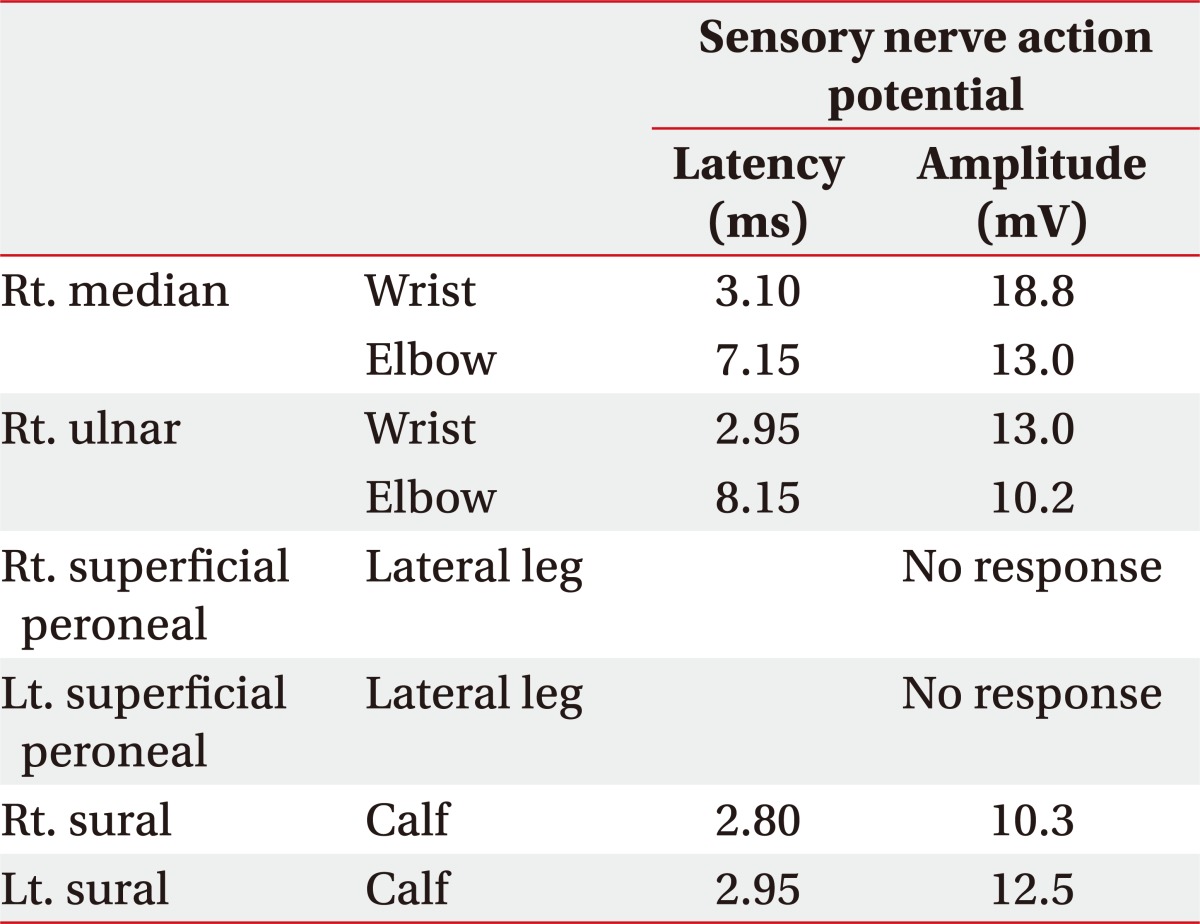
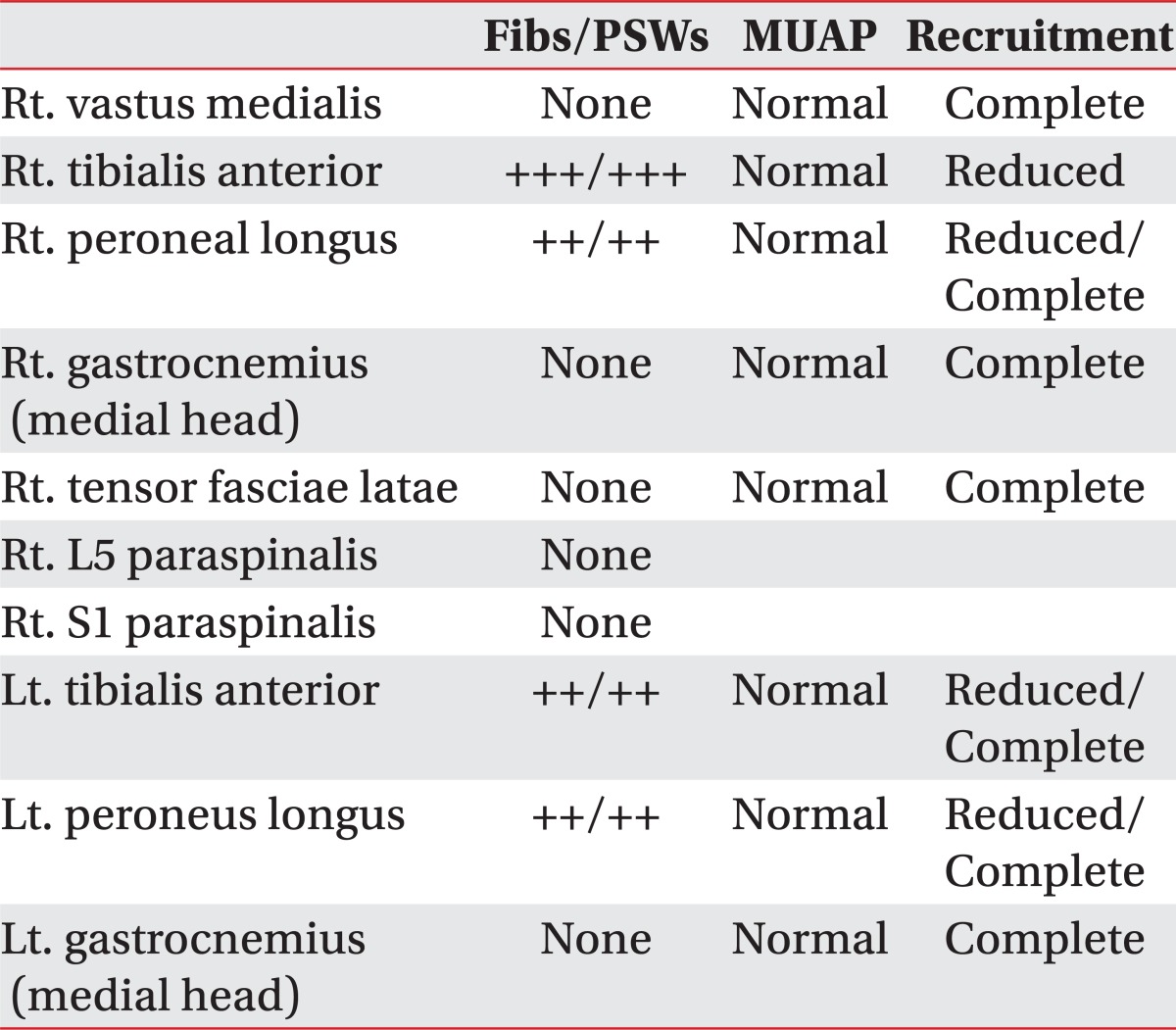
A 57-year-old patient visited the department of dermatology with pain and skin eruptions on his right T11 dermatome (Fig. 1-A). The patient had no underlying diseases such as diabetes or hypertension, or a medical history of any trauma or surgeries. Following a dermatological examination, he was hospitalized for herpes zoster. After a week of acyclovir intake, the symptoms faded and he was discharged from the hospital. There were no complications or recurrences for the next three weeks. But in the fourth week, the symptoms recurred and the patient was hospitalized and kept in the department of anesthesiology. At the time of hospitalization, the white blood cell count was 173,000/µl and the myelocyte count was 29 times the erythrocyte count in a bone marrow aspiration study. The karyotype was found to be 46, XY, t(9; 22) (q34; q11.2) so the patient was diagnosed with CML with a positive Philadelphia chromosome. The patient was immediately transferred to the department of hemato-oncology and began chemotherapy with Glivec® (Novartis, Basel, Switzerland). During chemotherapy, a remedial effect was observed through the complete blood cell count and nine weeks after being diagnosed with herpes zoster (five weeks afterchemotherapy), the patient stopped Glivec® intake due to pancytopenia. Also, aspiration pneumonia occurred and he was diagnosed with dysphagia after a videofluoroscopic swallowing study carried out in the department of rehabilitation medicine. Ten weeks after the herpes zoster diagnosis, foot drop in both feet and hypoesthesia in right foot dorsum occurred, but these symptoms were unnoticed due to severe pain and lack of evaluation of the motor-sensory system. Thirteen weeks after herpes zoster diagnosis, hypoesthesia and foot drop were detected by physical examination as the patient was being transferred to the department of rehabilitation medicine for swallowing rehabilitation (Fig. 1-B). In the manual muscle test, the muscular strength of the ankle dorsiflexor was reduced to II/III (right/left) and the muscular strength of the extensor hallucis longus was reduced to II/III (right/left). Also, the touch sense of the right foot dorsum was down to 50%. But the deep tendon reflex was normal. An electrodiagnostic study showed that the amplitudes of the compound muscle action potentials of both common peroneal nerves were reduced at the extensor digitorum brevis (Table 1) (Fig. 2) and the sensory nerve action potentials of both superficial peroneal nerves were not generated in the sensory nerve conduction study (Table 2) (Fig. 3). Besides, the results of a nerve conduction study on both tibial and sural nerves, right median nerve, and right ulnar nerve were normal. In needle electromyography, a denervation potential was observed in both tibialis anterior and peroneus longus, and a reduction in the recruitment pattern was also observed (Table 3). In conclusion, the patient was diagnosed with peripheral polyneuropathy of the axonal type. After the electrophysiologic diagnosis, antiviral therapy using famciclovir began, along with rehabilitation for muscular weakness in both legs. The patient took famciclovir for a week and the foot drop in both feet and hypoesthesia in right foot dorsum were greatly alleviated. Fourteen weeks after herpes zoster diagnosis (after a week of famciclovir intake), the manual muscle test showed that muscular strength of the ankle dorsiflexor and extensor hallucis longus improved to III/IV and II/IV respectively. The hypoesthesis of the right foot dorsum was completely alleviated during this week and famciclovir intake was stopped. Eighteen weeks after herpes zoster diagnosis (one month after famciclovir intake), the muscular strength of the foot dorsum and extensor hallucis longus improved to III/V and II/V, respectively. After two months of famciclovir intake, the foot drop no longer occurred when walking.
Up to date, it is generally assumed that motor nervous system complication of herpes zoster can be occurred through the following several ways. First, it can be caused as infection that first begins in spinal dorsal root ganglion and then progresses to anterior horn through motor nerve root. Second, it can be a result of segmental myelitis. Third, it can be caused by secondary degeneration of affected motor nerve root. Fourth, it can be caused by inflammation of both sensory and motor nervous system.3 Of neurological complications in herpes zoster, segmental paralysis is focal motor paralysis that occurs in a myotome corresponding to the dermatome having a skin eruption, which occurs in approximately 0.5-5% of all herpes zoster cases.4 On the other hand, there have been six reports of non-segmental peripheral polyneuropathy to date. Mondelli and colleagues6,7 reported four cases of patients with peripheral polyneuropathy diagnosed as a complication with no relation to the dermatome, along with electrodiagnostic findings. However, in four cases, all patients were diagnosed with diabetes; so diabetic peripheral neuropathy had to be taken into consideration. Also, Dayan and colleagues5 reported two cases of patients diagnosed through nerve biopsy and electrodiagnostic findings, but the electrodiagnostic finding was insufficient because there's only nerve conduction study. The pathophysiology of peripheral polyneuropathy secondary to herpes zoster is unclear, but the discovery of varicellar zoster virus and its products in endoneurium, perineurium and epineurium within the peripheral nervous system (PNS) shows that the virus itself or the viral infection causes neural damage as they move from spinal dorsal root ganglion to nerve root and PNS.6,8 In this case, a skin eruption occurred in the left T11 dermatome and the motor paralysis occurred symmetrically in both foot dorsiflexors and extensor halluces longus related to the L5-S1 myotome. Thus, the motor paralysis in this case is classified as non-segmental paralysis that is diagnosed as peripheral polyneuropathy by a electrodiagnostic study. Neurological complications caused by herpes zoster are difficult to notice by both patients and clinicians due to the presence of severe pain.3 In this case, neurological complications were not detected in the early stages of disease because of the severe pain, and assessment during walking could not be carried out due to aspiration pneumonia. Generally, herpes zoster can be cured without any complications.3 However, in this case, the patient had a compromised immune system that had been affected by CML. So, the varicella zoster virus might have a relatively strong pathogenicity. And due to the strong pathogenicity, the herpes zoster could not be cured as easily as other general cases, and even progressed to neurological complication. The typical chemotherapeutic agent for CML with a Philadelphia chromosome is Glivec®. In this case, the patient took Glivec®, therefore the possibility of neurological complications caused by Glivec® has to be taken into consideration. However, until now, neurological complications caused by Glivec® have been reported only once - in a patient who was administered Glivec® for 5.5 years.9 In this case, the patient stopped Glivec® intake due to pancytopenia and the neurological complication occurred after a week of Glivec® intake. So it is very unlikely that Glivec® is the cause of the complication. In addition, since there had been remarkable improvement after antiviral agent intake, there is a higher possibility that the neurological complication was caused by invasion by varicella zoster virus into the peripheral nervous system. For patients with compromised immune systems due to CML, herpes zoster is difficult to cure and the disease can even progress to produce complications in the PNS. Therefore, we suggest that assessment and thorough treatment of herpes zoster infection in patients with compromised immune s y s t em, focus ing on ne r vous s y s t em complications (including peripheral polyneuropathy) as well as pain are essential.
References
1. Meier JL, Strauss SE. Comparative biology of latent varicella-zoster virus and herpes simplex virus infections. J Infect Dis. 1992; 166(Suppl 1):S13–S23. PMID: 1320646.
3. Her Y, Kim CW, Kim SS. A clinical study of motor involvement by herpes zoster. Korean J Dermatol. 2010; 48:468–473.
4. Yoleri O, Olmez N, Oztura I, Sengul I, Gunaydın R, Memis A. Segmental zoster paresis of the upper extremity: a case report. Arch Phys Med Rehabil. 2005; 86:1492–1494. PMID: 16003688.

5. Dayan AD, Ogul E, Graveson GS. Polyneuritis and herpes zoster. J Neurol Neurosurg Psychiatry. 1972; 35:170–175. PMID: 5037030.

6. Mondelli M, Romano C, Rossi S, Cioni R. Herpes zoster of the head and limbs: electroneuromyographic and clinical findings in 158 consecutive cases. Arch Phys Med Rehabil. 2002; 83:1215–1221. PMID: 12235600.

7. Mondelli M, Scarpini C, Malandrini A, Romano C. Painful neuropathy after diffuse herpes zoster. Muscle Nerve. 1997; 20:229–231. PMID: 9040664.

8. Haanpaa M, Hakkinen V, Nunmikko T. Motor involvement in acute herpes zoster. Muscle Nerve. 1997; 20:1433–1438. PMID: 9342160.

9. Chakupurakal G, Etti RJ, Murray JA. Peripheral neuropathy as an adverse effect of imatinib therapy. J Clin Pathol. 2011; 64:456. PMID: 21278395.

Fig. 1
The photographs show (A) typical skin rash and vesicles of herpes zoster confined to right T11 dermatome, and (B) weakness of bilateral ankle dorsiflexors and big toe extensors, more severe in right side.

Fig. 2
The graphs show that compound muscle action potentials of both common peroneal nerves recorded at extensor digitorum brevis.
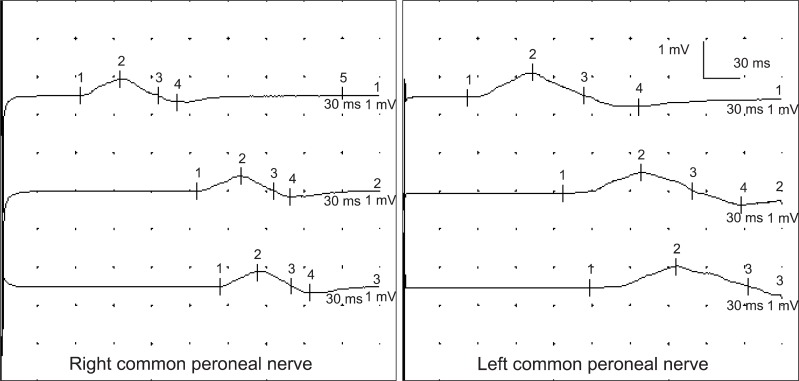
Fig. 3
The graphs show that sensory nerve action potentials of both superficial peroneal nerves were absent.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download