1. Jablecki CK, Andary MT, Floeter MK, Miller RG, Qartly CA, Vennix MJ, Wilson JR. Practice parameter: electrodiagnostic studies in carpal tunnel syndrome. Report of the American Association of Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2002; 58:1589–1592. PMID:
12058083.

2. Buchberger W, Schon G, Strasser K, Jungwirth W. High-resolution ultrasonography of the carpal tunnel. J Ultrasound Med. 1991; 10:531–537. PMID:
1942218.

3. Wong SM, Griffith JF, Hui AC, Lo SK, Fu M, Wong KS. Carpal tunnel syndrome: diagnostic usefulness of sonography. Radiology. 2004; 232:93–99. PMID:
15155897.

4. Yoon JS, Kim BJ, Kim SJ, Kim JM, Sim KH, Hong SJ, Walker FO, Cartwright MS. Ultrasonographic measurements in cubital tunnel syndrome. Muscle Nerve. 2007; 36:853–855. PMID:
17879384.

5. Yoon JS, Walker FO, Cartwright MS. Ultrasonographic swelling ratio in the diagnosis of ulnar neuropathy at the elbow. Muscle Nerve. 2008; 38:1231–1235. PMID:
18785184.

6. Tuncali D, Barutcu AY, Terzioglu A, Aslan G. Carpal tunnel syndrome: comparison of intraoperative structural changes with clinical and electrodiagnostic severity. Br J Plast Surg. 2005; 58:1136–1142. PMID:
16054604.

7. Hammer HB, Hovden IA, Haavardsholm EA, Kvien TK. Ultrasonography shows increased cross-sectional area of the median nerve in patients with arthritis and carpal tunnel syndrome. Rheumatology (Oxford). 2006; 45:584–588. PMID:
16332951.

8. Beekman R, Visser LH. Sonography in the diagnosis of carpal tunnel syndrome: a critical review of the literature. Muscle Nerve. 2003; 27:26–33. PMID:
12508291.

9. Peeters EY, Nieboer KH, Osteaux MM. Sonography of the normal ulnar nerve at Guyon's canal and of the common peroneal nerve dorsal to the fibular head. J Clin Ultrasound. 2004; 32:375–380. PMID:
15372443.

10. Cartwright MS, Shin HW, Passmore LV, Walker FO. Ultrasonographic findings of the normal ulnar nerve in adults. Arch Phys Med Rehabil. 2007; 88:394–396. PMID:
17321837.

11. Martinoli C, Schenone A, Bianchi S, Mandich P, Caponetto C, Abbruzzese M, Derchi LE. Sonography of the median nerve in Charcot-Marie-Tooth disease. AJR Am J Roentgenol. 2002; 178:1553–1556. PMID:
12034637.

12. Cho JM, Yoon JS, Kim SJ, Park BK, Lee GH, Jeong JS. Feasibility of ultrasonographic area ratio of median nerve in the diagnosis of carpal tunnel syndrome in Korea. J Korean Acad Rehabil Med. 2009; 33:627–631.
13. Cartwright MS, Shin HW, Walker FO. Ultrasonographic characteristics of the normal median nerve. Neurology. 2006; 66(Suppl 2):A83.
14. Hobson-Webb LD, Massey JM, Juel VC, Sanders DB. The ultrasonographic wrist-to-forearm median nerve area ratio in carpal tunnel syndrome. Clin Neurophysiol. 2008; 119:1353–1357. PMID:
18387336.

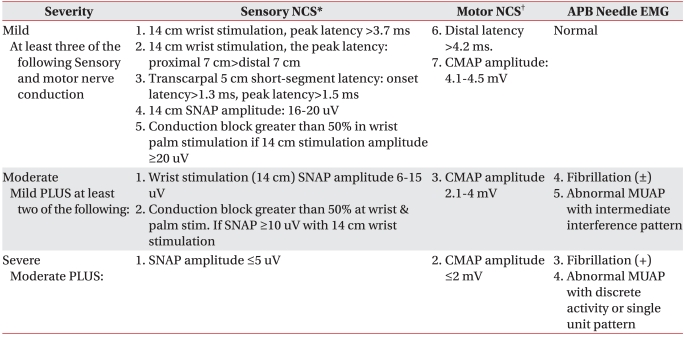
15. American Association of Electrodiagnostic Medicine. Guidelines in electrodiagnostic medicine. Practice parameter for electrodiagnostic studies in carpal tunnel syndrome. Muscle Nerve Suppl. 1999; 8:S141–S167. PMID:
16921633.
16. Bland JD. A neurophysiological grading scale for carpal tunnel syndrome. Muscle Nerve. 2000; 23:1280–1283. PMID:
10918269.

17. Giannini F, Cioni R, Mondelli M, Padua R, Gregori B, D'Amico P, Padua L. A new clinical scale of carpal tunnel syndrome: validation of the measurement and clinical-neurophysiological assessment. Clin Neurophysiol. 2002; 113:71–77. PMID:
11801427.

18. Padua L. A new approach to carpal tunnel syndrome: multicenter studies with multiperspective assessment. AAEM Course H. 2003. 2003 Sep 16-20; San Francisco, USA. Rochester: American Association of Electrodiagnostic Medicine.
19. Stevens JC. AAEM minimonograph #26: the electrodiagnosis of carpal tunnel syndrome American Association of Electrodiagnostic Medicine. Muscle Nerve. 1997; 20:1477–1486. PMID:
9390659.
20. Wee AS. Carpal tunnel syndrome: a system for categorizing and grading electrophysiologic abnormalities. Electromyogr Clin Neurophysiol. 2001; 41:281–288. PMID:
11572189.
21. El Miedany YM, Aty SA, Ashour S. Ultrasonography versus nerve conduction study in patients with carpal tunnel syndrome: substantive or complementary tests? Rheumatology (Oxford). 2004; 43:887–895. PMID:
15100417.

22. Lee HJ, Kwon HK. Electrophysiologic classification of severity of carpal tunnel syndrome. J Korean Assoc EMG-Electrodiagn Med. 2004; 6:1–3.
23. Cho YS, Lee SH, Kwon HK, Lee HJ. Reappraisal of nerve conduction studies in carpal tunnel syndrome. J Korean Acad Rehabil Med. 1998; 22:861–865.
24. Kotevoglu N, Gulbahce-Saglam S. Ultrasound imaging in the diagnosis of carpal tunnel syndrome and its relevance to clinical evaluation. Joint Bone Spine. 2005; 72:142–145. PMID:
15797494.

25. Buchberger W, Judmaier W, Birbamer G, Lener M, Schmidauer C. Carpal tunnel syndrome: diagnosis with high-resolution sonography. AJR Am J Roentgenol. 1992; 159:793–798. PMID:
1529845.

26. Lee CH, Kim TK, Yoon ES, Dhong ES. Correlation of high-resolution ultrasonographic findings with the clinical symptoms and electrodiagnostic data in carpal tunnel syndrome. Ann Plast Surg. 2005; 54:20–23. PMID:
15613877.

27. Bayrak IK, Bayrak AO, Tilki HE, Nural MS, Sunter T. Ultrasonography in carpal tunnel syndrome: comparison with electrophysiological stage and motor unit number estimate. Muscle Nerve. 2007; 35:344–348. PMID:
17143879.

28. Padua L, Pazzaglia C, Caliandro P, Granata G, Foschini M, Briani C, Martinoli C. Carpal tunnel syndrome: ultrasound, neurophysiology, clinical and patient-oriented assessment. Clin Neurophysiol. 2008; 119:2064–2069. PMID:
18620908.

29. Park JY, Park SR, Lee SH, Choi KH. The ultrasonographic findings of the median nerve in the carpal tunnel according to age and sex of normal Korean adults. J Korean Acad Rehabil Med. 2008; 32:564–569.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download