Abstract
Method
A retrospective study was done in 864 patients with contact burns who discharged from our hospital from January 2005 to December 2008. The following parameters were compared between patients with contact burns from therapeutic modalities and from other causes: general characteristics, burn extent, cause of burn injury, place of occurrence, burn injury site, treatment methods, prevalence of underlying disease, and length of hospital stay were compared between patients with contact burns.
Results
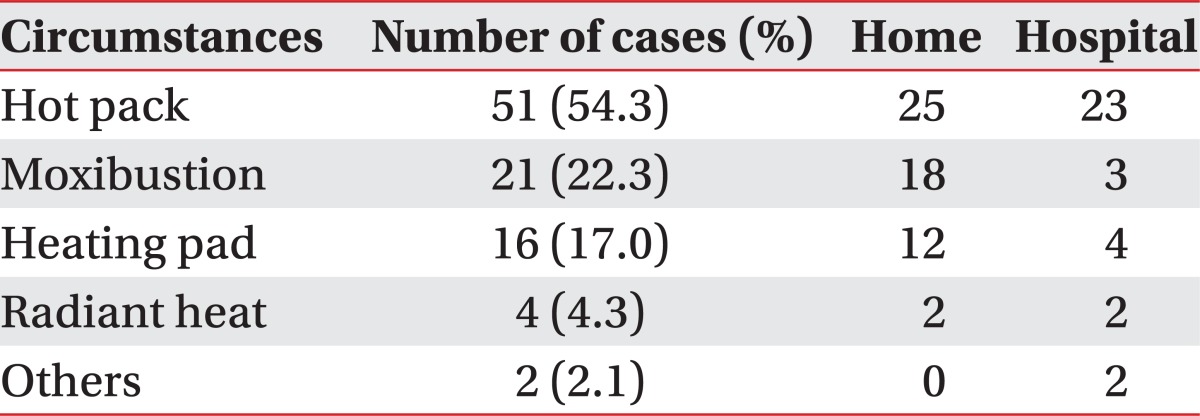
Of the 864 subjects, 94 patients were injured from therapeutic modalities. A hot pack (n=51) was the most common type of therapeutic modality causing contact burn followed by moxibustion (n=21), electric heating pad (n=16), and radiant heat (n=4). The lower leg (n=31) was the most common injury site followed by the foot & ankle (n=24), buttock & coccyx (n=9), knee (n=8), trunk (n=8), back (n=6), shoulder (n=4), and arm (n=4). Diabetes mellitus was associated with contact burns from therapeutic modalities; the odds ratio was 3.99. Injuries took place most commonly at home (n=56), followed by the hospital (n=33), and in other places (n=5).
Conclusion
A hot pack was the most common cause of contact burns from therapeutic modalities, and the lower leg was the most common injury site. Injuries took place most commonly at home. The patients with contact burns from therapeutic modalities showed high correlation to presence of diabetes mellitus. These results would be helpful for the prevention of contact burns due to therapeutic modalities.
Go to : 
The physical therapy or physiotherapy refers to activities using heat, cold ice, electricity, electromagnetic wave, or ultrasonic wave, for rehabilitational therapeutic efficacies with specific goals, such as relieving pain, facilitating healing, and improving body movement.1 Heat therapy, among them, is used for relieving general pains, relaxing of muscle spasm by physiological effect of heat, and in the case of joint stiffness and joint contracture, is used in combination with therapeutic exercise. This modality is especially helpful for treatment of musculoskeletal diseases and is commonly used in the hospital and at home.
The hot pack is a most widely used equipment in heat therapy due to its advantages, such as low cost and long period of use; however, it has to be used carefully for individuals with dysesthesia because of the risk of burns.2 It is known that a burn is most frequent side effect of moxibustion, a therapeutic modality used in folk remedies and in Oriental medicine as a heat stimulation on a certain site.3
It is reported that approximately 1,500 patients with burn injury from electric heating pad are treated in emergency room in the United States and an average of 8 deaths per year are associated with the use of heating pads.4 It is also relatively common in our country to visit hospitals with contact burns from therapeutic physical modality. Concerning this issue, Nam et al.5 reported on a case study and Song et al.6 noted the hot pack and moxibustion as causes of contact burns. According to Song et al.,6 402 of 4,321 patients with burn injuries were contact burns and the causes were hot pack (n=45, 11.2%) and moxibustion (n=27, 6.7%). These studies, however, have limits of focusing on heat therapy only, as a cause of contact burn injury. The purpose of this study was, therefore, to investigate the damage pattern of contact burns from physical therapeutic modalities, to analyze associated factors of them, and to propose preventive measures.
Go to : 
Of 7,817 hospitalized patients with burn injuries in our center from Jan 2005 to Dec 2008, 864 occurrences (11.1%) were from contact burns. The medical records of 94 events, among them, from physical therapeutic modality were analyzed retrospectively; the prevalences of diabetes mellitus, hypertension, alcoholism, and disability were analyzed, and the presence of diabetic neuropathy, associated factors, including duration of diabetes mellitus and blood HbA1C, were compared with that of 770 patients from other causes than physical therapeutic modalities. The electrodiagnostic examination for diabetic neuropathy was performed only with 7 patients because of acute treatment of contact burns and decreased general conditions. The number of operations and hospitalhospitalization periods of each physical therapeutic modality was analyzed as well. The additional phone questionnaires were administered to the survey treatment process and the method for the contact burns from physical therapeutic modalities; for the 64 survey responses, the period of physical therapy, prescription and indication of the physician before therapy, cause of burn injury, and cause of therapy were surveyed. The contact burn injury from the hot pack was defined as those from a hydrocollator pack used in hospital and keeping its temperature using water and from commercially available disposable hot packs used at home. The burns caused by hot towels and Ondol (heated stone) were excluded. Contact burn injuries from electric heating pad was defined as those that resulted from heating pad in which the heating amounts are controlled by electric currents, and burn injuries from electric mattress were not included.
The frequency analysis for general characteristics was performed against the collected data, using SPSS 18.0 program (SPSS Inc., Chicago, USA). The univariate analyses were tested using independent samples t-test and chi square test; multivariate logistic regression analysis was performed for the variables whose p-values were under 0.05. The Mann-Whitney U test was performed to compare the duration of diabetes mellitus and blood HbA1C level of patients with diabetes mellitus groups in those with contact burn injuries between occurrences from physical therapeutic modalities and from other causes. Treatment method and hospitalization period, by presence of diabetes mellitus and types of physical therapy, were compared using the Mann-Whitney U test and the Kruskal-Wallis test. A p-value under 0.05 was considered statistically significant.
Go to : 
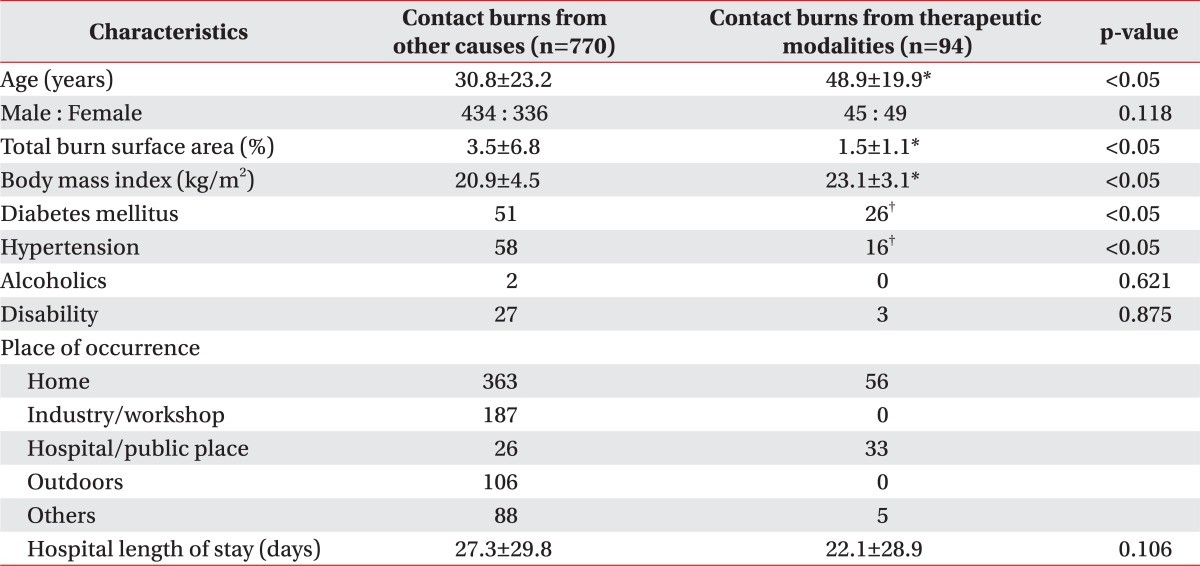
Of 94 patients, the average age was 47.5±19.7 for males (n=45) and 50.3±20.2 for females (n=49). The average burn surface area was 1.5±1.1%. The patients with contact burn injuries from physical therapeutic modalities (PT group) were statistically significantly older and had higher mean body mass index (BMI) than those that occurred from other causes (nPT group). The prevalence of diabetes mellitus was also statistically significantly higher in PT group. It was shown that the alcoholism and disabilities had no effect on the prevalence of contact burn injuries from physical therapeutic modalities. The home (n=56) was the most common place in which burn accidents occurred, followed by the clinic, hospital, and oriental medical clinic (n=33), and other sites (n=5) (Table 1).
The hot pack was most common cause of burn injury from physical therapeutic modalities and followed by moxibustion and electric heating pad. The most common place where contract burn injury occurred was home for ones from moxibustion and electric heating pad, and whereas was hospital (47.9%) for ones from hot pack (Table 2).
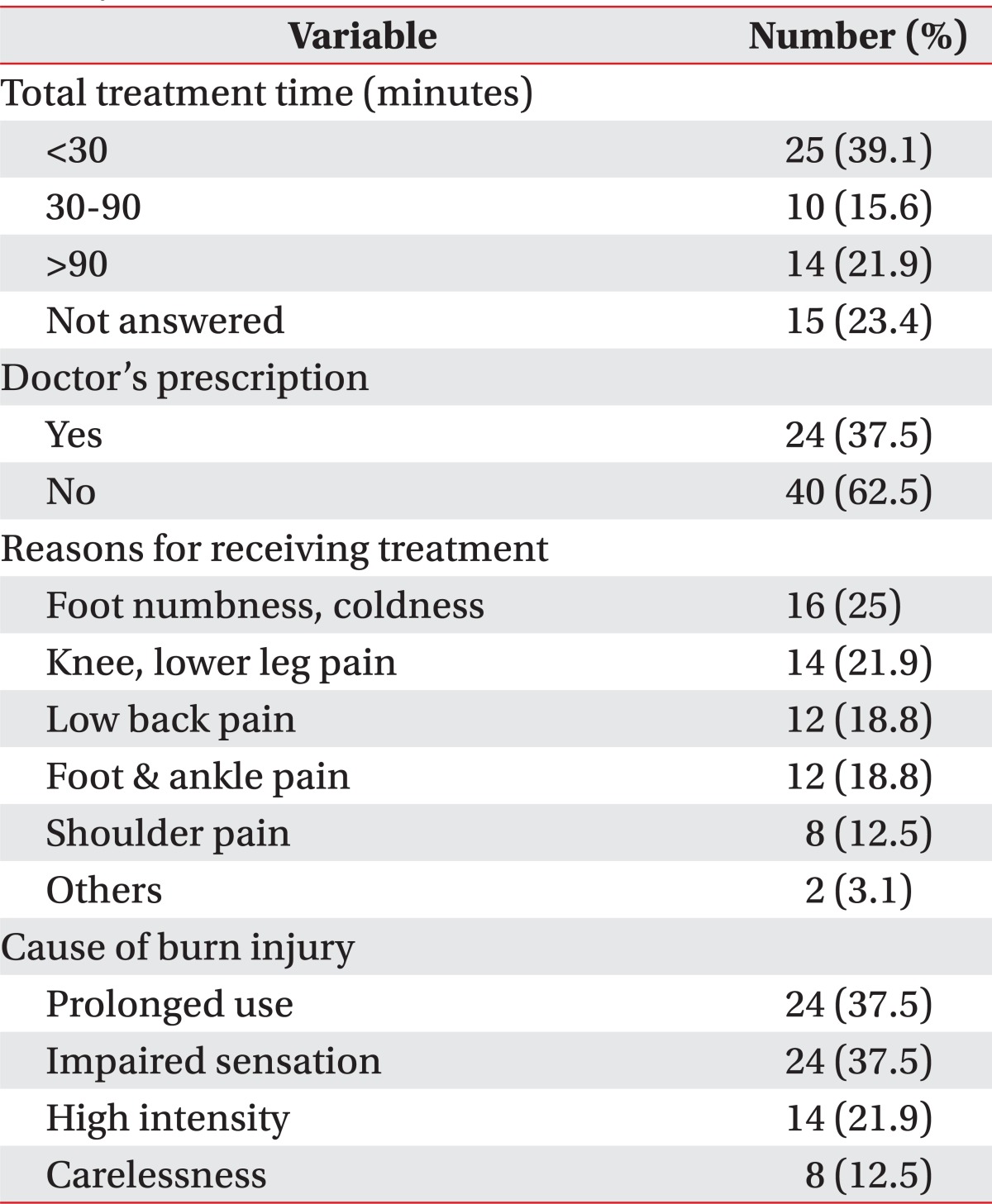
For the application time of physical therapeutic modalities, 39.1% were under 30 min and 30 minutes and over was 37.5% (not answered 23.4%). Of the 64 responses, the 24 patients received prescription or indication from doctor for physical therapeutic modalities and others didn't any indication and performed physical therapy on their voluntary choice. The main complaints for treatment were pain of the back, shoulders, knees, and ankles, and musculoskeletal diseases such as joint contracture for 48 patients, and were leg numbness and coldness for 16 patients. The 16 patients all had underlying diseases, such as diabetes mellitus, hemiplegia from stroke, or peripheral vascular disease. The perceived causes of burn injuries for patients were prolonged physical therapy (n=24), impaired sensation of affected sites (n=24), excessively high intensity of physical therapy (n=14), and careless use (n=8), including lying down on heating pad, extraction of hot pack contents, heated iron parts of rubber heating pack (Table 3).
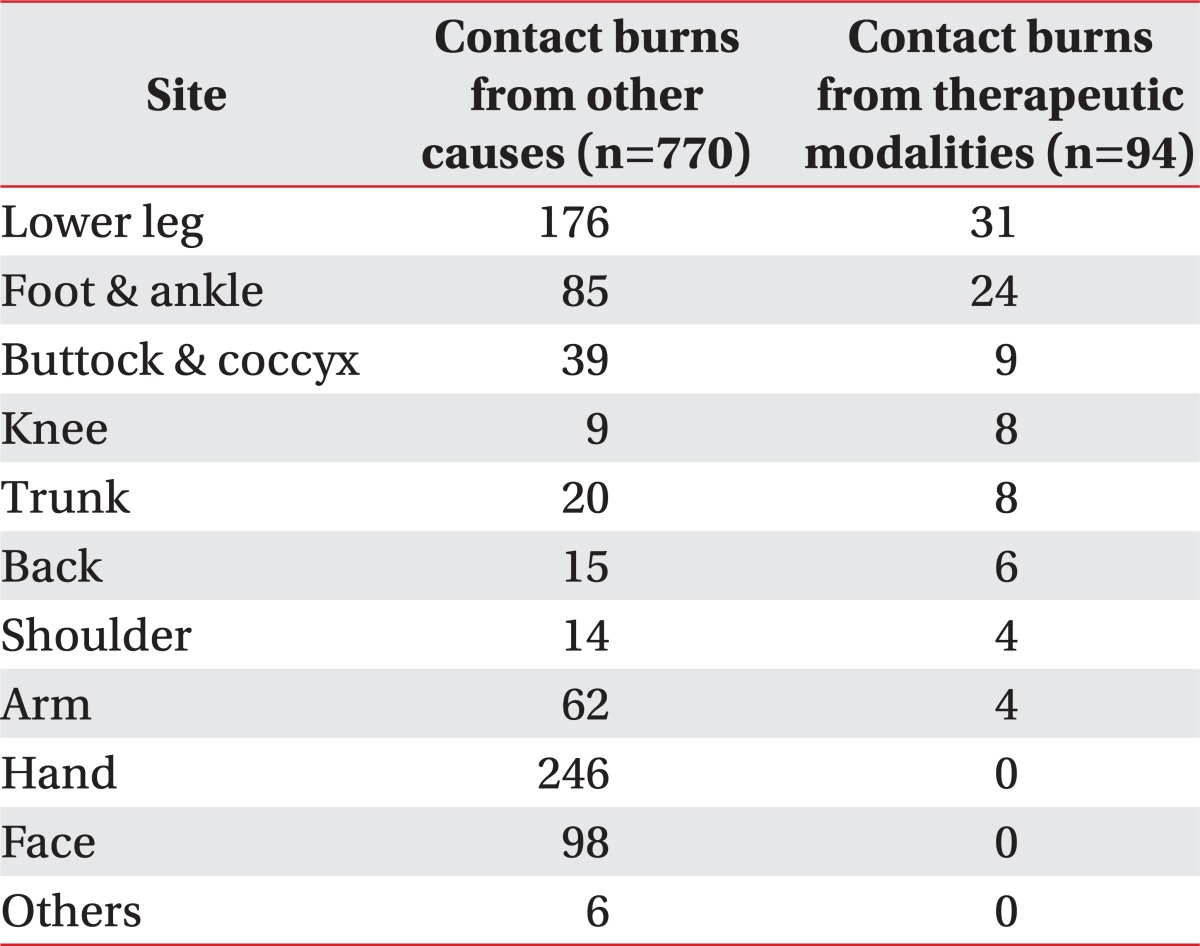
The most frequent burn injury site was the lower leg, followed by the foot & ankle, buttock, coccyx site, knee, trunk, back, shoulder, and upper arm; for patients with causes other than physical therapeutic modalities, it was the hand and followed by leg, face, foot & ankle and upper arm (Table 4). The most frequently used treatment method was split thickness skin graft (n=60), followed by conservative treatment (n=20), flap (n=5), and full thickness skin graft (n=3).
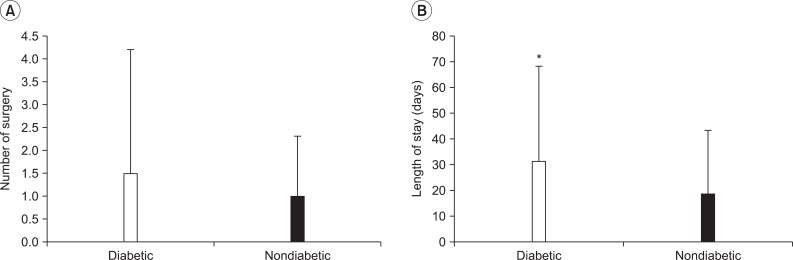
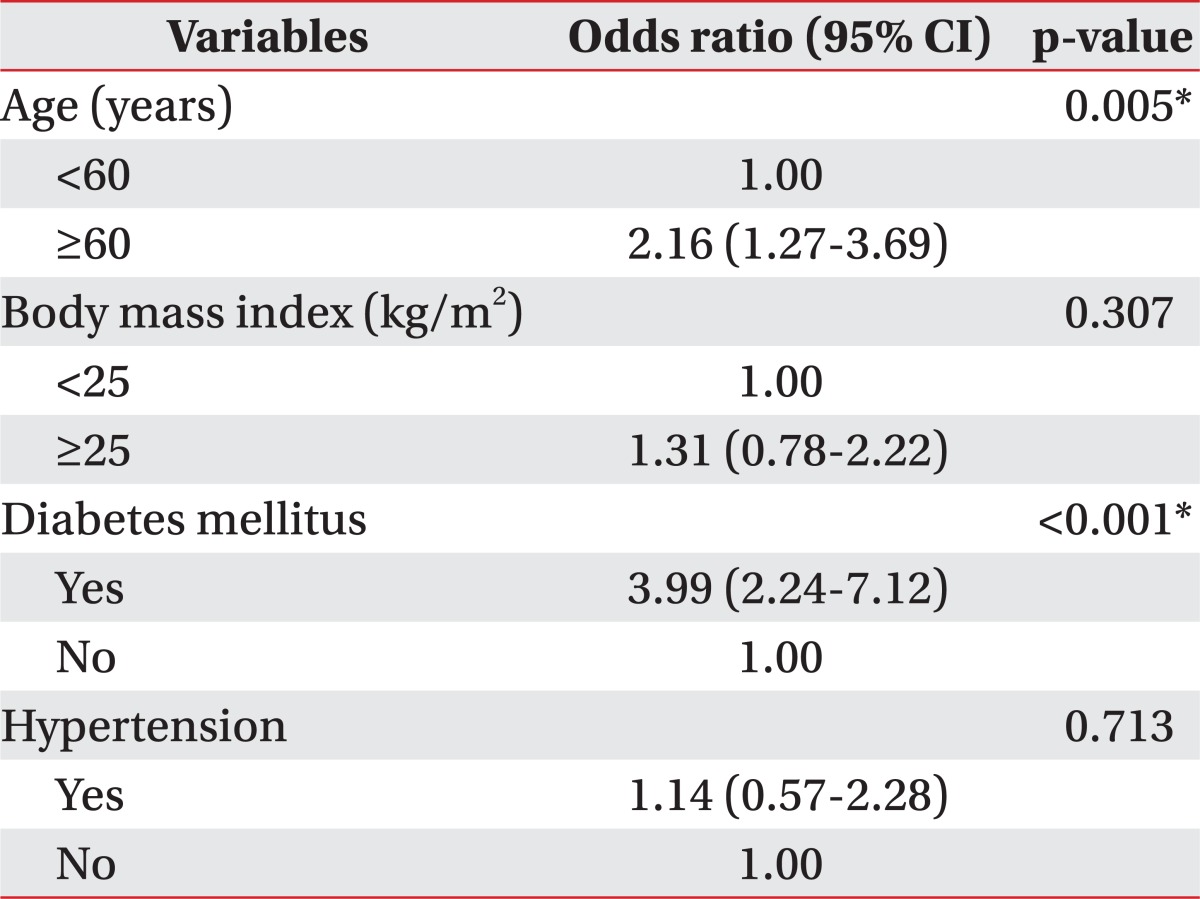
The univariate analysis showed that age, BMI, diabetes mellitus, and hypertension were significant variables. The multivariate logistic regression analysis was performed on the significant variables and age and diabetes mellitus were shown to be statistically significant (Table 5). For the PT group, the analysis of the difference in number of operation and hospitalization day, between patients with and without diabetes mellitus, showed that the number of operations had no significant difference but the hospitalization period increased significantly in subgroups with diabetes mellitus (p<0.05) (Fig. 1). There were no significant differences in the number of operations and the hospitalization period among the type of physical therapeutic modalities.
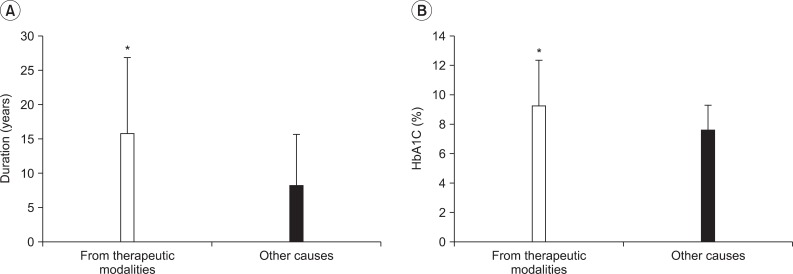
The average duration of diabetes mellitus of 26 patients with diabetes mellitus in PT group was 15.8±11.1 years, a significantly longer period than that (8.1±7.6 years) of 51 counterparts in nPT group (p<0.05). The average concentration of blood HbA1c of patients with diabetes mellitus in PT group was 9.3±3.1%, a significantly higher than that (7.6±1.7%) of 51 counterparts in the nPT group (p<0.05) (Fig. 2). The 7 patients available in electrodiagnostic examination were diagnosed with diabetic neuropathy.
Go to : 
The doctor, before prescribing physical therapy, investigate detail clinical history and general condition, assess functional ability, including physical examination and radiological findings, so that make medical judge synthetically, considering consciousness state, cognitive ability, anatomic structure, level of pain, disease period, temperature sensation, and sense of pain on damaged site of patients. The heat therapy, among them, is frequently used for treating various musculoskeletal diseases. The general contraindications for this treatment method include patients with dysesthesia or site of impaired sensation, site undergone recently or of high risk for hemorrhage, site of malignant tumor, acute inflammation, external wound, or edema, and patients with low cognitive ability.7 The hot pack is most frequent cause of burn injury from physical therapeutic modality because it has sedative effects and rarely performed under medical staff. In addition, when the patients lie on hot pack the exudated water wet the towel increase the heat conductivity and the local pressure is generated, resulting in increasing risk for burn injury. Similarly, the risk for burn injury increase also in case of using electric heating pad, especially more carefulness is required when the patients are lean or cachectic because the site with protruded bone has thin layers of fat.7
This study attempted to investigate clinical factors associated with contact burn injury, a complication common during physical therapeutic modalities. The 94 patients hospitalized in our center were analyzed and it was shown that the hot pack is most common cause of contact burn and followed by moxibustion, electric heating pad, electric stimulation, and moxa cautery. According to Song et al.,6 the hot pack and moxibustion were the most common cause of contact burn in the data covering 12 years, occupying 11.2% and 6.7%, respectively, in agreement with the results of this study. Nadler et al.4 reported, in the study about complications from physical therapeutic modalities among 905 athletic trainers, that 233 ones experienced complications from physical therapeutic modalities and that the most common causes were heat therapy (n=41), electric therapy (n=40) and cryotherapy (n=23). Bill et al.8 reported, in his case study, two cases in which patients with dysesthesia each due to congenital spina bifida and diabetes mellitus got burn injuries from electric heating pad, and Satter9 reported a case of third degree burn injury from interferential current therapy. In addition, Balmaseda et al.10 reported two cases of contact burn injuries from electric stimulation treatment and Ford et al.11 reported a case of burn injury after interferential current therapy for treating pain after total knee replacement arthroplasty. Nam et al.5 reported keloid after burn injury from moxibustion.
The hot pack, a superficial heat treatment, is best known conduction heat treatment. During treatment using this method, the medical staff should check the sensation and the skin state of patients because the feeling of patient is only indicator of temperature. The electric heating pad, an frequent alternative superficial heat treatment of hot pack used at home and hospital, has also risk of burn injury, necessitating limited period of use.1 It is considered that the reason hot pack and heating pad is most common causes of contact burn injuries is that those are most general heat therapy at home and hospital and have high risk of burn injury when carelessly used. The moxibustion is known, in Oriental medicine, to have efficacies of treatment, relieving pain, recovery and prevention, to be applicable in wide range of disease, and to have no major complication, so it is broadly used in clinical setting by Oriental doctors; however, it has been likely to be performed by unlicensed doctor or patients themselves. According to Han et al.,3 the most common symptom among outpatients for side effects from moxibustion was a severe scar; the moxibustion was also the secondly most common cause of contact burn injury in this study.
In the study by Song et al.,6 the most common place burn injuries occurred was home (66.9%) and followed by workplace (11.8%), it is consistent with this study, results of which showed that the most common case is self-treatment at home (60.2%) and followed by hospital and clinic (34.4%). The most common place where contract burn injury occurred was home for ones from moxibustion and electric heating pad, and whereas was hospitals for ones from hot pack. It is speculated, for the reason of those results, that the learning and performance of moxibustion is relatively easy, therefore is likely to be performed by unlicensed practitioners or patients themselves carelessly. It needs, therefore, to use professional treatment approaches by correct diagnoses and procedure at hospital in order to prevent those undesired side effects. The electric heating pad can be used at home easily because, unlike hot pack treatment which is applied by therapist under prescription at hospital, it needs only electric connection using consent and simple switch manipulation for controlling intensity. It causes, however, many burn injuries probably because it is hard to do careful observation on affected site and it is common to neglect for long time, left lying on the floor. Therefore, it is recommended to apply for limited periods of time in using and to be careful not to sleep leaving body sites contacted with electric heating pad. It is also recommended to force the manufacturers to attach timer to prevent prolonged application of excessive heat, and to specify use cautions largely.
The direct cause of contact burn injuries were analyzed using data from patients available in administering phone questionnaires. It was shown that the 37.5% of them got burn injuries from physical therapy over 30 minutes. Given that the 20-30 minutes is proper application time in heat therapy such as hot pack,7 the prolonged application time may be the cause of burn injuries in those cases. It is recommended, therefore, to comply appropriate application time and to check skin state frequently. It is also shown that the 62.5% of the patients get burn injuries during self-treatment without doctor's prescriptions. This indicates that the incorrectly prescribed physical therapies can have significant damages to body. In addition, the 25% of patients reported that they get burn injuries during heat therapies for the foot numbness and coldness. Those patients were all confirmed to have underlying diseases such as diabetes mellitus, hemiplegia from stroke that may cause dysesthesia of foot, probably that information were not informed to medical staffs or there were no careful hearing of clinical history and examining general condition, nor physical examination which are necessary medical diagnosis steps for suitable prescription of physical therapies. It is, especially, important for patients with diabetes mellitus to inform patients with clinical manifestation and suitable treatment method in order to prevent burn injuries from above careless performance of heat therapy, because, in that group, the chance of developing diabetic neuropathy increases with the length of disease period. The facts that patients perceived careless use as most common cause of burn injuries indicates that it is important for therapists and patients to have correct knowledge about physical therapy and use them properly.
The most common burn injury site was lower limbs (67.7%) including foot, knee joint and followed by buttock and trunk, the arms was the less frequent site. The hands are the medium allowing us to interact with environments, and arms are the most frequent morbid site.12 According to Kim and Na13 the sites where the burn injuries occurred mostly were hands (29%) and lower limbs (21.3%). The reason for the significant dominance of lower limbs burn injuries in this study is speculated that the dysesthesia due to diabetic neuropathy is more severe on lower limbs than other body parts, and the numbness and pains make patients to seek physical therapies. The fact that is harder for patients to observe lower limbs than upper body may be another reason. Notably, the results of this study may be affected by selection bias because this study, unlike Kim and Na,13 which included outpatients and private hospital patients with burn injuries based on data from National Health Insurance Corporation, included only patients with burn injuries hospitalized at our center.
The prevalence of diabetes mellitus in PT group was higher by 3.99 times than that in nPT group, indicating that the patients with diabetes mellitus is likely not to sense high temperature despite the prolonged heating, due to their dysesthesia from diabetic neuropathies. The severities of seven patients available in electrodiagnostic examination, measured by the modified version of electromyographic findings from The Diabetes Control and Complications Trial (DCCT)14 were suspected group for three patients, probable group for two patients, and definite group for two patients. Although those who diagnosed with diabetic neuropathy were only seven, comparing the patients with diabetes mellitus in nPT group, they had longer disease period and higher concentration of blood HbA1C, resulting in higher chance of developing peripheral neuropathy.15 It is also problematic, in other hands, that patients with diabetes mellitus are likely to complain pains and dysesthesia, resulting in more prescription of physical therapeutic modalities. It needs, therefore, to be more careful in applying physical therapy to patients with diabetes mellitus, and it is considered that it is helpful in preventing contact burn injuries from physical therapy to inform patients with diabetes mellitus to inform them clinical manifestation and suitable treatment method and related information.
The hospitalization period of patient with diabetic mellitus, in this study, was significantly longer than one without the disease, this is consistent with the results of Schwartz et al.16 showing that the patients with diabetic mellitus had higher infection rate, occurrence of complication from graft and longer hospitalization period compared to patients without the disease.
The limitation of this study is that the patients with burn injuries of minor severities were not included because patients were restricted to ones hospitalized at our center. It is considered, therefore, to plan wider scope of study in future.
Go to : 
The most common cause of contact burn injuries from physical therapeutic modalities was a hot pack, followed by moxibustion and electric heating pad. The burn injuries occurred most commonly at home, although the hospital was another place where therapeutic burns occurred frequently. Many patients experienced burn injuries during self-treatment without the prescription or diagnosis by a doctor. The prolonged application time, application on sites of dysesthesia, and carelessness were the direct causes. The most common site on which burn injuries occurred was the lower limbs, including the foot. The patients in the PT group were older and had higher prevalence of diabetes mellitus compared to ones in nPT group. Patients with diabetes mellitus stayed longer in the hospital than those patients without the disease. The results showed that it is important to consider temperature and pain sensation of the affected sites based on the careful taking of clinical histories and physical examination before prescribing physical therapeutic modalities and to provide patients with dysesthesia, such as diabetic neuropathy, and sufficient information about the hazards of heat therapy in order to prevent contact burn injuries from physical therapeutic modalities.
Go to : 
References
1. Han TR, Bang MS. Rehabilitation medicine. 2008. 3rd ed. Seoul: Kunja Publishing Co.;p. 159–161.
2. Basford JR. Delisa JA, Gans BM, Walsh NE, editors. Therapeutic physical agents. Physical medicine and rehabilitation: principles and practice. 2005. 4th ed. Philadelphia: Lippincott Williams & Wilkins;p. 252–253.
3. Han CH, Shin MS, Kang KW, Kang BK, Park SH, Choi SM. An in-depth interview for use of moxibustion therapy in Korea. Korean J Acupunct. 2008; 25:85–97.
4. Nadler SF, Prybicien M, Malanga GA, Sicher D. Complications from therapeutic modalities: results of national survey of athletic trainers. Arch Phys Med Rehabil. 2003; 84:849–853. PMID: 12808537.
5. Nam YH, Ko DH, Yoon TJ. A case of moxibustion-induced keloid. Korean J Dermatol. 2006; 44:1091–1093.
6. Song DS, Kim HC, Woo GW. A retrospective epidemiologic analysis of burn patients at Hanil Hospital. J Korean Burn Soc. 2009; 12:21–37.
7. Weber DC, Hoppe KM. Braddom RL, editor. Physical agent modalities. Physical medicine and rehabilitation. 2007. 3rd ed. Philadelphia: Saunders;p. 459–477.

8. Bill TJ, Edlich RF, Himel HN. Electric heating pad burns. J Emerg Med. 1994; 12:819–824. PMID: 7533807.

9. Satter EK. Third-degree burns incurred as a result of interferential current therapy. Am J Dermatopathol. 2008; 30:281–283. PMID: 18496434.

10. Balmaseda MT Jr, Fatehi MT, Koozekanani SH, Sheppard JS. Burns in functional electric stimulation: two case reports. Arch Phys Med Rehabil. 1987; 68:452–453. PMID: 3496867.
11. Ford KS, Shrader MW, Smith J, Mclean TJ, Dahm DL. Full-thickness burn formation after the use of electrical stimulation for rehabilitation of unicompartmental knee arthroplasty. J Arthroplasty. 2005; 20:950–953. PMID: 16230253.

12. Smith MA, Munster AM, Spence RJ. Burns of the hand and upper limb-a review. Burns. 1998; 24:493–505. PMID: 9776087.

13. Kim DC, Na DS. Epidemiology of burns in Korea. J Korean Burn Soc. 2011; 14:6–11.
14. The Diabetes Control and Complications Trial Research Group. The effect of intensive diabetes therapy on the development and progression of neuropathy. Ann Intern Med. 1995; 122:561–568. PMID: 7887548.
15. Park JM, An GY. Factors affecting diabetic neuropathy and significance of nerve conduction study. J Korean Acad Rehabil Med. 1993; 17:578–584.
16. Schwartz SB, Rothrock M, Barron-Vaya Y, Bendell C, Kamat A, Midgett M, Abshire J, Biebighauser K, Staiano-Coico LF, Yurt RW. Impact of diabetes on burn injury: preliminary results from prospective study. J Burn Care Res. 2011; 32:435–441. PMID: 21436717.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download