Abstract
Objective
To evaluate the effect of extracorporeal shock wave therapy (ESWT) in myofascial pain syndrome of upper trapezius with visual analogue scale (VAS) and pressure threshold by digital algometer.
Method
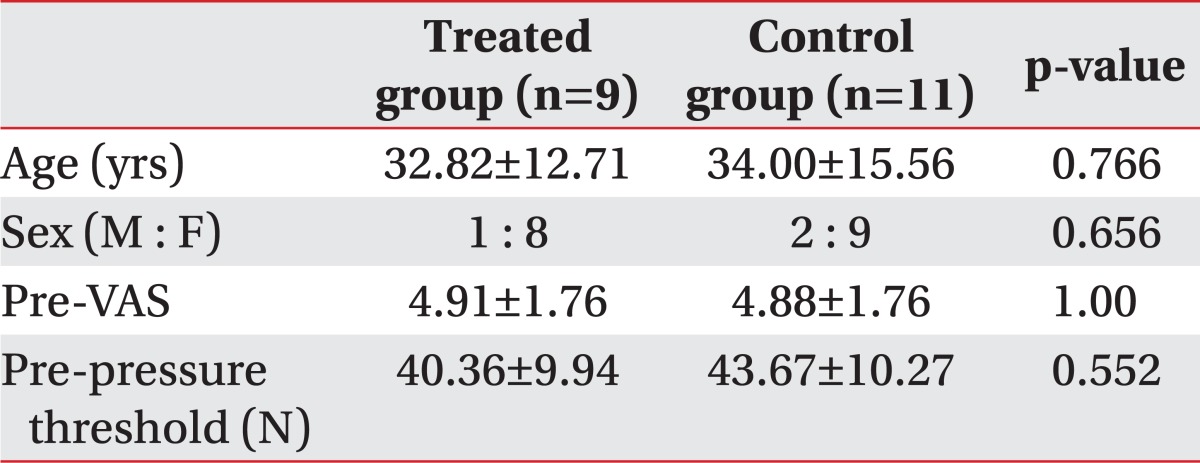
Twenty-two patients diagnosed with myofascial pain syndrome in upper trapezius were selected. They were assigned to treatment and standard care (control) groups balanced by age and sex, with eleven subjects in each group. The treated group had done four sessions of ESWT (0.056 mJ/mm2, 1,000 impulses, semiweekly) while the control group was treated by the same protocol but with different energy levels applied, 0.001 mJ/mm2. The VAS and pressure threshold were measured twice: before and after last therapy. We evaluated VAS of patients and measured the pressure threshold by using algometer.
Results
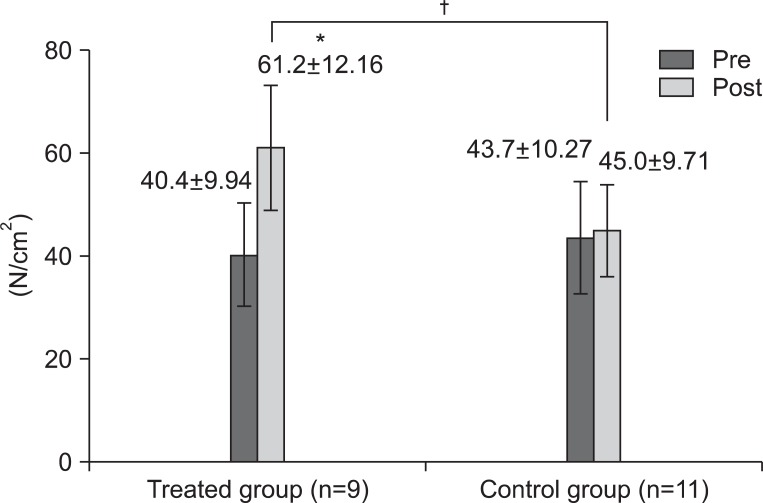
There were two withdrawals and the remaining 20 patients were three men and 17 women. Age was distributed with 11 patients in their twenties and 9 over 30 years old. There was no significant difference of age, sex, pre-VAS and pre-pressure threshold between 2 groups (p>0.05) found. The VAS significantly decreased from 4.91±1.76 to 2.27±1.27 in the treated group (p<0.01). The control group did not show any significant changes of VAS score. The pressure threshold significantly increased from 40.4±9.94 N to 61.2±12.16 N in the treated group (p<0.05), but there was no significant change in the control group.
Go to : 
Myofascial pain syndrome is represented by many clinical symptoms such as pain, hyperirritable nodule of spot tenderness, referred pain, muscle spasm by trigger points. The upper trapezius is probably the muscle most often beset by trigger points,1,2 and Fischer3 indicated that the upper trapezius is the most sensitive of 8 different muscles (upper trapezius, pectoralis major, leavator scapulae, teres major, supraspinatus, gluteus medius, infraspinatus, paraspinalis) to the pressure of an algometer. Although the pathophysiology of trigger point is not clear, Simons et al.4 assumed that the muscle fibers are shortened and taut bands are made by calcium influx in damaged fibers or acetylcholine secretion in motor end plates. The trigger points are the hyperirritable nodules of spot tenderness in a palpable taut band of skeletal muscle that may cause pain to a distant point and also causes distant motor and autonomic effects.
The treatments of myofascial pain are divided into the invasive and the non-invasive therapy. The invasive therapy is about the injection of medications, dry needling and non-invasive therapy refers to massage, stretching and ultrasound.4-10 Extracorporeal shock wave therapy (ESWT) is recently considered an effective treatment for myofascial pain syndrome. It's been proved an effective in musculoskeletal disease such as nonunion of pseudoarthrosis or fracture, calcific tenosynovitis, plantar fasciitis.11,12 Although the pathophysiology is not clear, the effectiveness of ESWT in myofascial pain syndrome has been studied. We thought this significant since it is a non-invasive and simple treatment, easy to apply at a large surface, and has fewer side effects with low intensity even if it requires relatively high cost.
With other diseases which are improved the effectiveness is thought to stem from promoting angiogenesis, increasing perfusion in ischemic tissues, decreasing inflammation, enhancing cell differentiation, accelerating wound healing and alleviation of pain by altering pain signal.13-18 Considering these pathophysiologies, we hypothesized that ESWT could reduce the pain of myofascial pain syndrome by pain signal alteration, promoting angiogenesis and increasing perfusion in ischemic tissues induced by sensitization of nociceptors and muscle ischemia. The purpose of this study is to find a reducing effect of ESWT with visual analogue scale (VAS) and pressure threshold in myofascial pain syndrome of upper trapezius.
Go to : 
Twenty-two patients who suffered from shoulder pain are recruited, and they are diagnosed with typical myofascial pain syndrome based on Simon's criteria19 when they show a referred pain with a limitation of motion and pain with a nodule of taut bands.
We excluded patients who had medication or other therapies for myofascial pain syndrome, neurological deficits involving the upper limbs, advance osteopathic or arthropathic disorders of the cervical spine or the shoulder of the investigated side and contraindication of ESWT14,15 such as children, hypertension, coagulopathy, ulcer, recent severe hemorrhage, neoplasm, renal insufficiency, severe hepatic disease, epilepsy, cutaneous pathology, central pain and mental retardation.
The ESWT was applied by using a Dornier AR2® (MedTech, Munchen, German). This study was single-blind study and the participants were randomly assigned by treated group or control group. One doctor examined the taut band of one side upper trapezius and applied ESWT for 700 impulses to the taut band and 300 impulses surrounding the taut band. The treated group had 0.056 mJ/mm2 applied as low energy while the control group was applied 0.001 mJ/mm2, an ineffective level of ESWT, but can keep the participants blinded to their treatment by the sound of shock. There were 4 treatments sessions: 2 sessions per week in 2 weeks and no other treatment of myofascial pain syndrome such as medication, physical therapy and exercise.
A level of shoulder pain has been measured by a pressure threshold and VAS, done twice in total: before the initial treatment and right after the 4th treatment.
(1) pressure threshold: One examiner estimated pressure threshold by a digital algometer, OE-220® (ITO., Tokyo, Japan). The patients were asked to lie down in a prone position and were measured for the pressure threshold with a 1 cm-wide disk applied to the trigger point of upper trapezius perpendicularly per 1 N of the pressure increased. Before the examination, an examiner asked participants to say 'stop' when they feel pain or any uncomfortable feeling from the pressure and the pressure was noted when they say 'stop'. This procedure was performed 3 times with 10-seconds intervals, and the average was determined as pain threshold.
(2) Visual analogue scale (VAS): To evaluate pain intensity, the VAS was explained to the participants, that a 10 score is maximum pain that cannot be endured, and 0 score is no pain, and to express the score on the 10 cm line at the pressure threshold. An examiner asked participants to rate their pain at the pressure threshold as 10 point for the max which they cannot endure and 0 point for no pain. They were also asked to indicate their pressure threshold pain on 10 cm line.
All statistical analysis was analyzed by SPSS statistical software, version 15.0 (SPSS Inc., Chicago, USA). Mann-Whitney test was used to compare the characteristics and results between treated group and control group. Wilcoxon Signed Ranks test was performed to determine the effect of therapy in each group. Null hypotheses of no difference were rejected if p-values were less than 0.05.
Go to : 
Only 20 out of 22 participants were studied since 1 man and 1 woman in treatment group dropped due to geographic accessibility problem. There was no withdrawal due to side-effects of therapy. The participants 3 men and 17 women, the age ranged from 25 years to 74 years, and mean age was 33.35±12.25 years old. The mean age of treated group was 32.82±12.71 years old and control group was 34.00±15.56 years old. The treated group was 1 man and 8 women whereas the control group was 2 men and 9 women, and no significant difference found between groups in age and sex. The VAS tested before the therapy (pre-VAS) was 4.91±1.76 in treated group, 4.88±1.76 in control group, and the pressure threshold tested before the therapy (pre-pressure threshold) was 40.36±9.94 N in treated group, 43.67±10.27 N in control group. There is no significant difference of pre-VAS and pre-threshold between two groups (Table 1).
When we compare the VAS before and after the therapy, pre-VAS was 4.91±1.76 for treated group and 4.89±1.76 for control group, no significant difference between groups. However, post-VAS was 2.27±1.27 for the treated group and 4.44±2.13 for control group, a significant difference (p<0.05) (Fig. 1). The pressure threshold was 40.4±9.94 for treated group and 43.7±10.27 for control group before the therapy (pre-pressure threshold). We observed 61.2±12.16 N for treated group and 45.0±9.17 N for control group after therapy (post-pressure threshold), again a significant difference (p<0.05) (Fig. 2). When we compare pre-VAS and post-VAS within each group, VAS in the control group was 4.89±1.76 and changed to 4.44±2.13 after therapy while the VAS in the treated group was fell significantly from 4.91±1.76 to 2.27±1.27 after therapy (p<0.05) (Fig. 1). A pressure threshold in control group changed from 43.7±10.27 N to 45.0±9.17 N while it rose significantly from 40.4±9.94 N to 61.2±12.16 N in the treated group (p<0.05) (Fig. 2).
Go to : 
In this study, we compared the VAS and pressure threshold before and after 4 therapies, finding a significant difference between groups after therapy and no difference before therapy. Pre-post comparisons show VAS drops and pressure threshold increases in the treated group only.
The study of effect of ESWT in myofascial pain syndrome has been very limited. From a study which administered 7.3 treatments on average (1-2/week) with 800-1,000 impulses, 6 Hz and 0.04-0.26 mJ/mm2, we found that VAS decreased after three months of treatment.11 The study of ESWT using the electrohydraulic effect was uncontrolled and unblinded.12 The VAS score decreased 26% after the first therapy, and 58.5%, 67%, 85% after 2, 3, 4th therapy respectively. This study also shows decreased VAS and increased pressure threshold significantly after ESWT in myofascial pain syndrome of upper trapezius. It is significant as the first controlled, single blind and randomized study, and as the first study designed to apply constant energy and intensity of extracorporeal shock wave during regular duration. In addition, pressure thresholds are objectively evaluated by using an algometer, in contrast to previous studies.11,12 In this study, we used the electromagnetic effect with a cylindrical coil arrangement of an electromagnetic generator and a parabolic reflector to focus the shock waves, whereas previous studies used piezoelectric or electrohydraulic effect. Although it has the benefit of stable shock wave generation to the focal tissues, its energy is low and we used low energy, 0.056 mJ/mm2.
In this study, the treated group received extracorporeal shock wave for 4 sessions of treatments; 2 sessions per week in 2 weeks, 0.056 mJ/mm2, 700 impulses at taut band and 300 impulses at surroundings of taut band. It was designed on the basis of a previous study by Müller-Ehrenberg and Licht,11 in which participants were treated for 1-2 sessions per week, mean 7.3 sessions, 0.04-0.26 mJ/mm2 and 800-1,000 impulses at each taut band, resulting in significant change for reducing pain. Especially, this study applied low energy intensity. There is no need for local anesthesia because of less pain, and less side effects such as inflammation, tendon rupture, vessel injuries than high energy therapy.20 Also patient participation and compliance of participants are improved.
The pathophysiology of ESWT in myofascial pain syndrome is not clear so far. The myofascial pain syndrome is hypothesized to stem from an abnormal increase in the production and release of acetylcholine induce sustained depolarization of the postjunctional membrane of the muscle fiber, possibly causing a continuous release and uptake of calcium ion, producing muscle ischemia as a result of sustained shortening of sarcomeres and release of sensitizing substances (substance P, bradykinin, calcitonin gene-related peptide, TNF a, IL-1B, IL-6, IL-8). Through this pathophysiology, the vicious cycle is completed when the nociceptors are sensitized and the muscle ischemia is aggravated.17,21 Considering for the pathophysiology of extracorporeal shockwave therapy in other diseases,13-16,18 we thought that ESWT can promote angiogenesis, increase perfusion, and alter the pain signaling at ischemic tissues caused by calcium influx.
This study cannot be generalized for all age and sex because of small numbers of subjects, imbalance of sex ratio, and limited age distribution. It was not a double-blinded study, so there can be some bias because the examiner knew who was treated group or control group. Also we did not collect the data of disease duration so we could not prove that there is no significant difference of disease duration between treated group and control group. We recruited participants who had not received any other treatment of myofascial pain syndrome, but a future study can be designed to compare the pain reducing effect with the medication, exercise and ESWT. In this study, we examined the VAS and pressure threshold before the initial treatment and right after the 4th treatment, but it was a limited design due to the revealing duration of ESWT effect. So future studies should examine the short-term and long-term effects. An animal study is essential for investigation of pathophysiology of pain reducing effects in ESWT.
Go to : 
ESWT was effective in relieving pain for myofascial pain syndrome in upper trapezius after therapy 4 times over two weeks. The effect of ESWT in myofascial pain syndrome might be pain relief by alternating concentration of pain related substances, promoting angiogenesis and increasing perfusion at ischemic tissues. With this, we thought that ESWT can be a treatment of myofascial pain syndrome. Considering limitations, a future study should be conducted with more patients, more diverse characteristics of age and sex and evaluating within further duration.
Go to : 
References
1. Sciotti VM, Mittak VL, DiMarco L, Ford LM, Plezbert J, Santipadri E, Wigglesworth J, Ball K. Clinical precision of myofascial trigger point location in the trapezius muscle. Pain. 2001; 93:259–266. PMID: 11514085.

2. Wade B. Trigger points in the upper trapezius or normal subtrapezial anatomy? Physiother Can. 2001; 53:219–222.
3. Fischer AA. Pressure algometry over normal muscles. Standard valuses, validity and reproducibility of pressure threshold. Pain. 1987; 30:115–126. PMID: 3614975.
4. Simons DG, Travell JG, Simons LS. Myofascial pain and dysfunction: upper half of body. 1999. 2nd ed. Baltimore: Lippincott Williams & Wilkins;p. 69–86.
5. Borg-Stein J, Simons DG. Focused review: myofascial pain. Arch Phys Med Rehabil. 2002; 83:S40–S47. PMID: 11973695.
6. Bennet R. Myofascial pain syndromes and their evaluation. Best Pract Clin Rheumatol. 2007; 21:427–445.
7. De las Penas CF, Campo MS, Carnero JF, Miangolarra Page JC. Manual therapies in myofascial trigger point treatment: a systematic review. J Bodyw Mov Ther. 2005; 9:27–34.
8. Rickards LD. The effectiveness of non-invasive treatments for active myofascial trigger point pain: a systematic review of the literature. Int J Osteopath Med. 2006; 9:120–136.

10. Tough EA, White AR, Cummings TM, Richards SH, Campbell JL. Acupuncture and dry needling in the management of myofascial trigger point pain: a systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2009; 13:3–10. PMID: 18395479.
11. Müller-Ehrenberg H, Licht G. Diagnosis and therapy of myofascial pain syndrome with focused shock waves (ESWT). Med Orthop Tech. 2005; 5:1–6.
12. Bauermeister W. Diagnosis and therapy of myofascial trigger point syndrome through stimulation of sensitized nociceptors using focused electrohydraulic shockwaves. Med Orthop Tech. 2005; 5:65–74.
13. Liang HW, Wang TG, Chen WS, Hou SM. Thinner plantar fascia predicts decreased pain after extracorporeal shock wave therapy. Clin Orthop Relat Res. 2007; 460:219–225. PMID: 17353798.

14. Hammer DS, Adam F, Kreutz A, Rupp S, Kohn D, Seil R. Ultrasonographic evaluation at 6-month follow-up of plantar fasciitis after extracorporeal shock wave therapy. Arch Orthop Trauma Surg. 2005; 125:6–9. PMID: 14530990.

15. Wang FS, Yang KD, Chen RF, Wang CJ, Sheen-Chen SM. Extracoporeal shock wave promotes growth and differentiation of bone-marrow stromal cells towards osteoprogenitors associated with induction of TGF-beta1. J Bone Joint Surg Br. 2002; 84:457–461. PMID: 12002511.
16. Shah JP, Danoff JV, Desai MJ, Parikh S, Nakamura LY, Phillips TM, Gerber LH. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil. 2008; 89:16–23. PMID: 18164325.

17. Ottomann C, Hartmann B, Tyler J, Maier H, Thiele R, Schaden W, Stojadinovic A. Prospective randomized trial of accelerated re-epithelization of skin graft donor sites using extracorporeal shock wave therapy. J Am Coll Surg. 2010; 211:361–367. PMID: 20800193.

18. Rompe JD, Hope C, Küllmer K, Heine J, Bürger R. Analgesic effect of extracorporeal shock-wave therapy on chronic tennis elbow. J Bone Joint Surg Br. 1996; 78:233–237. PMID: 8666632.

19. Han TR, Kim JH, Paik NJ, Lim SJ. Importance of local twitch response induced by needling in myofascial pain syndrome. J Korean Acad Rehabil Med. 1999; 23:595–600.
20. Rompe JD, Meuer A, Nafe B, Hofmann A, Gerdesmeyer L. Repetitive low-energy shock wave application without local anesthesia is more efficient than repetitive low-energy shock wave application with local anesthesia in the treatment of chronic plantar fascitits. J Orthop Res. 2005; 23:931–941. PMID: 16023010.
21. Shah JP, Gilliams EA. Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: an application of muscle pain concepts to myofascial pain syndrome. J Bodyw Mov Ther. 2008; 12:371–384. PMID: 19083696.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download