Abstract
Objective
To describe inpatient course and length of hospital stay (LOS) for people who sustain brain disorders nationwide.
Method
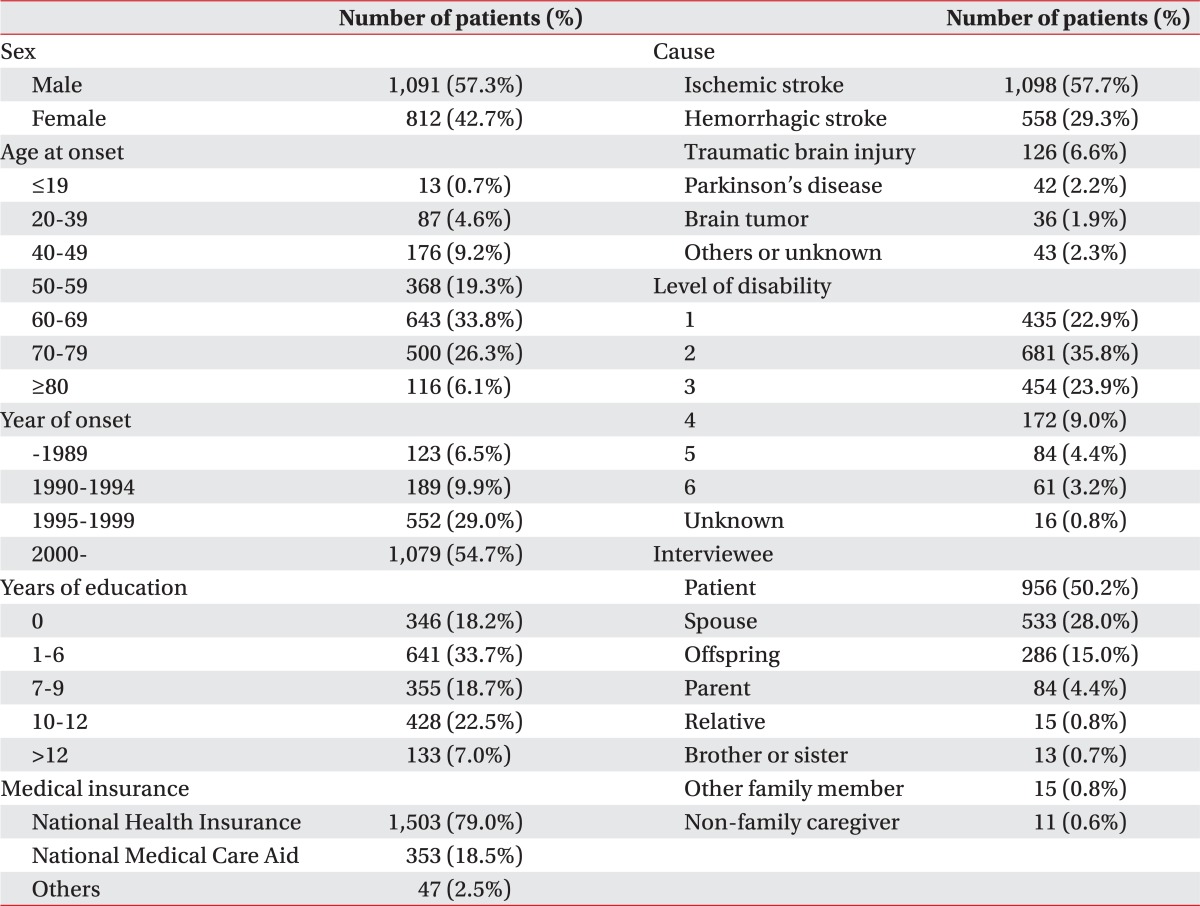
We interviewed 1,903 randomly selected community-dwelling patients registered as 'disabled by brain disorders' in 28 regions of South Korea.
Results
Seventy-seven percent were initially admitted to a Western medicine hospital, and 18% were admitted to a traditional Oriental medicine hospital. Forty-three percent were admitted to two or more hospitals. Mean LOS was 192 days. Most patients stayed in one hospital for more than 4 weeks. The transfer rate to other hospitals was 30-40%. Repeated admissions and increased LOS were related to younger onset age, higher education, non-family caregiver employment, smaller families, and more severe disability.
Go to : 
South Korea has registries for disabled people, among which the registry for patients 'disabled by brain disorders' was initiated in 2000. The 'disabled by brain disorders' registry comprises persons who are limited or dependent in gait or activities of daily living due to disability following organic brain diseases such as cerebrovascular accident (CVA), traumatic brain injury, cerebral palsy, and degenerative brain disorders like Parkinson's disease. By this registry system, people are categorized into 6 levels of disability (Level 1 is the most severe and 6 is the least severe). As of 2011, a total of 261,746 persons were registered, and 333,798 were presumed to be 'disabled by brain disorders', representing 0.73 persons per 1,000.1 When the dysfunction level was estimated using the Modified Barthel Index,2 22.8% of patients 'disabled by brain disorders' were classified as level 1 and 2.1
Eighty-four percent of the patients 'disabled by brain disorders' in Korea had family members as their primary caregivers.1 The lack of social services for the disabled in Korea makes the burden of care heavy. Moreover, the family burden has become heavier as Korean families have changed from large to nuclear in structure.
In Korea, the National Health Insurance program covers approximately 60% of the medical expenditures charged by 96.3% of the population, and the National Medical Care Aid program, which is for the poor, covers 100% of the expenditures charged by 2.1% of the population and approximately 85% of the medical expenditures charged by 1.3% of the population. Furthermore, these programs pay for all inpatient days.3 Therefore, medical fees for inpatient treatment in Korea are relatively low. For these reasons, families tend to be reluctant to take care of patients at home, and patients tend to delay discharge or request transfer to another medical institutions instead of their home. Increases in the length of hospital stay (LOS) and repeated admissions in patients with brain disorders hamper providing appropriate medical service and make the disease burden on society unnecessarily large. Therefore, appropriate policies should be implemented in the provision of inpatient medical services for patients with brain disorders. To guide policy, a thorough analysis is needed of the inpatient course describing characteristics of patients and institutions. However, no studies have investigated the multi-level inpatient treatment course or LOS in patients with brain disorders, especially at a national scale.
Another consideration is that traditional Oriental medicine coexists with Western medicine and is practiced widely in Korea. There is a hospital system in traditional Oriental medicine that is organized similarly to the Western system, and traditional Oriental medicine has long been recognized as an effective treatment for CVA.4 Western medicine hospitals and traditional Oriental medicine hospitals are usually founded independently, but some new hospitals offer both types of medicine.
We sought to investigate the inpatient medical course, including LOS and hospital type, and to determine associated factors in Korean patients disabled by brain disorders at a national level.
Go to : 
This study was part of a larger study investigating utilization of medical services in community-dwelling people disabled by brain disorders. Our questionnaire was developed stepwise. A list of survey questions was developed in an expert meeting, which consisted of professors from the departments of rehabilitation medicine and medical statistics. Survey questions were revised by means of a focus group meeting, which consisted of sample patients and professors from the department of rehabilitation medicine. A draft of the survey questionnaire was developed using factor analysis, and the validity of each item was tested. Patients who visited the outpatient clinics at five major hospitals located in Seoul joined the validity testing. We performed a preliminary study and completed a final survey questionnaire. The survey instrument consisted of 84 questions categorized into 11 sections: demographics, socioeconomic status, disease onset, course of medical treatment, utilization of medical facilities, health status on discharge home, activity level, utilization of traditional Oriental medicine, sequelae of brain disorders, degree of satisfaction with medical services, and current health status. A survey firm was selected, and visiting surveyors were trained twice concerning the questionnaire and interview protocol.
This survey was carried out between September 2005 and May 2006. We recruited community-dwelling patients who were registered as 'disabled by brain disorders' in 28 regional health centers in Korea. These centers are involved in a community-based rehabilitation program run by the National Rehabilitation Hospital in Korea. Patients were sampled through a stratified random sampling in proportion to the constitution rate of the 'disabled by brain disorders' group. Targeted samples (2,002 among 10,469 patients) were allocated in the administrative district: 2 wards in Seoul (257 among 1,342 patients), 8 wards in 6 metropolises (852 among 4,459 patients), 8 small cities (473 among 2468 patients), and 10 rural areas (420 among 2,200 patients). Patients were contacted in advance by phone, and the survey was introduced to the patients or caregivers. Surveyors visited patients who agreed to participate in this study and interviewed the patients or their family members or caregivers after informed consent was obtained. Patients suffering from acute disease and those institutionalized or admitted to the hospital for other medical problems were excluded from the study. Patients (or their family members) who could not answer the survey properly or who did not consent to the survey were excluded, as well.
Demographic data such as sex, age at onset, year of onset with a 5-year interval, years of education, level of disability, and location were independent variables. Dependent variables included type of initial visit and admission, reason for hospital selection, number of hospital admissions, LOS, discharge rate, and discharge destination. Statistical analysis was performed with Student's t-test, chi-square analysis, or ANOVA using SPSS statistical software version 12 SPSS V12.0K (SPSS Inc., Chicago, USA). We rejected null hypotheses of no difference if p-values were less than 0.05.
Go to : 
A total of 1,903 patients (mean age 62.8±12.8 years, range 9-93 years) were surveyed, resulting in a response rate of 95.1% (Table 1). The mean time duration since disease onset was 84.6±67.7 months (range 1-589 months).
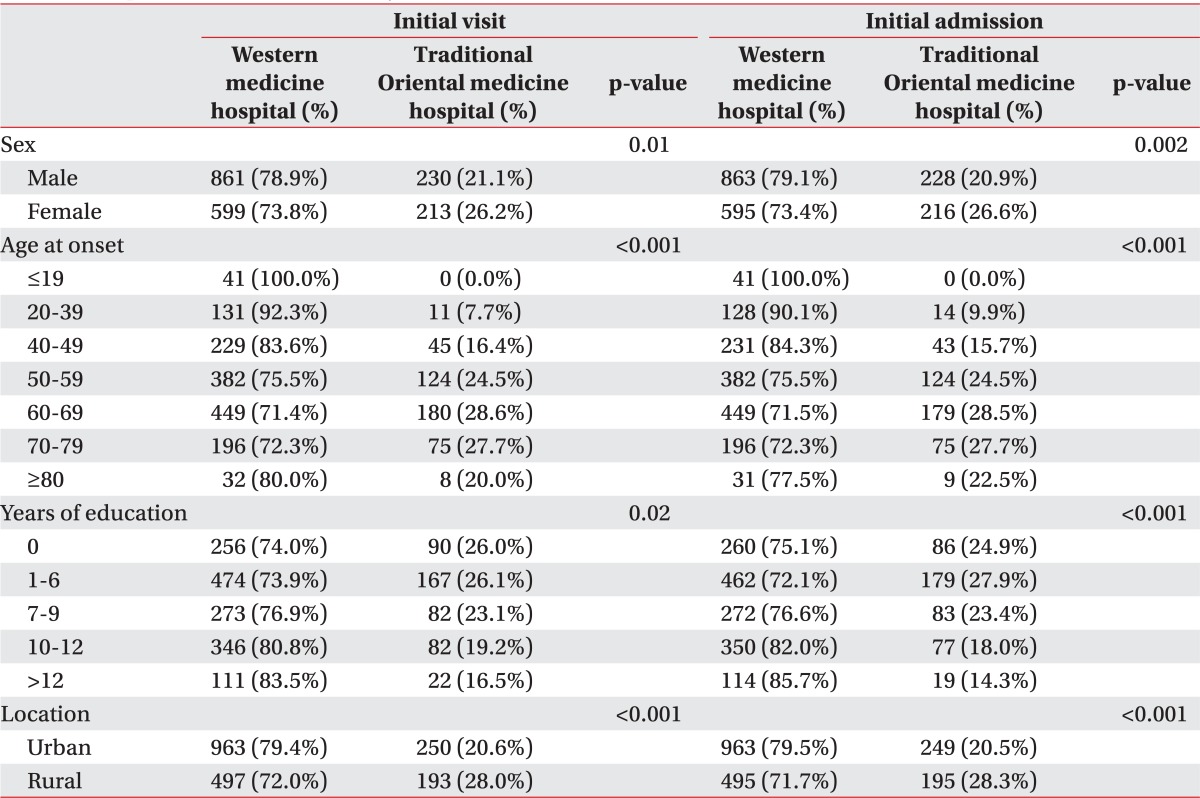
Most (76.7%) patients initially visited a Western medicine hospital. The proportion of subjects who visited traditional Oriental medicine hospitals was 19.3%. Four percent of subjects visited conjoined Western and traditional Oriental medicine hospitals. Male patients, younger patients, patients with higher education, and urban inhabitants preferred Western medicine hospitals to traditional Oriental hospitals for the initial visit (Table 2). Preferences for either Western or traditional Oriental medicine have not changed significantly over the past several decades.
Most patients (76.6%) were also initially admitted to a Western medicine hospital. Eighteen percent of subjects were admitted to traditional Oriental medicine hospitals and five percent were admitted to conjoined Western and traditional Oriental medicine hospitals. The characteristics of patients who preferred Western medicine hospital for the initial admission were nearly the same as those who chose Western medicine hospitals for their initial visit (Table 2). More patients (52.1% compared to 26.6% for traditional Oriental medicine hospitals) selected Western medicine hospitals as the initial admission hospital following the decision of family members.
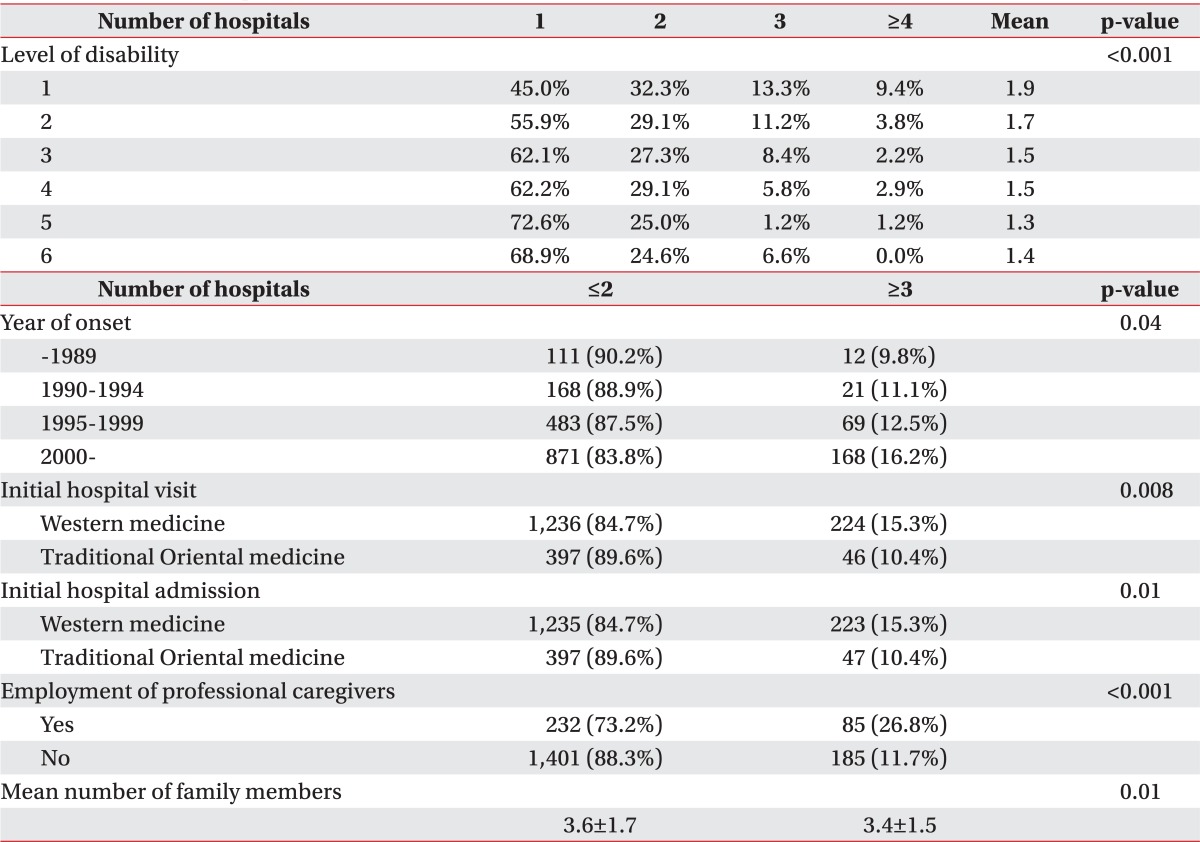
Almost 57% of patients were admitted to one hospital, while 29.0% were admitted to two hospitals, 9.8% were admitted to three hospitals, and 4.5% were admitted to four or more hospitals. The number of patients admitted to three or more hospitals has increased over the past several decades (Table 3). Patients with graver disabilities were admitted to more hospitals (p<0.001). Patients who employed a professional caregiver and who had a smaller number of family members were more likely to be admitted to three or more hospitals (Table 3).
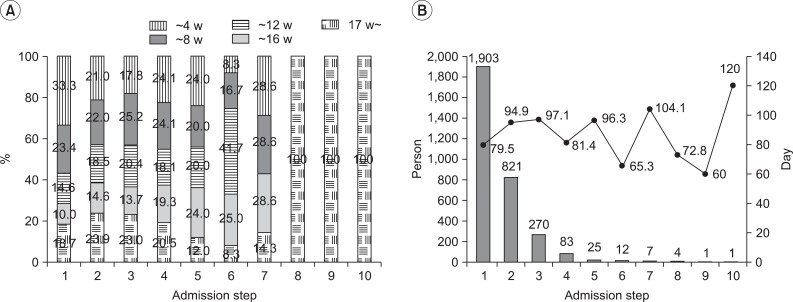
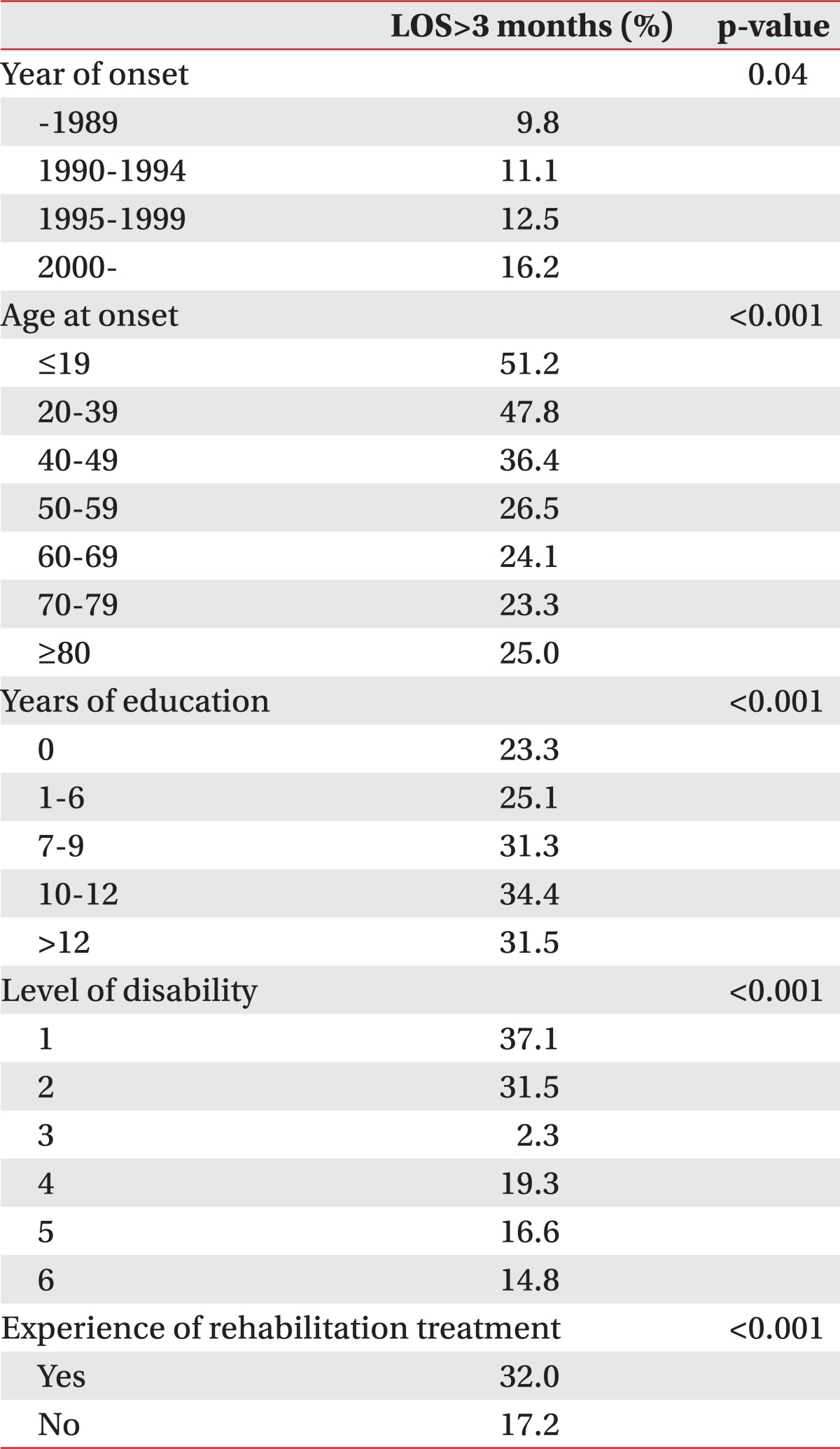
The total mean LOS was 191.5 days. Most patients stayed in one hospital for more than four weeks and the mean LOS for each individual admission step tended to increase through admission steps regardless of the admission course (Fig. 1). Patients who were younger, more educated, or more severely disabled, or who underwent rehabilitation treatment were more likely to be admitted for more than three months (Table 4).
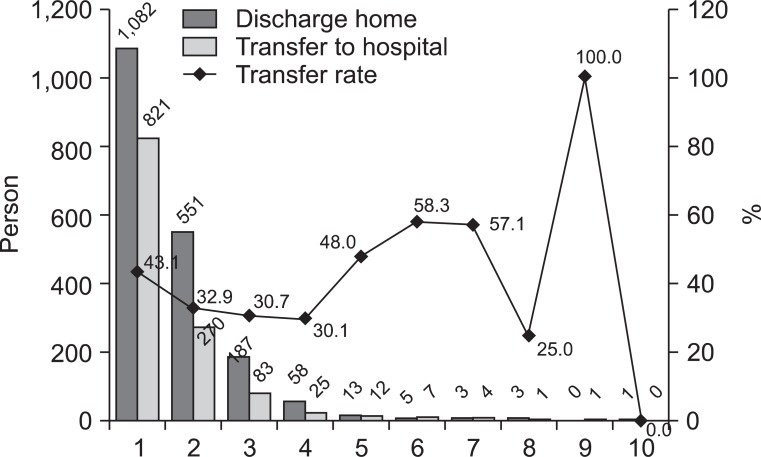
The proportion of patients transferred to other hospitals is depicted in Fig. 2. The transfer rate for each admission step was between 30% and 40% and did not differ significantly according to hospital type. Twenty-eight percent of patients decided to be transferred to other hospitals because of dissatisfaction with previous medical services and twenty-one percent decided the transfer because of recommendation of the medical staff (20.8%). Patients with graver disability (p<0.001) were more likely to decide to transfer due to hospital variables, such as dissatisfaction with previous medical services or the recommendation of medical staff. The proportion of patients expressing dissatisfaction with medical services was much lower, at 3.5% among those discharged home.
Go to : 
This is the first study to detail the characteristics of inpatient hospital course in community-dwelling patients registered as 'disabled by brain disorders' in the Korean population. To understand the characteristics of the inpatient course and discharge of patients with brain disorders is important for medical staff, as well as for health administrators. The factors that influence LOS and discharge destinations should be understood so that appropriate rehabilitation strategies and efficient planning of medical services can be provided for patients disabled by brain disorders.5
Compared to Western medicine, traditional Oriental medicine has long been regarded as having equal social and cultural status in stroke treatment in Korea.6 In this study, one of five Koreans selected a traditional Oriental medicine hospital for the treatment of brain disorders, and most patients were influenced by the generalized Korean idea that traditional Oriental medicine is effective in treating stroke. The preferred type of medicine differed significantly according to sex, age, education level, and location. The decision concerning initial hospital admission was found to be affected by family and neighbors. This corresponds with the results of a previous study showing that neighborhoods contribute substantially to disease awareness and treatment.7
The mean LOS in this study was 191.5 days. The mean LOS for CVA in the United States is 4.9 days.8 Even though the population in this study (registered as disabled) did not include patients with mild stroke or brain disorders without significant accompanying disability, the LOS was much longer than the average LOS seen in the US. Even when the inpatient medical treatment including rehabilitation is finished, patients with brain disorders usually feel insufficiently recovered and desire longer-term treatment. Patients and their families are concerned about returning to the community with persistent disability and are not convinced that they recover sufficient function at the time of discharge. In reality, patients tend to have higher expectations about their recovery. They usually feel reassured during inpatient treatment, and discharge is regarded as the end of recovery; discharge prior to the attainment of expected recovery leaves patients with a sense of abandonment and distress.9 Moreover, the burden of care in patients with brain disorders is more substantial than that seen in patients with any other disease.10 CVA, which was seen in 87.0% of the subjects in this study, is known to be the second highest cause of disease burden in Korea.11 Home care for an illness such as a brain disorder is known to place a considerable burden on caregivers, especially on female caregivers in Korea, where men traditionally provide financial security and women care for the household.12 In such circumstances, patients are reluctant to return home, and their reluctance is shared by their families. Therefore, it is frequently difficult to establish agreement between the medical staff and patients and their families concerning the time of discharge.
The health expenditure in Korea is the third lowest among OECD countries, and the health spending per capita in Korea ranks below the OECD average.13 Medical fees for inpatient care are also low. Moreover, there is no limitation on the number of hospital admissions or the admission period, and social infrastructure and services for the disabled are lacking. It is no surprise that we noted prolonged admissions in patients with brain disorders and found that LOS is on the rise. The large disparity between our LOS and the OECD average is attributable to socioeconomic factors in Korea, rather than to clinical factors such as medical complications.
The LOS at each admission step was usually over four weeks, and increased with advanced admission steps. The patients with a mean LOS shorter than one month was at most 20% on the second admission step. Patient characteristics related to longer LOS included younger age, higher education level, more severe disability, and experience with rehabilitation treatment.
We found that the number of patients admitted to three or more hospitals has increased over the past several decades. Patients with severe disability, with fewer family members, and with a non-family member caregiver are more likely to be admitted to more hospitals. This corresponds with a previous study showing that high level impairment is related to a low likelihood of discharge home.14 This finding suggests that the burden imposed on family members at home influences the discharge destinations of patients disabled by brain disorders. The mean LOS in one hospital was longer in patients who were admitted to more hospitals. In a previous study, LOS was shown to be influenced significantly by medical complications.15 However, longer LOS may also be attributable to non-medical factors such as waiting for space to open at the next destination. When patients are set to be transferred to another hospital, they usually need to wait until there is an available patient bed. Therefore, counseling patients and family members about transfer or discharge, advanced transfer planning and efficient discharge procedures will shorten LOS.16
Decision-making concerning the referral and transfer of patients with brain disorders is complex and must account for clinical and non-clinical factors,17 such as health service resources, perception of patient motivation, and extent of physical recovery.9 The rate of transfer to another hospital was between 30% and 40% at each admission step. More patients or caregivers held the medical staff responsible for their transfer rather than themselves (48.8%), a trend that was more pronounced in patients with more severe disability. More patients said their transfer was recommended by medical staff at an advanced step of admission. This implies there was a clash of opinions between medical staff members who recommended that patients be discharged and patients or families who wanted longer hospital stay. The proportion of patients expressing dissatisfaction with medical services was much lower among those discharged home (3.5%) than among those transferred (28.0%).
There are several limitations to this study. First, the accuracy of data concerning LOS, order of admission, and type of medical institutions could be affected by the nature of the survey, based as it was on the memories of patients or their caregivers. This may also explain why very few (1.3%) indicated that unavailability of nursing by a family member was the reason why they decided to transfer to another hospital instead of being discharged home. Second, we collected only the patients' accounts of why they were transferred or discharged home. We did not study the accounts of the medical staff. Therefore, the reasons for the decision on transfer or discharge collected in this study reflect the patients' perspective only. Third, we could not obtain clinical data concerning physical function or complications that could influence transfer or LOS. Fourth, this study recruited patients with a wide range of disease onset. Therefore, there were mixed data from different time points, which diminished the clinical significance of the data. However, a potential strong point of our study is that data analysis is not limited only to a specific time period and instead shows changes over a time period. Fifth, we only performed univariate analyses. We did not employ multivariate analyses to control other factors or to check collinearities between variables. Lastly, this study did not limit disease to the cause of disability. Depending on diagnosis, there could be a variety of disease courses, characteristics, and strategies of care.
In spite of the above limitations, we offer several conclusions concerning the inpatient course and LOS of patients disabled by brain disorders in South Korea. Patients showed considerably prolonged LOS and repeated admissions. Factors increasing the burden of care in patients were found to influence LOS significantly. Considerations of these characteristics are crucial for strategic planning and provision of inpatient medical services and for relieving the burden of care in patients disabled by brain disorders, both in social and personal respects.
Go to : 
ACKNOWLEDGEMENTS
This work was supported by the grant from Samsung Life Insurance. We gratefully acknowledge the help of the Korean Society for NeuroRehabilitation and National Rehabilitation Center, Seoul, Korea. We are also grateful to every single patient who participated in this study.
Go to : 
References
1. Kim SH, Byun YC, Sohn CG, Lee YH, Lee MK, Lee SH, Kang DW, Kwon SJ, Oh HK, Yoon SY, et al. Study on the disabled 2011. 2011. 1st ed. Seoul: Korea Institute for Health and Social Affairs (KIHASA);p. 5–7.
2. Granger CV, Albrecht GL, Hamilton BB. Outcome of comprehensive medical rehabilitation: measurement by PULSES profile and the Barthel Index. Arch Phys Med Rehabil. 1979; 60:145–154. PMID: 157729.
3. Lee JY, Kim CY. 2006 National health insurance statistical yearbook. 2007. 1st ed. Seoul: Korea Ministry of Health and Welfare (KMHW) & National Health Insurance Corporation (NHIC);p. 6.
4. Kim JS, Yoon SS. Perspectives of stroke in persons living in Seoul, South Korea. A survey of 1000 subjects. Stroke. 1997; 28:1165–1169. PMID: 9183344.
5. Somerford PJ, Lee AH, Yau KK. Ischemic stroke hospital stay and discharge destination. Ann Epidemiol. 2004; 14:773–777. PMID: 15519899.

6. Park MH, Jo SA, Jo I, Kim E, Eun SY, Han C, Park MK. No difference in stroke knowledge between Korean adherents to traditional and western medicine - the AGE study: an epidemiological study. BMC Public Health. 2006; 6:153–162. PMID: 16772038.

7. Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: the role of neighborhood context. Soc Sci Med. 2007; 65:1853–1866. PMID: 17640788.

8. Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, et al. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010; 121:e46–e215. PMID: 20019324.
9. Wiles R, Ashburn A, Payne S, Murphy C. Discharge from physiotherapy following stroke: the management of disappointment. Soc Sci Med. 2004; 59:1263–1273. PMID: 15210097.
10. Magliano L, Fiorillo A, De Rosa C, Malangone C, Maj M. Family burden in long-term diseases: a comparative study in schizophrenia vs. physical disorders. Soc Sci Med. 2005; 61:313–332. PMID: 15893048.

11. Yoon SJ, Bae SC, Lee SI, Chang H, Jo HS, Sung JH, Park JH, Lee JY, Shin Y. Measuring the burden of disease in Korea. J Korean Med Sci. 2007; 22:518–523. PMID: 17596664.

12. Kim JS, Lee EH. Cultural and noncultural predictors of health outcomes in Korean daughter and daughter-in-law caregivers. Public Health Nurs. 2003; 20:111–119. PMID: 12588428.

13. OECD. OECD reviews of health care quality: Korea 2012--rasing standards. 2008. 1st ed. Paris: OECD Publishing;p. 81–82.
14. Massucci M, Perdon L, Agosti M, Celani MG, Righetti E, Recupero E, Todeschini E, Franceschini M. Prognostic factors of activity limitation and discharge destination after stroke rehabilitation. Am J Phys Med Rehabil. 2006; 85:963–970. PMID: 17033592.

15. Saxena SK, Ng TP, Yong D, Fong NP, Gerald K. Total direct cost, length of hospital stay, institutional discharges and their determinants from rehabilitation settings in stroke patients. Acta Neurol Scand. 2006; 114:307–314. PMID: 17022777.

16. van Straten A, van der Meulen JH, van den Bos GA, Limburg M. Length of hospital stay and discharge delays in stroke patients. Stroke. 1997; 28:137–140. PMID: 8996502.

17. Foster M, Tilse C, Fleming J. Referral to rehabilitation following traumatic brain injury: practitioners and the process of decision-making. Soc Sci Med. 2004; 59:1867–1878. PMID: 15312921.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download