Abstract
In this article, we report a case where a videofluoroscopic swallowing study (VFSS) revealed the cause of a recently developed idiopathic dysphagia in a 66-year-old patient and enabled emergent treatment. The patient reported a 10-day history of fever, cough, sputum production, and progressive jaundice. He was then admitted to the hospital with suspicion of aspiration pneumonia. Despite treatment with antibiotics, fever and leukocytosis were persistent. As he also reported dysphagia, we performed the VFSS, which showed subglottic aspiration on all types of food and revealed a retropharyngeal mass causing mechanical compression. A contrast-enhanced computerized tomography (CT) of his neck was performed following the VFSS, which helped diagnose the mass as an extensive retropharyngeal abscess with mediastinitis. Following this diagnosis, emergent surgical incision and drainage was performed on the patient. Although the VFSS is primarily designed to evaluate swallowing function rather than to diagnose a disease, it can be used to reveal the primary medical cause of dysphagia while it studies the mechanical and structural abnormalities in the oropharyngeal and esophageal regions. This study also proposes that retropharyngeal abscess should be considered in the differential diagnosis of cases showing progressive dysphagia with fever. As confirmed through this work, the VFSS can function as a useful tool for detecting crucial diseases accompanying deglutition disorder.
Go to : 
The videofluoroscopic swallowing study (VFSS) is a reliable diagnostic tool for swallowing disorders.1 During the VFSS, examiners usually study the flow of the food bolus through the oropharyngeal and esophageal regions and the real-time movements of the oropharyngeal and esophageal structures, which vary in length, shape, and thickness. Occasionally, the VFSS can also provide crucial information on the hidden cause of swallowing disorders. In this study, we present a case in which the cause of recently developed dysphagia in a 66-year-old patient, where an emergent treatment was needed, was revealed by the VFSS.
Go to : 
A 66-year-old male patient reported a 10-day history of fever, cough, sputum production, and progressive jaundice. He was a chronic alcoholic who had been drinking two or more bottles of liquor daily, and he was earlier diagnosed with diabetes mellitus and liver cirrhosis. He had suffered from cerebral infarction four years earlier, but there were no neurological sequelae, including dysphagia.
He visited a hospital nearby, and a plain chest X-ray and an abdominal computerized tomography (CT) scan were done. The chest X-ray showed bilateral lower lung field haziness and the abdominal CT scan revealed a 27-mm liver mass. With suspicion of aspiration pneumonia and hepatocellular carcinoma, he was transferred to a secondary hospital and admitted to the Department of Internal Medicine. Despite three days of intravenous antibiotics (ceftriaxone and azithromycin), a fever running temperatures more than 37.5℃ persisted.
As he also complained of difficulty swallowing food and showed reflexive cough while drinking water, it was decided to evaluate his swallowing function.
A physical examination revealed intact gag reflexes but decreased pharyngeal elevation. The patient reported that the swollen bilateral anterior neck area had persisted for the last two weeks before the admission. The lower left quadrant of the anterior neck was particularly swollen with mild tenderness. A follow-up plain radiograph of the chest was normal.
The laboratory tests showed leukocytosis (white blood cell (WBC) count: 18,690/µl) and neutrophilia (89% of WBC). C-reactive protein (CRP) increased to 14.8 mg/dl.
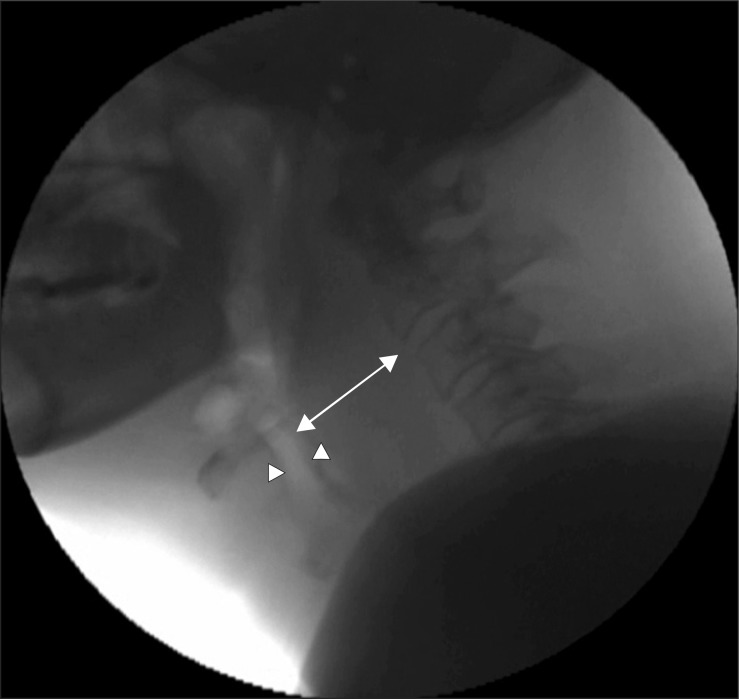
We performed the VFSS using the following types of food: puree-like diet, boiled rice, semi-blended diet, curd-type yogurt, and small and large amounts of fluid. The VFSS showed that the soft tissue located posterior to the upper esophagus was severely swollen, and this retropharyngeal mass caused mechanical obstruction (Fig. 1). As the mass restricted laryngeal elevation and epiglottic rotation severely, aspiration occurred in all types of food, with a high risk of suffocation on puree-like diet. Moderate-to-severe grade residues were observed in the valleculae and the pyriform sinuses for all types of food. Based on the findings of the VFSS, we recommended tube feeding. However, insertion of the nasogastric tube was unsuccessful because of the obstruction by the retropharyngeal mass.
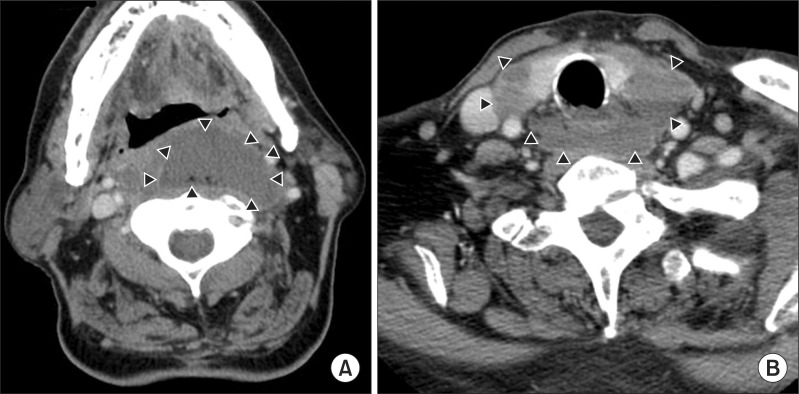
On the day of the VFSS, we recommended an urgent contrast-enhanced CT scan of the neck (Fig. 2). The CT revealed loculated fluid collection in the retropharyngeal, anterior cervical, pericarotid, and prevertebral spaces. In addition, fluid collection was observed in the upper mediastinum, and the airway was severely narrowed in the subglottic region. Several reactive intraparotid or superficial cervical lymph nodes were observed on the left side of the neck. These findings were consistent with the diagnosis of retropharyngeal abscess with mediastinitis.
The patient underwent an emergency tracheostomy, and an incision was made to drain the abscess. He remained afebrile throughout the postoperative period with intravenous administration of ampicillin-sulbactam. As a culture of the purulent discharge from the abscess revealed methicillin-resistant Staphylococcus aureus and Klebsiella pneumoniae, the patient was administered ceftriaxone-vancomycin instead of the ampicillin-sulbactam combination. On the fifth postoperative day, CRP decreased to 10.2 mg/dl.
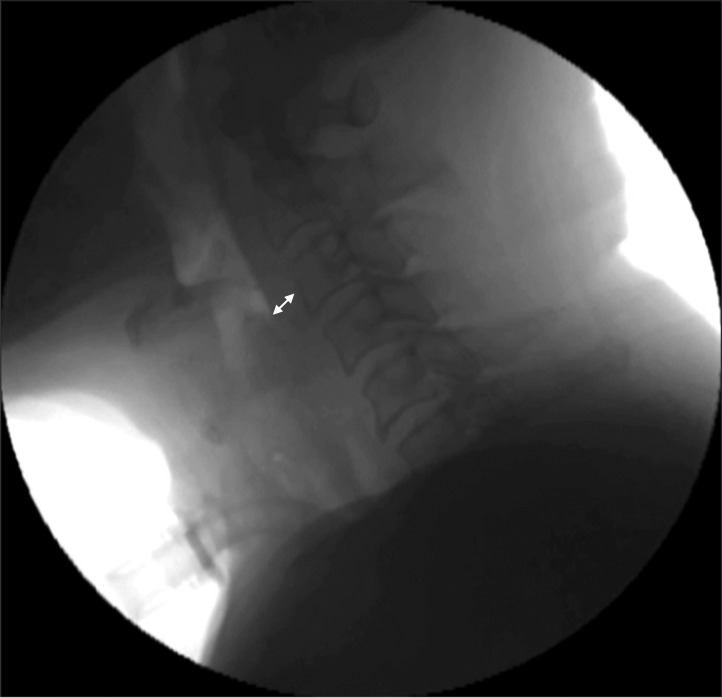
After 10 days of intensive care, the patient was transferred to the general ward. An examination on the 18th postoperative day showed that his general condition had improved significantly, and a follow-up VFSS was performed (Fig. 3). When curd-type yogurt or a large amount of free fluid was administered to the patient, supraglottic penetration was observed. However, the amount of pharyngeal residue was markedly reduced when compared with his initial condition on admission. He was recommended initiation of oral feeding training with small amounts of puree-like food; however, the nasogastric tube feeding was advised to be maintained.
The tracheostomy tube was removed a week after the second VFSS. A third VFSS was performed on the patient two weeks after the second study, and very little silent aspiration was observed with a teaspoon of fluid. We recommended initiation of full oral feeding with puree-like consistency. A follow-up chest CT showed improvement in the mediastinal extension of the deep neck infection. The WBC count and CRP were normalized to 7,510/µl and 0.19 mg/dl, respectively. He was discharged 46 days after surgery, and the swallowing function continued to improve steadily allowing stable full oral intake.
Go to : 
The retropharyngeal space is situated behind the pharynx, limited by the buccopharyngeal fascia anteriorly, the prevertebral fascia posteriorly, and the carotid sheath laterally. It extends from the base of the skull to the posterior mediastinum. Retropharyngeal abscess is a rare but potentially life-threatening infection requiring immediate emergent treatment. The infection usually develops following direct trauma to the pharynx or esophagus by a foreign body along with dissemination from an adjacent focus. Immunocompromised patients or patients with chronic illnesses such as diabetes or alcoholism are at increased risk for retropharyngeal abscess.2
The overall mortality in patients with retropharyngeal abscess has been reported to range from 1.0% to 2.6%.2,3 If the lesion extends to the surrounding regions, retropharyngeal abscess can lead to internal jugular vein thrombosis, carotid arterial erosion, pericarditis, epidural abscesses, and sepsis.4 If it is allowed to invade the mediastinum, mortality increases to 50% even with antibiotic therapy. Hence, early diagnosis and proper treatment with broad spectrum antibiotics are critical.5
The most common symptoms that lead to successful diagnosis are fever, sore throat, neck pain, drooling, dysphonia, and dysphagia. Dysphagia and odynophagia occur in about 75% of patients.6 An enlarged mass compresses the posterior pharyngeal wall and hinders the constriction of pharyngeal muscles and rotation of the epiglottis.
The VFSS has high clinical value in evaluating swallowing function in patients with oropharyngeal and esophageal dysphagia. It also functions as an effective diagnostic tool for diverse lesions causing dysphagia.7 The VFSS can subsequently indicate proper treatment for dysphagia depending on the cause, which ranges from diet modification to surgical intervention.8 In this study, the VFSS that was performed to evaluate the patient's swallowing function revealed an undiagnosed retropharyngeal abscess accompanying mediastinitis and enabled urgent treatment.
Retropharyngeal abscess requires urgent surgical treatment and should be considered in the differential diagnosis of cases showing progressive dysphagia with fever. The VFSS is a valuable tool not only for functional evaluation but also for serious detection of retropharyngeal abscess causing mechanical dysphagia.
Go to : 
References
1. Castell DO, Donner MW. Evaluation of dysphagia: a careful history is crucial. Dysphagia. 1987; 2:65–71. PMID: 3507297.

2. Wang LF, Kuo WR, Tsai SM, Huang KJ. Characterizations of life-threatening deep cervical space infections: a review of one hundred ninety-six cases. Am J Otolaryngol. 2003; 24:111–117. PMID: 12649826.

3. Ridder GJ, Technau-Ihling K, Sander A, Boedeker CC. Spectrum and management of deep neck space infections: an 8-year experience of 234 cases. Otolaryngol Head Neck Surg. 2005; 133:709–714. PMID: 16274797.
4. Lazor JB, Cunningham MJ, Eavey RD, Weber AL. Comparison of computed tomography and surgical findings in deep neck infections. Otolaryngol Head Neck Surg. 1994; 111:746–750. PMID: 7991254.

5. Sichel JY, Dano I, Hocwald E, Biron A, Eliashar R. Nonsurgical management of parapharyngeal space infections: a prospective study. Laryngoscope. 2002; 112:906–910. PMID: 12150626.

6. Tannebaum RD. Adult retropharyngeal abscess: a case report and review of the literature. J Emerg Med. 1996; 14:147–158. PMID: 8740744.

7. Martin-Harris B, Logemann JA, McMahon S, Schleicher M, Sandidge J. Clinical utility of the modified barium swallow. Dysphagia. 2000; 15:136–141. PMID: 10839826.

8. Lind CD. Dysphagia: evaluation and treatment. Gastroenterol Clin North Am. 2003; 32:553–575. PMID: 12858606.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download