Abstract
Objective
To verify the influence of sour taste on swallowing and the presence of reflex cough when sour material was swallowed in patients with dysphagia secondary to brain injury.
Method
Fifty dysphagic brain injury patients who underwent videofluoroscopic swallowing study (VFSS) were recruited. The patients who had shown severe aspiration at 2 ml of liquid were excluded. The dysphagic patients were given 5 ml each of a sour tasting liquid (SOUR) and a thin liquid barium (LIQUID) in random order. An expert analyzed the result of VFSS by reviewing recorded videotapes. Analysis components consisted of the Penetration-Aspiration-Scale (PAS) score, oral transit time (OTT), pharyngeal transit time (PTT), pharyngeal delay time (PDT) and the reflex cough presence.
Results
The PAS score for SOUR was significantly lower than the one for LIQUID (p=0.03). The mean OTT for SOUR was significantly shortened compared to that for LIQUID (p=0.03). The mean PTT and PDT were also shortened in SOUR, although the differences were not statistically significant (p=0.26 and p=0.32, respectively). There was no significant difference between SOUR and LIQUID regarding the presence of reflex cough (p=1.00).
Videofluoroscopic swallowing study (VFSS) is often considered the gold standard in the diagnosis and management of dysphagia.1,2 However, often a reflex cough is not shown during VFSS in dysphagic patients, although they show reflex cough during regular diet. This can be attributed to the differences between swallowing a regular diet and a VFSS. The difference in characteristics of food ingested may be one of them. Generally, food of single consistency is used for VFSS. In a regular diet, however, we eat food composed of mixed consistencies. There are some studies that have studied the differences in physiology of swallowing between single and mixed consistencies.2,3 In addition, the intensity of the gustatory stimulation is also a significant factor that differentiates between the swallowing in regular diet and VFSS. Generally, less stimulant materials are given to patients for the VFSS. Many researchers have also revealed that swallowing is highly influenced by the sensory stimulation of taste.4-12 Furthermore, some studies have shown the influence of sour taste has on swallowing.6-8 Despite the fact that a reflex cough is evoked by acid aspiration,13 no studies have been performed on the presence of reflex cough during the swallowing of sour bolus in VFSS. Also, a blind study focused on the influence of sour taste and swallowing has not been done.
This study aimed to verify the influence of sour taste on swallowing and the presence of a reflex cough when sour material was swallowed in patients with dysphagia secondary to brain injury, by blind study.
Fifty dysphagic brain injury patients who underwent VFSS between March 2011 and July 2011 at our clinic were recruited. The patients on whom it was dangerous to proceed the exam, due to severe aspiration at 2 ml of liquid, were excluded. Participants were informed of the purpose and risks of this study and a written informed consent was submitted.
We designed a blind study. One researcher prepared both target and placebo tasting liquid and put them in random sequence. Another researcher blinded to the sequence gave each liquid to the participants. Then each liquid swallowing was recorded separately. The other researcher interpreted the recorded VFSS with blinded information.
The patients were seated in an upright position. The fluoroscopy machine was the Winscope 6000 (Toshiba, Otawara, Japan). The fluoroscopy tube was located to the left side of the neck of the patients and it was adjusted to show the nasal and oral cavity, larynx, pharynx, trachea and upper esophagus. X-rays were taken 5 seconds to correct the location of the fluoroscopy tube.
We used liquid mixtures for the test. We mixed water and barium sulfate liquid to make the non sour tasting liquid (LIQUID) at a ratio of 2 : 1, respectively. The barium sulfate liquid was Raydix suspension (Dongindang, Siheung, Korea). We also prepared a sour tasting liquid (SOUR) which consisted of a mixture of lemon juice and barium sulfate liquid at a ratio of 2 : 1, respectively. The lemon juice was Lazy Lemon Juice (Polenghi, Milano, Italy).
During the first phase, participants were given 2 ml of LIQUID. The exam was stopped if participants showed severe aspiration at this phase. During the second phase, they swallowed 5 ml of both SOUR and LIQUID in random sequence. To wash out the residual chemical effects of the previous liquid, they swallowed 2 ml of water before the next swallowing.
Patients were instructed to swallow in their usual manner, and this was performed twice for each liquid. X-rays were projected from the beginning of the swallowing process until the moment the liquid passed through the upper esophagus. The images were recorded at a rate of 30 frames per second.
We used recorded videotapes, which allowed for analyses in slow motion and frame-by-frame. The components of the analysis consisted of the Penetration-Aspiration-Scale (PAS) score, oral transit time (OTT), pharyngeal transit time (PTT), pharyngeal delay time (PDT) and the presence of reflex cough. The triggering marker of the onset of the pharyngeal swallow was the elevation of the hyoid bone or larynx. The severity of penetration-aspiration was quantified from 1 to 8 points using the validated Penetration-Aspiration Scale (PAS).14
Passage times were measured as follows: OTT was measured from the bolus movement onset in the mouth until the the bolus head reached the point where the lower rim of the mandible crosses the tongue base. PTT was measured from the arrival of the main bolus head at the point where the lower rim of the mandible crosses the tongue base to the point where the bolus tail passes through the cricopharyngeal region. PDT was measured from the bolus head arrival at the point where the lower rim of the mandible crosses the tongue base until the first onset of the laryngeal elevation. A positive value of the pharyngeal delay time indicated that the pharyngeal swallow was initiated after the main bolus head had passed through the intersection, while a negative value indicated the reverse.3,15,16
The Wilcoxon signed rank test was used to test the differences between the severities of penetration-aspiration of each liquid. The paired t-test was used to test the difference between the passage times of each liquid. The McNemar test was used to test the difference in the presence of reflex cough between each liquid. The p-values less than 0.05 were considered statistically significant. The SPSS 12.0 program was used for the statistical analyses.
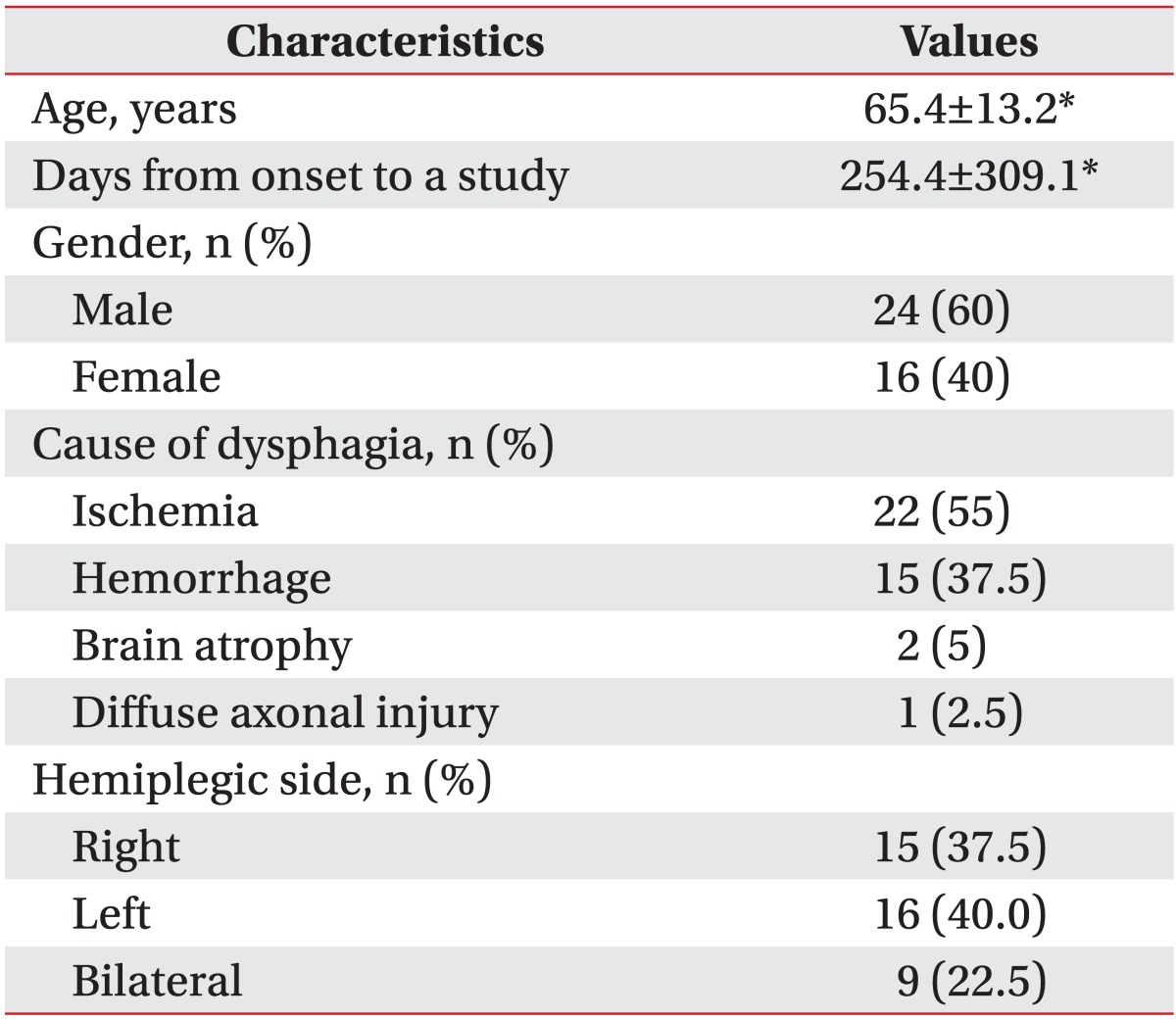
Ten patients on whom it was dangerous to proceed the exam due to severe aspiration at 2 ml amounts of LIQUID, were excluded. Excluding these cases, 40 patients were finally included in this study. The general characteristics of the subjects are listed in Table 1.
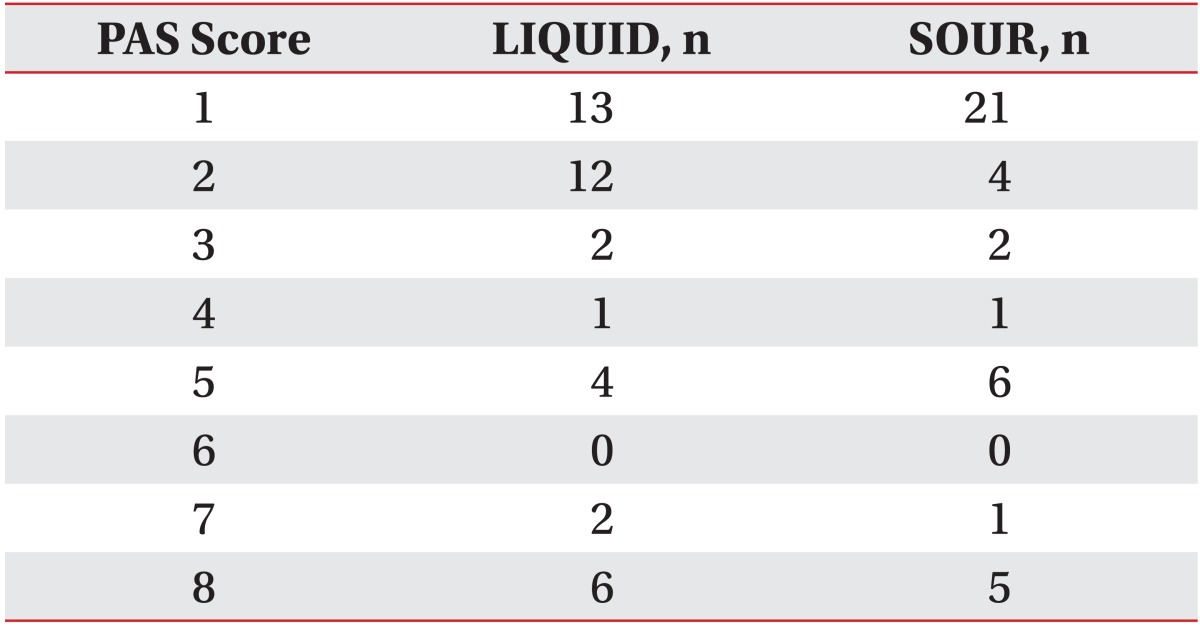
The PAS score for each liquid is shown in Table 2. The number of penetrations (from 2 to 5 points of PAS) and aspirations (from 6 to 8 points of PAS) for SOUR was 13 (32.5%) and 6 (15.0%), respectively. The number of penetrations and aspirations for LIQUID was 19 (47.5%) and 8 (20.0%), respectively. The PAS score for SOUR was significantly lower than the one for LIQUID (p=0.03). The improvement of the PAS scores with SOUR is shown in Table 3.
The mean results for SOUR were OTT 1.47±2.10, PTT 0.97±0.46 and PDT 0.35±0.44 seconds, respectively. The mean results for LIQUID were OTT 2.36±3.38, PTT 1.19±1.30 and PDT 0.53±1.28 seconds, respectively. The mean OTT for SOUR was significantly shortened (p=0.03). The mean PTT and PDT were also shortened in SOUR, although the differences were not statistically significant (p=0.26 and p=0.32, respectively).
Impaired sensation in the oropharynx can cause dysphagia, including aspiration, and inversely, an increased sensory stimulation can improve dysphagia.15-17 In addition, patients with an impaired sensation of the oropharynx, have longer swallowing passage times and consequently an increased risk of aspiration.15 Prior researchers have reported that a major reason for the promotion of reflex swallowing by sour taste is the increase of sensory stimulation to the brain via sensory nerves.6-8 One of these researchers evaluated 19 patients with stroke, using a videofluoroscopy to note the differences in swallowing with and without lemon added to the material.7 There was reduction in the amount of aspiration and a shortening of the oropharyngeal passage time when a sour bolus was applied. Likewise, our current results are similar to those of prior studies. The oropharyngeal passage times were shortened by the sour gustatory stimulation, which consequently lowered the chances of penetration-aspiration. We believe that the reason for no statistically significant differences of PTT and PDT is due to not only small sample size but also to the concentration of sour taste. The intensity of the sour gustatory receptor sensory input generally depends on the concentration of acidity.6 Moreover the sensory thresholds for sour taste of the palate are higher than those of the tongue.10,11,18 However, this study was done using only with a certain concentration. We thought that the reason why the results of PTT and PDT are not statistically significant is that the concentration of the SOUR which may be enough to exceed the oral sensory threshold, but may not be enough to exceed the pharyngeal sensory threshold.
Despite the fact that the reflex cough is evoked by the aspiration of acid solution,13 there were only 3 patients who showed a reflex cough in our study. This may be caused by the exclusion of 10 patients on whom it was dangerous to proceed with the exam due to severe aspiration. We could not perform the test on them due to the ethical problems related to aspiration pneumonia. Moreover, as the same assumption stated above, it may be also affected by the concentration of acidity which was insufficient to exceed the sensory threshold of the pharyngeal reflex. Further studies are needed in larger sample sizes and different concentrations of sour taste.
Swallowing is influenced by the characteristics of food.3 There are differences between single and mixed consistencies that affect the physiology of swallowing.2,3 In our study, additionally, there was an improvement of swallowing in sour taste. As the generally followed VFSS protocol is not enough to reflect the regular diet, other factors which affect the physiology of swallowing, such as sour taste and mixed consistencies, would provide more detailed results if included in the test.
Swallowing itself is the best treatment for improving swallowing in dysphagia patients.19,20 However, due to risks, such as aspiration pneumonia, it is not safe to practice swallowing with any random material. Therefore VFSS is performed by changing only the viscosity of the material swallowed in order to determine the best viscosity for the therapeutic diet.1,21 The protocol generally followed for VFSS measures only viscosity. However, our results have shown that patients may have different chances of aspiration depending on the presence of sour taste at the same viscosity. Furthermore, other studies suggest that sensory stimulation therapy using sour taste could improve swallowing.7,8,22 Thus we recommend considering the use of sour tasting material for swallowing as a treatment for dysphagia. For example, there may be a patient who has shown safer swallowing with sour tasting material, as compared to one without taste at the same viscosity. For those patients, we recommend considering the use of a sour tasting material as the safer therapeutic diet at the same viscosity. Therefore, further studies are needed that focus on VFSS protocols that include sour taste and on its adequacy.
This study also had other limitations. First, the participants performed each liquid test only twice. We could not perform each session more often due to the ethics related to radiation exposure. Second, we did not compare the results with other tastes. Further studies with various gustatory stimulations are needed. Third, the gag reflex is often used as the clinical assessment of dysphagia and a deficit of pharyngeal sensation has been known as the sensitive predictor of aspiration in acute stroke.23 If these factors were included in our study, it would be more meaningful research. However, we did not investigate with them in this study. Further studies are needed focused on these factors.
References
1. Martin-Harris B, Jones B. The videofluorographic swallowing study. Phys Med Rehabil Clin N Am. 2008; 19:769–785. PMID: 18940640.

2. Ozaki K, Kagaya H, Yokoyama M, Saitoh E, Okada S, Gonzalez-Fernandez M, Palmer JB, Uematsu AH. The risk of penetration or aspiration during videofluoroscopic examination of swallowing varies depending on food types. Tohoku J Exp Med. 2010; 220:41–46. PMID: 20046051.

3. Lee KL, Kim WH, Kim EJ, Lee JK. Is swallowing of all mixed consistencies dangerous for penetration-aspiration? Am J Phys Med Rehabil. 2012; 91:187–192. PMID: 22019974.

4. Chee C, Arshad S, Singh S, Mistry S, Hamdy S. The influence of chemical gustatory stimuli and oral anaesthesia on healthy human pharyngeal swallowing. Chem Senses. 2005; 30:393–400. PMID: 15829608.

5. Ding R, Logemann JA, Larson CR, Rademaker AW. The effects of taste and consistency on swallow physiology in younger and older healthy individuals: a surface electromyographic study. J Speech Lang Hear Res. 2003; 46:977–989. PMID: 12959474.
6. Kajii Y, Shingai T, Kitagawa J, Takahashi Y, Taguchi Y, Noda T, Yamada Y. Sour taste stimulation facilitates reflex swallowing from the pharynx and larynx in the rat. Physiol Behav. 2002; 77:321–325. PMID: 12419408.

7. Logemann JA, Pauloski BR, Colangelo L, Lazarus C, Fujiu M, Kahrilas PJ. Effects of a sour bolus on oropharyngeal swallowing measures in patients with neurogenic dysphagia. J Speech Hear Res. 1995; 38:556–563. PMID: 7674647.

8. Pelletier CA, Lawless HT. Effect of citric acid and citric acid-sucrose mixtures on swallowing in neurogenic oropharyngeal dysphagia. Dysphagia. 2003; 18:231–241. PMID: 14571326.

9. Jin Y, Sekizawa K, Fukushima T, Morikawa M, Nakazawa H, Sasaki H. Capsaicin desensitization inhibits swallowing reflex in guinea pigs. Am J Respir Crit Care Med. 1994; 149:261–263. PMID: 7509247.

10. Nilsson B. Taste acuity of the human palate. I. Studies with electrogustometry and taste solutions on young adults. Acta Odontol Scand. 1977; 35:51–62. PMID: 265675.

11. Sato K, Endo S, Tomita H. Sensitivity of three loci on the tongue and soft palate to four basic tastes in smokers and non-smokers. Acta Otolaryngol Suppl. 2002; (546):74–82. PMID: 12132625.

12. Ujiie Y, Sekizawa K, Aikawa T, Sasaki H. Evidence for substance p as an endogenous substance causing cough in guinea pigs. Am Rev Respir Dis. 1993; 148:1628–1632. PMID: 7504893.

13. Gu Q, Lee LY. Airway irritation and cough evoked by acid: from human to ion channel. Curr Opin Pharmacol. 2011; 11:238–247. PMID: 21543258.

14. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–98. PMID: 8721066.

15. Power ML, Hamdy S, Singh S, Tyrrell PJ, Turnbull I, Thompson DG. Deglutitive laryngeal closure in stroke patients. J Neurol Neurosurg Psychiatry. 2007; 78:141–146. PMID: 17012336.

16. Stephen JR, Taves DH, Smith RC, Martin RE. Bolus location at the initiation of the pharyngeal stage of swallowing in healthy older adults. Dysphagia. 2005; 20:266–272. PMID: 16633870.

17. Logemann JA. Preswallow sensory input: its potential importance to dysphagic patients and normal individuals. Dysphagia. 1996; 11:9–10. PMID: 8556885.

18. Nakazato M, Endo S, Yoshimura I, Tomita H. Influence of aging on electrogustometry thresholds. Acta Otolaryngol Suppl. 2002; (546):16–26. PMID: 12132616.

19. Palmer JB, Drennan JC, Baba M. Evaluation and treatment of swallowing impairments. Am Fam Physician. 2000; 61:2453–2462. PMID: 10794585.
20. Hamdy S, Rothwell JC, Aziz Q, Singh KD, Thompson DG. Long-term reorganization of human motor cortex driven by short-term sensory stimulation. Nat Neurosci. 1998; 1:64–68. PMID: 10195111.

21. Logemann JA, Veis S, Colangelo L. A screening procedure for oropharyngeal dysphagia. Dysphagia. 1999; 14:44–51. PMID: 9828274.

22. Kaatzke-McDonald MN, Post E, Davis PJ. The effects of cold, touch, and chemical stimulation of the anterior faucial pillar on human swallowing. Dysphagia. 1996; 11:198–206. PMID: 8755466.

23. Davies AE, Kidd D, Stone SP, MacMahon J. Pharyngeal sensation and gag reflex in healthy subjects. Lancet. 1995; 345:487–488. PMID: 7861875.

Table 3
Improvement of the PAS Scores for Lemon Juice with Barium
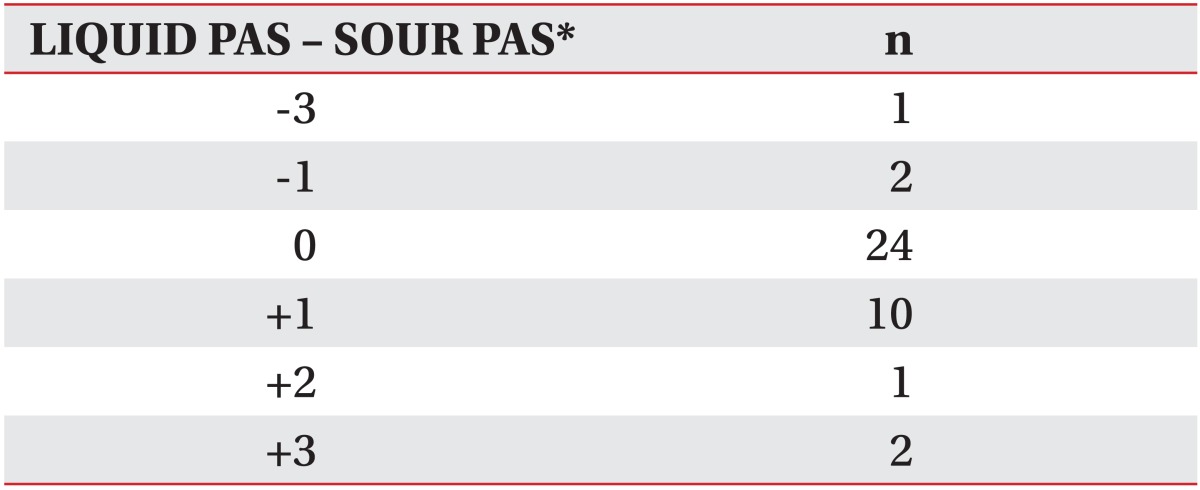
PAS: Penetration-Aspiration Scale, LIQUID PAS: Penetration-Aspiration Scale score of thin liquid barium, SOUR PAS: Penetration-Aspiration Scale score of lemon juice with barium
*It means subtracting the Penetration-Aspiration Scale score of lemon juice with barium from the Penetration-Aspiration Scale score of thin liquid barium. The positive (+) means the improvement of the Penetration-Aspiration Scale score with lemon juice with barium and the negative (-) means the reverse




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download