INTRODUCTION
Brucellosis, a zoonosis with a systemic infection caused by facultative intracellular bacteria of the genus
Brucella. Brucella species are transmitted by direct contact with infected animals or by the consumption of products from infected animals.
1-
3 Each year, half a million new cases are reported worldwide, but according to the World Health Organization (WHO), these numbers greatly underestimate the true incidence of human disease.
4 Brucellosis affects the entire body, including various human organs, the musculoskeletal system and the reticuloendothelial system. Osteoarticular manifestations are the most frequent and severe complications, but it is difficult to diagnose because its clinical symptoms are variable and non-specific.
5 The disease is a major public health problem in the Mediterranean region, the Middle East, and Latin America but is rare in Korea.
2,
6 However, due to an increase in overseas travel, it has been introduced to Korea and its incidence rate is on the rise.
5 Brucellar spondylitis was first described by Kulowski and Vinke in 1932, and it is one of the most serious complications of brucellosis.
7 However, Brucellosis has rarely been reported in Korea. Therefore, the brucellar spondylitis is quite rare. We present a case of brucellar spondylitis as the cause of non-specific back pain in a patient that works as a farmer, with a review of the relevant literature.
Go to :

CASE REPORT
A 52-year old male patient was admitted to the Department of Rehabilitation Medicine at our hospital with a complaint of severe sudden back pain and a radiating pain in the right lower extremity, which had gradually developed for 2 months prior to the visit. His medical history revealed that he had partial gastrectomy because of a gastric adenocarcinoma that was diagnosed about 3 years ago, and he was being treated with oral medication for his type 2 diabetes, which was diagnosed about 1 month ago. He had no medical history of diseases including hypertension, tuberculosis or hepatitis. He also had no recent history of overseas travels or eating raw meat, and there was no evidence of specific family history. The patient worked as a farmer and also raised cows.
From the physical and neurological examination conducted at the time of his admittance, the patient was found to be normal in the manual muscle power test and the deep tendon reflex of upper and lower extremities on both sides. However, in the sensory test, hypesthesia was found in the L5 dermatome in the right lower extremity. The lumbar range of motion was slightly limited due to the pain in the left lateral flexion, rotation, and the ends of the extension. In the L4 and L5 spinous process, tender points were found, and the degree of pain was found to be 9 out of 10 on the visual analogue scale pain score.
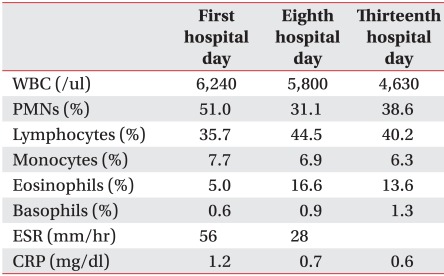
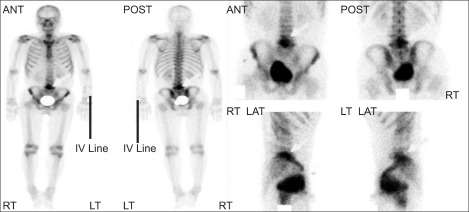
Laboratory findings on the peripheral blood test (
Table 1) showed a raised erythrocyte sedimentation rate (ESR) of 56 mm/hr, and C-reactive protein (CRP) was raised to 1.2 mg/dl. However, no abnormality was observed in other biochemical tests and there were negative findings in the blood culture.
Table 1
The Serial Results Obtained from Laboratory Studies

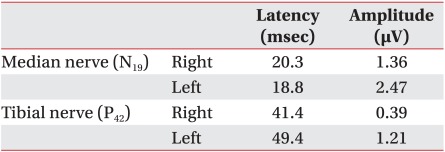
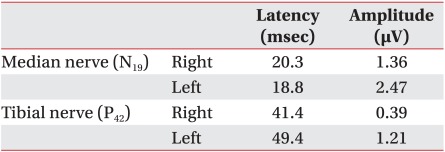
Normal findings were observed in the needle electromyography test, nerve conduction study and sensory evoked potential test (
Table 2), and lumbosacral spine plain radiographs, whole body bone scan, and lumbosacral spine MRI were also conducted. Lumbosacral spine plain radiographs (
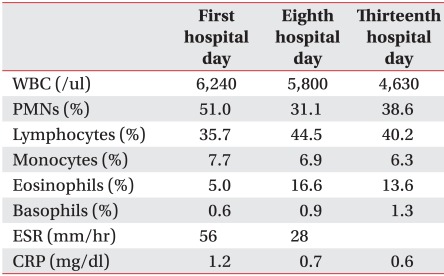
Fig. 1) showed an erosive change of the anterior portion of L4 and L5. Whole body bone scan with 99 mTc dicarboxypropane diphosphonate (DPD) (
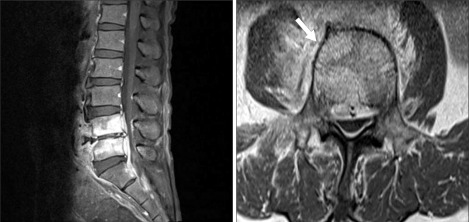
Fig. 2) showed an increased radioisotope uptake in L5. Lumbosacral spine MRI (
Fig. 3) showed low-signal intensity in L4, L5 and S1 vertebral body from the T1 weighted image with contrast enhanced and heterogenous high-signal intensity in T2 weighted image. Also, endplate injury in the anterior portion of L4 and L5 vertebral body and contrast enhanced in nearby soft tissues were observed, indicating the possibility for infectious spondylitis, and L3-4, L4-5 herniation of intervertebral disc findings were observed.
 | Fig. 1A radiograph of the lumbosacral shows a markedly erosive change of the anterior portion of L4 and L5 body. 
|
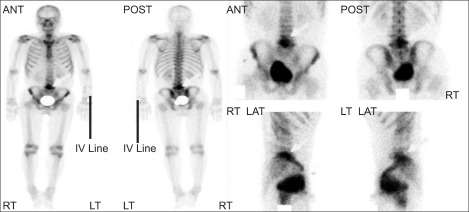 | Fig. 2Whole body bone scan with Tc-99m DPD shows increased radioisotope uptake in L5. DPD: Dicarboxypropane diphosphonate. 
|
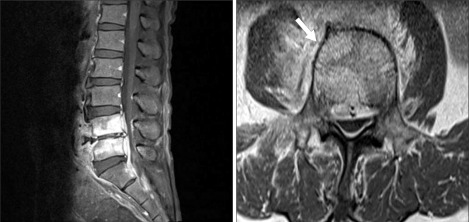 | Fig. 3Lumbosacral spine contrast-enhanced T1-weighted magnetic resonance imaging shows abnormal signal change with enhancement in L4 and L5 body, anterior longitudinal ligament, posterior longitudinal ligament and ligamentum flavum. 
|
Table 2
Somatosensory Evoked Potentials Studies 9 Weeks after Symptom Development

A medical consultation with the Infection Internal Medicine department using CT guided aspiration biopsy, tuberculosis bacillus culture test, molecular genetic testing of tuberculosis bacillus, blood culture test, and brucella antibody test were conducted. The titer of brucella antibody was measured as 1 : 320 and the patient was diagnosed with brucellar spondylitis. He was transferred to the infection internal medicine department and SDR combination therapy mixed with streptomycin, doxycycline and rifampin was injected intravenously 1g daily for 15 days. Following that, 100 mg of it was administered twice a day for 45 days orally, followed by the dosage of 15 mg/kg (600-900 mg/day) being administered once a day orally for 45 days. The follow-up observation reported improved symptoms and back pain.
Go to :

DISCUSSION
Human brucellosis, caused by small Gram negative, aerobic coccobacilli of the genus brucella is a zoonotic infection and is transmitted most commonly through the ingestion of unpasteurized milk products such as cheese or raw liver, or by direct contact with infected animals.
3 Species that cause human brucellosis are
Brucella melitensis,
B. abortus,
B. suis and
B. canis,
1 and in Korea,
B. abortus is found most frequently.
After entering the human body and being taken up by local tissue lymphocytes, Brucellae are transferred through regional lymph nodes into the circulation and are subsequently seeded throughout the body, with tropism for the reticuloendothelial system.
4 Symptoms are non-specific and can include fever, headache, back pain, myalgias, and fatigue.
5,
6 Because of the non-specific symptoms of this disease and difficulty in distinguishing it from other infectious spondylitis diseases on MRI, suspicious patients with a history of direct contact with infected animals or consumption of their products is important for early diagnosis and treatment.
1,
4
Brucellosis may affect various body organs, but spondylitis is the most frequent and significant complication of brucellosis and the reported incidence varies from 2-60%.
1,
5,
6 Lumbar vertebrae are the most frequently involved regions in brucellar spondylitis, followed by thoracic and cervical segments.
1
Definite diagnosis of brucellosis is established by clinical manifestations and the isolation of Brucella species from blood or bone marrow cultures,
1,
6,
7 but this is very difficult for patients with chronic brucellosis or local complications.
2 In the absence of bacteriologic confirmation, a positive serology for brucella standard tube agglutinin testing (titer over 1 : 160), a 4-fold rise in brucella-antibody titer in the interval of 2 weeks, is considered definitive.
6 However, there is the limitation that the sensitivity drops in the early stage of the disease and thus, repeated antibody tests are important.
6 Another test is the indirect enzyme linked immune sorbent assay (ELISA). It uses cytoplasmic proteins as antigens and measures immunoglobulins class M, G, and A, which allows for a better interpretation of the clinical situation and overcomes some of the shortcomings of the serum agglutination tests. A comparison with the serum agglutination test yields higher sensitivity and specificity.
4 The development of a specific polymerase chain reaction (PCR) is a recent advancement. PCR is fast, can be performed on any body tissue, and can yield positive results as soon as 10 days after inoculation.
4 Although PCR and ELISA offer new possibilities in the future for diagnosing brucellosis, standardization of extraction methods and set up is lacking, and a better understanding of the clinical significance of the results is still needed.
4
Routine laboratory data reported in most studies have been of little diagnostic value. Hemogram and ESR are not useful indicators for the diagnosis of brucellar spondylitis. However, the increase of ESR has been observed in a majority of case reports, which may be considered as a useful measure for assessing the response to therapy. Generally, CRP was within the normal range,
1,
8 but in this patient, increased to 1.2 mg/dl and this was considered an abnormal increase due to his medication for diabetes and pain. Plain radiographs can show various degrees of bone involvement, with narrowing of the intervertebral disc space, gross destruction, patchy sclerosis of the vertebral end plateau, syndesmophytes with or without paravertebral noncalcified soft tissue swelling, or displacement of the vertebral axis.
9 As the earliest appearances of the destructive changes visible on plain radiographs begin approximately 3 months after the onset of symptoms, magnetic resonance imaging, which is more sensitive to demonstrate early bone infection, should be considered.
4
In patients who stayed in certain endemic areas, tuberculous or brucella infections of the spine can be confused. Both are caused by intracellular pathogens which are difficult to isolate or identify in a short period.
4 For this reason, differential diagnosis between spinal brucellosis and vertebral tuberculosis is usually made on the basis of clinical and routine laboratory and radiological findings.
9 Leukocyte count and ESR are relatively lower in brucellar spondylitis than in tuberculous spondylitis.
9 In addition, The brucellar spondylitis lesion may be unifocal or multifocal on MRI. This disease has a predilection for the lower lumbar spine, and intact vertebral architecture and diffuse vertebral osteomyelitis, disc space involvement, minimal paraspinal soft tissue involvement, and absence of gibbus deformity are features that suggest brucellar spondylitis over other pyogenic spondylitis and tuberculous spondylitis.
10 On the other hand, the characteristic features of tuberculous spondylitis include the involvement of a single vertebra or disc, predilection for the midthoracic region, severe vertebra body collapse, extensive associated paraspinal abscess, and gibbus deformity. In contrast to spinal involvement in brucellosis, tuberculous spondylitis is commonly seen in younger patients.
8
There is no standard recommended treatment regimen and various combinations of antibiotics can be used to treat brucellar spondylitis. SDR combination therapy is the most effective regimen for reducing failure and relapse rates.
7 Brucellar spondylitis is one of the rare complications of brucellosis in Korea and its symptoms are non-specific, which makes differential diagnosis difficult. Especially in Korea, tuberculosis is an endemic disease. Therefore, for diff erential diagnosis of patients suspected of brucellar spondylitis with other spine disorders or tuberculous spondylitis, detailed medical history, MRI, and serum test should be conducted for early diagnosis and treatments. We present a rare case of brucellar spondylitis as the cause for non-specific back pain, with a review of the relevant literature.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download