Abstract
Objective
To evaluate quality of life (QOL), upper extremity function and the effect of lymphedema treatment in patients with breast cancer related lymphedema.
Method
The basic data comprised medical records (detailing age, sex, dominant side, location of tumor, cancer stage, operation record, cancer treatment and limb circumferences) and questionnaires (lymphedema duration, satisfaction, self-massage). Further to this, we measured upper extremity function and QOL, administered the DASH (Disabilities of Arm Shoulder and Hand outcome measure) and used the EORTC (European Organization for Research and Treatment of Cancer)-QLQ-C30 and the EORTC-QLQ-Br23. Results of these were calculated as main outcome variables.
Results
The questionnaire responses and arm circumferences of 59 patients with breast cancer related lymphedema were analyzed. In the DASH questionnaire, it was found that the older the lymphedema patient was, the lower their upper extremity function. On the EORTC-QLQ, patients with metastasis had significantly lower scores in physical functioning and role functioning. In terms of upper extremity circumference, there was a significant upper extremity size reduction after lymphedema treatment.
Conclusion
There were several dissociations between some subscales of quality of life questionnaires and those of upper extremity functions. Upper extremity function was correlated with the age of breast cancer patients and QOL was influenced by M-stage. Lymphedema treatment was found to be effective in reducing edema in patients with breast cancer related lymphedema.
Go to : 
Upper extremity lymphedema is a chronic complication that appears frequently after breast cancer treatment. It is not only a disease that causes cosmetic problems, but also one that exerts effects on psychosocial adjustment, quality of life and functional status. In part related to growing obesity levels, a westernization of diet habits and a decrease in breast feeding, the incidence of breast cancer is the highest of all female cancers.
Given this, interest in lymphedema has developed concurrent to a rise in breast cancer treatment. In its initial period, the disease involves a swollen sensation or mild discomfort in the upper extremities, and as it progresses, symptoms such as a limitation of joint motion, pain, and skin discoloration develop and the risk of infection increases.
Lymphedema is a factor that mediates significant effects on the function of upper extremities as well as quality of life after breast cancer surgery. Thus lymphedema treatments, quality of life and upper extremity function after treatment have been frequently studied.
Among the current treatments for lymphedema, complex decongestive physical therapy (CDT) is the most common. CDT includes education on skin care to prevent infection, manual lymphatic drainage that accelerates the drainage of excess lymph fluids, non-elastic bandaging to maintain the decreased edema by elevating tissue pressure, and special exercise therapy to accelerate the drainage of lymph fluid by muscle contraction and to enhance the range of joint motion.1 The method that has been applied most widely to assess treatment outcomes is to measure the circumference reduction in certain areas of the affected arm. Additional methods include evaluating the reduction of the affected arm's volume by immersing it in water and then measuring the volume of overflowed water, and measuring the tension in the affected tissue.
Studies on quality of life and upper extremity function after breast cancer treatment have been frequently conducted, and it has been reported that quality of life in lymphedema patients is lower than in those patients without the condition.2 However, studies that consider both quality of life and upper extremity function within a patient group that has received treatment for lymphedema are rare.
In this study, the capacity of lymphedema therapies to reduce lymphedema was assessed, alongside survey results on quality of life and upper extremity function according to the demographic information of lymphedema patients. This will allow us to apply this information as a clinical index for treatment outcomes of lymphedema that had developed after breast cancer surgery, measuring both quality of life and upper extremity function.
Go to : 
134 patients were treated with CDT for breast cancer related lymphedema from January 2007 to March 2010 at department of rehabilitation medicine, Seoul National University Hospital in Seoul, South Korea. Of these, 64 patients visited the rehabilitation outpatient clinic from 11th May 2010 to 14th June 2010. After agreement, 59 patients responded to the survey and filled out the questionnaires independently.
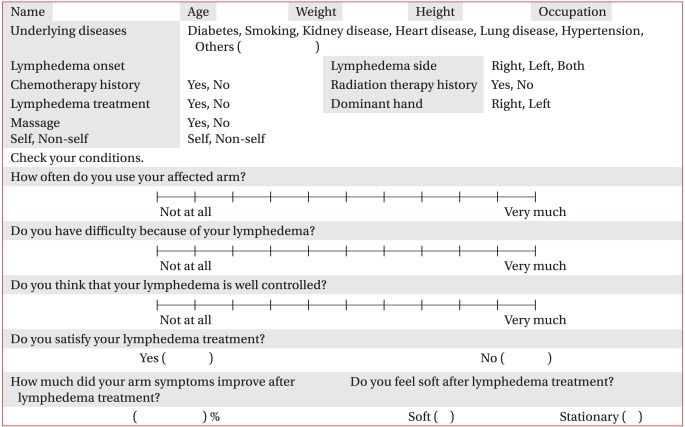
To evaluate quality of life after lymphedema treatment, a questionnaire survey was conducted applying the European Organization for Research and Treatment of Cancer (EORTC)-QLQ-C30 and the EORTC-QLQ-Br23, which were designed for breast cancer patients. For the evaluation of upper extremity function, the short version of the Disabilities of Arm Shoulder and Hand outcome measure (DASH) was applied. The onset of the development of lymphedema, the dominant arm, and patients' satisfaction level with their breast cancer and lymphedema treatments, as well as whether or not self-massage was being performed at home were assessed by a questionnaire that was designed for this study (Appendix 1).
In the EORTC-QLQ-C30, there are subcategories of global health status, function scale and symptom scale. Physical functioning, role functioning, emotional functioning, cognitive functioning, social functioning are assessed in the function scale, whereas fatigue, nausea and vomiting, pain, dyspnea, insomnia, appetite loss, constipation, diarrhea, and financial difficulty are assessed in the symptom scale. The EORTC-QLQ-Br23 also consists of function scale and symptom scale. Body image, sexual functioning, sexual enjoyment and future perspective are assessed in the function scale, whereas systematic therapy side effects, breast symptoms, arm symptoms and emotional response to hair loss are assessed in the symptom scale.
Medical records were reviewed between April 2010 and May 2010, similar to the period in which we acquired questionnaire responses. This allowed us to obtain the information about those subjects who responded to the questionnaire, i.e., their age, gender, whether or not their lesion was in the dominant arm, cancer stage, surgical records and whether or not chemotherapy, radiotherapy or hormone therapy had been performed. Based on this data, alongside results from the EORTC-QLQ-C30, the EORTC-QLQ-Br23, and the K-DASH, the demographic characteristic of subjects as well as the factors related with breast cancer were evaluated to assess the associations between quality of life and upper extremity function.
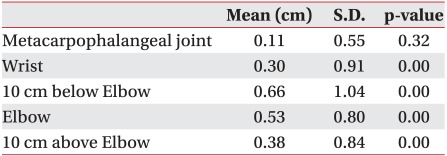
To assess improvements in lymphedema after treatment, measurement of the circumference of the upper arm was carried out. At the metacarpophalangeal joints, the wrist, 10 cm below the elbow, at the elbow, and 10 cm above the elbow level, the circumference was measured horizontally by rulers. Records of circumference measurement prior to and after lymphedema treatments performed both at outpatient clinics and in the physical therapy room were used. Lymphedema treatment for each patient comprised two weeks of complex decongestive physical therapy (CDT). They received skin care, manual lymphatic drainage, compression bandaging, and undertook an exercise regime for 30 minutes a day, five days a week.
For statistical analysis, SPSS 18.0 was used. To analyze whether the demographic characteristics and the factors pertinent to breast cancer were related with questionnaire results measuring quality of life and upper extremity function, multiple regression analysis, Kruskal Wallis Test and Mann-Whitney U test were applied. To assess the effect of lymphedema treatment, the circumference of arm data were analyzed by Paired Samples t-Tests.
Written informed consent was obtained prior to the study from all subjects. The study was performed in accordance with the principles set forth in the Declaration of Helsinki.
Go to : 
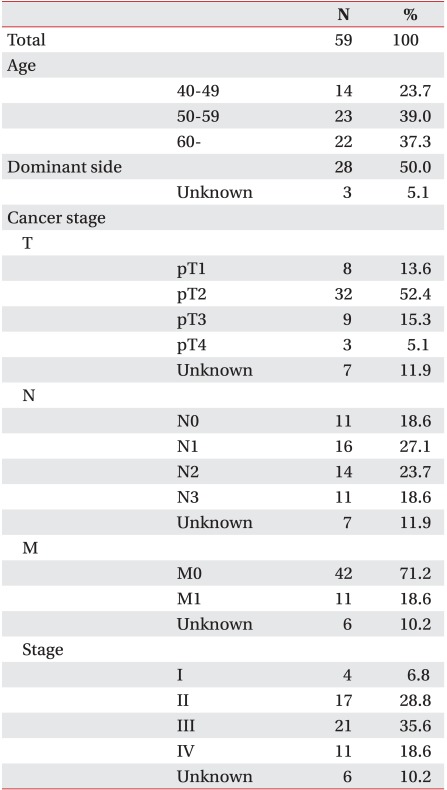
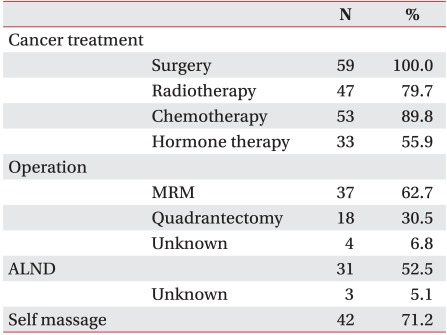
Out of the 134 patients who received CDT for breast cancer related lymphedema from January 2007 to March 2010 and the 64 patients who visited the rehabilitation outpatient clinic between 11th May 2010 and 14th June 2010, 59 patients filled out the EORTC-QLQ-C30, the EORTC-QLQ-Br23 and the K-DASH questionnaire. There were seven patients with shoulder pain and axillary web syndrome, which can affect upper extremity functions. In terms of average age, 14 patients were in their 40s (23.7%), 23 in their 50s (39.0%), and 22 patients were in their 60s or above (37.3%). The mean age was 56.31±9.49 years. The average duration of lymphedema was 4.21±2.11 years (Table 1). Concerning breast cancer treatments, all patients had undergone surgical treatment, with radiation therapy being given to 47 patients (79.7%), chemotherapy to 53 patients (89.8%), and hormonal therapy to 33 patients (55.9 %) (Table 2).
DASH questionnaire results were analyzed, considering patients' age, the lesion side of breast cancer, the disease stage of breast cancer, whether or not axillary lymph node dissection was performed during surgery, whether or not chemotherapy, radiation therapy or hormone therapy had been performed, the duration of lymphedema, the satisfaction level with treatments, and whether or not self-massage was being performed at home.
Considering the correlation between age and K-DASH scores, it was found that the older the patient was, the lower their upper limb function (Regression coefficient: -0.834, p-value: 0.012), but the duration of lymphedema and postoperation period were not significantly correlated with age. In addition, no significant relation was found between upper extremity function and lesion side, axillary lymph node dissection having been performed, a history of chemotherapy, radiation therapy or self-massage, and treatment satisfaction level. There was also no significant difference in K-DASH scores between patients with shoulder pain and those without (p-value: 0.263).
The EORTC questionnaire was used to measure this. As with the survey of upper extremity function, based on the general demographic characteristic of patients and the factors associated with breast cancer, quality of life results were analyzed.
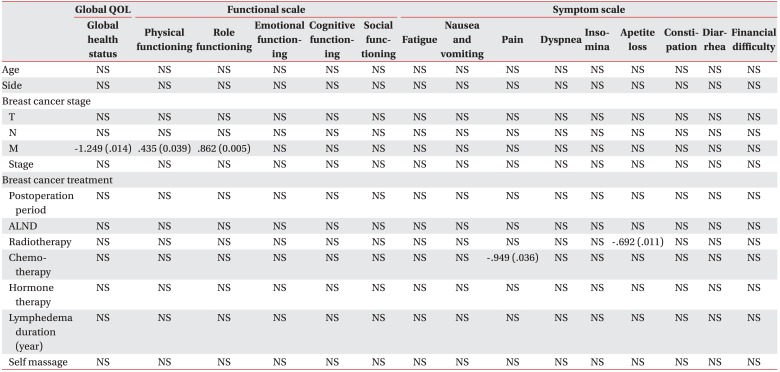
In EORTC-QLQ-C30, the global health status of metatstatic cancer patients was lower than that of non-metastatic patients. Physical functioning and role functioning were also similarly correlated with metastatic breast cancer patients. Emotional functioning, cognitive functioning and social functioning were, however, not correlated with any demographic factors, breast cancer factors or treatments factors. Other symptom scales, including pain and appetite loss showed some correlations (Table 3).
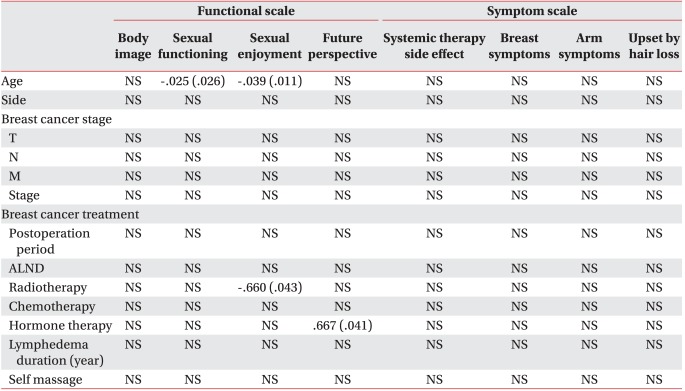
In EORTC-QLQ-Br23, sexual functioning, sexual enjoyment were negatively correlated with age. Future perspective was lower in patients who had undergone hormone therapy. Body image, systemic therapy side effects, breast symptoms, arm symptoms and response to hair loss were not correlated with any demographic factors, breast cancer factors or treatment factors (Table 4). Additionally, there was no significant relationship found between shoulder pain and quality of life in the EORTC-QLQ-C30 or the EORTC-QLQ-Br23 results, except for the pain item (p-value: 0.0014).
For the upper extremity function questionnaire, the K-DASH, there were significant correlations with patient age. For the two QOL questionnaires, there were also significant correlations with the presence of metastasis, and some with age, particularly related to sexual functioning. No other factors investigated in this study were significantly correlated with questionnaire results (the lesion side of breast cancer, the disease stage of breast cancer, whether or not axillary lymph node dissection was performed during surgery, whether or not chemotherapy, radiation therapy or hormone therapy, treatment satisfaction level, and whether or not self-massage was being performed at home).
After two weeks of CDT treatment, pre-treatment and post-treatment patient arm circumferences were compared. Paired sample t-tests were performed and the results showed that circumference at every level, i.e. the circumference at the wrist level, at 10 cm below the elbow, at the elbow, and 10 cm above the elbow level, was significantly reduced after l treatment (Table 5).
Go to : 
The lymphatic system is the system that collects lymph fluid from the skin, subcutaneous tissues, muscles, bones and other tissues and circulates it to blood vessels. Lymph fluid consists of water, proteins and cell debris. As lymph fluid within lymph ducts circulates to blood vessels, the body maintains optimal conditions. However, in patients with breast cancer, the lymphatic system active in the breast area is destroyed by surgery or other treatment for breast cancer, which then prevents lymph fluid circulating into blood vessels and leads it to enter adjacent tissues and to raise oncotic pressure. Consequently, edema is developed due to the migration of water into tissues.1
Treatment for lymphedema causes a reduction of edema by facilitating lymphatic circulation. Good reduction in lymphedema through treatment of lymphedema after breast cancer treatment has taken place has been reported by several studies with wide reduction ranges from 20% to 80%.3-5 It appears that the degree of reduction may be different according to the method of assessing lymphedema and the difference of the time interval between pre-treatment and post-treatment measurement. In our study, it was also observed that the level of lymphedema was reduced after lymphedema treatments.
Different from the results for upper extremity function, in the survey assessing quality of life, M stage was shown to be a significant parameter affecting quality of life. The difference of quality of life according to the presence or absence of breast cancer metastasis has been reported by several studies. In some studies, it has been stated that breast cancer metastasis is associated with depression and overall quality of life, and it has also been reported that the recurrence of breast cancer strongly lowered the quality of life of patients, and even their guardians.6,7 This appears to be due to a fear of additional metastasis as well as the burden of additional treatments after metastasis. In addition, it has been reported that the fear of recurrence becomes, in itself, a source of stress for patients.8
It is well known that lymphedema treatments have a reduction effect on edema. Nevertheless, it has been claimed that a reduction in the size of the upper extremities in which edema has developed is associated neither with the quality of life nor with the upper extremities function, but rather the presence or absence of edema is more important than the size of edema.2 In addition, it has been also reported that quality of life is not significantly associated with physical functions.9-11 The satisfaction level with treatments is a part of subjective evaluation based on patients' personal experiences, and quality of life is also a subjective construct that includes financial and the environmental factors as well as those related to treatment. In this study, the quality of life survey and the one relating to upper extremity function showed different distributions by category. Therefore, it can be proposed that when assessing the treatment of lymphedema, quality of life and upper extremity function should be evaluated from different aspects.
One of the limitations of this study is that it was a cross-section study which examined quality of life and the functional impairment of upper extremities in breast cancer related lymphedema patients, and thus information about the cause-effect relationships or temporal sequences involved is necessarily limited. In addition, given that it was a retrospective study, additional prospective and longitudinal studies on quality of life and upper extremity function in breast cancer related lymphedemapatients may be required. It is also necessary to develop treatments and programs that can improve of quality of life and upper extremity function in subjects, alongside a reduction in edema.
Go to : 
In terms of upper extremity function, it was found that older breast cancer related lymphedema patients had a lower level of upper extremity function than younger counterparts. Patients with metastasis had significantly lower quality of life scores on the physical and role functioning subscales. Upper extremity function was not significantly associated with quality of life. In addition, it was found that the currently most-used lymphedema treatment was successful in reducing edema.
Go to : 
References
1. Warren AG, Brorson H, Borud LJ, Slavin SA. Lymphedema: a comprehensive review. Ann Plast Surg. 2007; 59:464–472. PMID: 17901744.
2. Dawes DJ, Meterissian S, Goldberg M, Mayo NE. Impact of lymphoedema on arm function and health-related quality of life in women following breast cancer surgery. J Rehabil Med. 2008; 40:651–658. PMID: 19020699.

3. Ko DS, Lerner R, Klose G, Cosimi AB. Effective treatment of lymphedema of the extremities. Arch Surg. 1998; 133:452–458. PMID: 9565129.

4. Boris M, Weindorf S, Lasinski B, Boris G. Lymphedema reduction by noninvasive complex lymphedema therapy. Oncology (Williston Park). 1994; 8:95–106. PMID: 7993730.
5. Casley-Smith JR. Modern treatment of lymphoedema. I. Complex physical therapy: the first 200 Australian limbs. Australas J Dermatol. 1992; 33:61–68. PMID: 1294054.

6. Slovacek L, Slovackova B, Slanska I, Petera J, Priester P. Quality of life and depression among metastatic breast cancer patients. Med Oncol. 2010; 27:958–959. PMID: 19771532.

7. Slovacek L, Slovackova B, Slanska I, Petera J, Priester P, Filip S, Kopecky J. Depression symptoms and health-related quality of life among patients with metastatic breast cancer in programme of palliative cancer care. Neoplasma. 2009; 56:467–472. PMID: 19873686.

8. Northouse LL, Mood D, Kershaw T, Schafenacker A, Mellon S, Walker J, Galvin E, Decker V. Quality of life of women with recurrent breast cancer and their family members. J Clin Oncol. 2002; 20:4050–4064. PMID: 12351603.

9. Kelly MH, Brillante B, Kushner H, Gehron Robey P, Collins MT. Physical function is impaired but quality of life preserved in patients with fibrous dysplasia of bone. Bone. 2005; 37:388–394. PMID: 15963775.

10. Robbins RA, Simmons Z, Bremer BA, Walsh SM, Fischer S. Quality of life in ALS is maintained as physical function declines. Neurology. 2001; 56:442–444. PMID: 11222784.

11. Bossier R. Physical function and health-related quality of life in culturally diverse elders: evidence of environmental press [dissertation]. 2005. The Department of Kinesiology: Louisiana State University.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download