DISCUSSION
In patients with stroke, cerebral palsy, cervical spinal cord injury, increased spasticity of elbow flexor may cause adverse effect on daily performance and walking balance. To solve this spasticity of the elbow flexor, several treatment methods have been developed, for example, physical therapy, orthotics, medication, and injection therapy and so on. These injection methods, used commonly, are nerve branch or motor point block using phenol and motor point (neuromuscular junction) block using botulinum toxin, which is used popularly in recent practices.
9,
13-
19
In Korea, prior to the studies of the motor points of the upper arm, the research for describing the motor points of gastrocnemius and soleus muscles have been reported. Kim et al.
7 reported that the first motor point of the medial gastrocnemius muscle was located at 5.0%, the second was at 16.0%, the first motor point of lateral gastrocnemius was located at 10.0%, the second was at 16.0%, the first motor point of soleus muscle was located at 18.0% and the last motor point at 19.0% of the lower leg length. Further, Kim et al.
8 reported that the first motor point of the medial gastrocnemius muscle was located at 9.6%, the last at 37.5% and the first motor point of lateral gastrocnemius was located at 12.0%, the last was at 37.9% and the first motor point of soleus muscle was located at 20.5%, as well as the last motor point at 46.7% of the lower leg length. The reason why there are differences in the results of both studies may be associated with the different definition of the motor point in the two researchers. Kim et al.
7 defined the motor point as the area where the motor nerve branch enters into the muscle (macroscopic entry into the muscle), however Kim et a1.
8 defined the motor point as the point where the intramuscular motor nerve branch was tracked so deep that the branch could not be separated from the muscles (microdissection). Kim et al.
8 differentiated their definition because of the fact that anatomically, the motor point were dense regions of the motor endplates, which were the end regions of the motor nerve fiber and the motor endplates were formatted after a big myelinated motor nerve axon that approached the muscle was divided into multiple smaller branches, and which traveled along the surface of the muscle for a certain distance. They also considered that the location of the motor point in observing anatomically, where the motor nerve branch enters into the muscle with the naked eyes, was different from that of the motor point in the electrical diagnostics. In clinical practice, the motor point could be found by inserting the needle into the muscle, where maximum muscle contraction can be caused by the minimum stimulus after searching the region of the response that was the most remarkable in electrical stimulation on the skin surface around the area, which has the most tension in palpation or the area where the muscle seemed swollen visually or around the standard insertion area of the needle EMG. But so far, there has not been any specific method for practicing or any quantitative standard for positioning of the motor point.
20 So Ko et al.
20 attempted the objective and standardized mapping on the surface of the skin via electrical stimulation for easy access of the motor point. Ko et al.,
20 using EMG devices, stimulated the posterior tibial nerve electrically at the popliteal area and recorded the evoked compound muscle action potentials of triceps of the lower leg and defined the motor point as the area where the maximum amplitude appeared, and then they reported that the motor point of the medial gastrocnemius muscle was located at 41.0%, the lateral gastrocnemius at 35.7%, the soleus at 68.6% of the lower leg length from proximal to distal. This result showed that the discrepancies of the location of the motor point exist between in the cadaver dissection study and in the surface mapping study. We think that this result show that the motor point of microdissection study, in which the motor point was described after tracking the motor nerve branch as much as possible, could be closer to the location of the motor point based on the anatomic definition - the crowded area of the motor endplates, which are the end of motor nerve fiber - rather than the motor point in the study in which motor point was defined as the first area for the motor nerve branch to enter into the muscle. Furthermore, we think that the result suggests that the study method of Ko et al.
20 may be a more reasonable way to find the dense area of the motor endplates, rather than the cadaver dissection studies. In addition, we think it is necessary to vary the access to the motor point, according to which block is performed in the phenol or botulinum toxin. As such, we think that in the case of phenol block, it is reasonable to refer to the location of the motor point in the earlier cadaver studies, since we believe that when practicing the whole nerve block, the motor branch block, the motor point block using phenol,
16 according to the patient's conditions, both the first point for the motor nerve to enter into the muscle (macroscopic entry into the muscle) and the point for intramuscular branch to enter into the muscle after being tracked maximally (microscopic entry into the muscle), are expected to produce some sufficient clinical effects. In other words, the motor point, in the cadaver dissection study (the first area for the motor nerve or motor nerve branches to enter into the muscle), which is thought to be located proximally to the motor endplates, is a valid position for phenol block. Clinically, we believe that in phenol block, the nerve conduction devices using EMG needle is necessary. However, this information in the cadaver dissection study can provide the approximate information about the place in which to locate the needle first and this can help to reduce the pain of the patients in addition to giving a time advantage to the practitioners through avoidance of the repeated sticking and make better therapeutic effects. However, we thought that in contrast with motor point block using phenol, crowded areas of the motor endplates that is the target in motor point block using botulilum toxin, could be different from the location of the motor point in the cadaver dissection study. Further, the method by Ko et al.,
20 in which the surface mapping of the motor points were performed using the surface nerve stimulation, could be more of a reasonable method for reflecting the ultimate conditions of the motor endplates. Therefore, we performed our study.
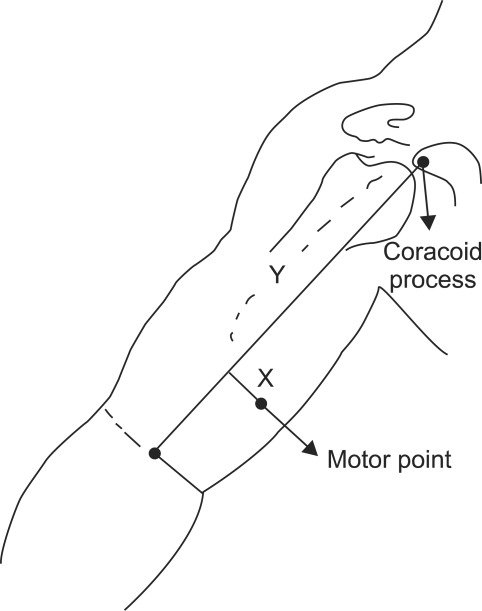
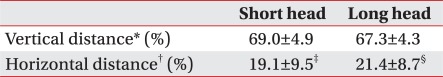
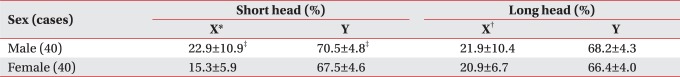
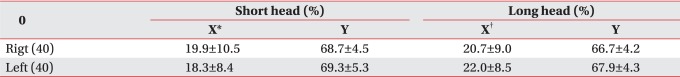
In this experiment, when the vertical length of the upper arm was defined as the length of the line connecting coracoid process and mid-point of the elbow crease along with the horizontal length of the upper arm (upper arm width) as the length of the elbow crease, the motor point of short head and long head of biceps brachii was located at about 2/3 of the vertical length from coracoid process, respectively, and about 1/5 of the half of the horizontal length from the vertical reference line on both sides. When the results of our study compared with the results of other studies, consideration of the disagreement of the motor point might be needed, as in the study of the motor point of the lower leg. In the cadaver dissection studies, when the motor point was defined as the area for the motor nerve or motor nerve branch to enter into the muscle (macroscopic entry into the muscle), Buchanan and Erickson
9 described the motor point of the biceps brachii near 1/2 of the upper arm (53%) in 13 cadaver, 26 arms. Further, Kim et al.
10 reported in the study of 5 cadaver, 9 arms, that the motor points of the biceps brachii were distributed at about 1/2 (first motor point of the short head was located at 47.5%, the second 51.8%, the first motor point of long head was located at 53.0%, the second 57.7%) of the upper arm. In addition, Park et al.11 also reported that the motor point of biceps brachii was observed at about half of the upper extremity (short head 48.24%, long head 53.19%). In our opinion, as in the studies of the motor point of the lower leg, the location of the motor points described in these three studies could be appropriate in the motor point block using phenol. Unlike earlier studies, Lee et al.
12 investigated the area where the points for the motor nerve branches to enter into the muscle (intramuscular motor point) using micro-dissection, were most densely distributed, as well as the area for the motor nerve entering into the muscle (motor entry point) in 30 cadavers, 56 upper limbs. In biceps brachii, they reported that in relation to a reference line, connecting the coracoid process and the medial epicondyle of humerus, the motor entry point was located at 46.1% (short head 44.3%, long head 47.9%) and intramuscular motor points were most densely distributed at a length from 64.6-70.3% from the coracoid process, these results closely match our results. Furthermore, Lee et al.
12 determines the location of the motor endplates through the micro-dissection, but did not confirm by nerve staining.
In addition to the cadaver dissection, there have been attempts to locate the motor endplates of biceps brachii through histological methods. Aquilonius et al.
21 studied the location of the motor endplates of the biceps brachii, through the histological method (whole mount cholinesterase staining), and have reported that the endplates were primarily distributed as a 5-10 mm wide band in a length of 4-6 cm long region that was halfway between the tendons of the muscle. Amirali et al.
22 localized the motor endplate of biceps brachii through the histological method (3 muscles processed by sihler's stain, 2 muscles by acetylcholinesterase stain) and reported that the major motor endplate region was distributed as an inverted V-shaped band, 1 cm in width at about 2/3 of the length of a reference line connecting the acromion and olecranon, the results are similar to those of our study. Studies of the muscle fiber and the location of the motor endplates have been performed mainly through histological methods, Coërs
23 reported that in young children's muscle, motor endplates gathered in the narrow band shape and this motor endplate was always located in the middle of the origin and the insertion point of the muscle fiber, in addition, the shape of this band depends on the texture of the muscle and how the muscle fibers insert, so when the muscle fibers were inserted into the narrow tendon, such as biceps brachii, the band formed more or less a shape of a parabola. In addition, Using histological methods used in the study of Coërs, Christensen
24 conducted the study in stillborns and reported that the direction of the muscle fiber was up to the muscle fiber length and pennation, therefore, in the unipennate muscle, motor endplates formed striped shape in the middle of the muscle, in the bipennate muscle, formed the concave endplates belt shape and the multipennate muscle such as sartorius or gracilis muscle, formed scattered pattern. Biceps brachii muscle was actually two separate unipennate muscles, with fibers running through the whole length of the muscle, except in the medial distal part of the short head some shorter fibers exist, and the endplates form a distinct band through the middle of the two heads, in the short head a smaller endplate band was seen in the distal part of the muscle. Further, Deshpande et al.
25 predicted theoretically the position of the motor endplate by considering pennation, location and orientation, and that in biceps brachii muscle, which was a unipennate fusiform muscle, the motor endplate should form an inverted V-shaped band, slightly below the middle of the humerus. In addition, with respect to the motor endplate of the short and long head, the endplate band of the long head would be a little higher than that of the short head because the fibers of the short head begin a little below and end slightly above that of the long head. This result is consistent with that of our study.
In addition, there have been studies that analyzed the myoelectric signal, which was detected via surface electrodes, when muscle was contracted. Masuda et al.
26 conducted analysis of myoelectric signal from the biceps brachii of 3 subjects, using surface electrode array. They arranged stainless steel, strip electrodes in a 25×4 configuration on an acryl plate, which was molded to fit the shape of the right biceps brachii. Each electrode was 1mm in diameter and 10 mm in length, and they were separated by 5.0 mm in the longitudinal direction and 2.5 mm in the lateral direction. They analyzed myoelectric signal of the biceps brachii that occurred when the force of 40% of the maximum voluntary contraction was given. The neuromuscular junctions of the biceps brachii were located nearly at the middle length of the muscle and distributed in the zone. In 1 subject, neuromuscular junctions occupied a single zone, across the muscle, while the other 2 subjects had 2 parallel zones separated by 10-20 mm. By a similar method, Saitou et al.
27 investigated the distribution of innervation zones of the biceps brachii in 3 subjects by detecting bi-directional propagation of the motor unit action potentials (MUAPs) with the multichannel surface electrode array and they reported that the innervation zones were distributed in a narrow band around the muscle belly. In one subject, the innervation zones in the short head were scattered in a wider band.
In our study, motor point of the short head had slightly more distal position than that of the long head. This matches the prediction of Deshpande et al.
25 However, this is slightly different from the results of Amirali et al.,
22 who showed that the motor endplate band was located at 75% at the lateral edge, 61% at the midline, and 72% at the medial edge when the length of the upper arm was defined as the distance between acromion and olecranon. In regards to the cause of this discrepancy, future research needs to be conducted. In comparison between male and female, the motor point of the short head of the biceps was located more medially and distally, in the male when compared to that in the female. This result might be related to the fact that women have more fat tissue and less muscle tissue than men. However, further study is thought to be needed to confirm this. In our study, when we made a horizontal reference line and a vertical reference line for the surface mapping of motor points in the biceps brachii muscle, we defined the length of the upper arm as the distance between coracoid process and mid-point of the elbow crease. The reason why we set the elbow crease in 90° flexion of the elbow, as the horizontal reference line, was that this could be detected easily in the supine position, and we thought that this could be useful, especially in patients whose arm had flexor synergy, which could make accurate identification of anatomic landmarks technically difficult. The vertical reference line was defined as the line connecting the mid-point of the horizontal reference line and coracoid process since the tip of coracoid process was easier to palpate than the acromion, and a setting like this could help more easily to display two-dimensional location of the motor points, with respect to the injection point of botulinum toxin through the easier distinguishing of the short head and the long head of the biceps brachii. Further, the reason why we used the proportional distance, when setting the coordinates of the motor point, was that we wanted for the results of this study to be available in both groups of adults and children, as it was known that motor innervations was completed in the early childhood days and the location of motor endplates in the adult muscle was correlated with that in the pediatric muscle.
21,
23,
24 In addition, with regards to the stimulating area, the reason why we stimulated the musculocutaneous nerve at above 1/3 of the arm length was that this area would be the most appropriate area to stimulate the nerve, when considering the mileage of musculocutaneous nerve, which exited the brachial plexus then pierced the coracobrachialis muscle then passed between biceps brachii muscle and brachialis muscle then at 1/3 of the arm length, which then produced the first branch to the biceps brachii at 45% of the arm length.
28 In addition, this area was known to be the main route for the block of musculocutaneous nerve.
29 Meanwhile, with regards to erb's point, we thought that it was inappropriate in our study, since the subjects could not bear such repetitive and strong stimulations in that area.
Thus, with regards to the total mileage of musculocutaneous nerve, when putting together the findings of the cadaver dissection studies, the histologic studies, and our study, we could summarize this as the following; after the musculocutaneous nerve came out of coracobrachialis muscle, the nerve branch to the biceps brachii would exit from nerve trunk at about 45% of the arm length
28 then, at about 50% of arm length, would reach the motor point of the biceps brachii, which could be described as a macroscopic entry into the muscle in the cadaver dissection studies.
9-
12 Then the neuromuscular junctions would be formed at near 2/3 of the arm length, which results were showed in our study and also could be compatible with that of the histologic studies.
21-
24 Furthermore, this position could be regarded as the target area for motor point block using botulinum toxin. When practicing the method of motor point block
30 with conventional electromyography equipment, we stimulate target muscle directly, using only cathode with anode fixed to tendon and found a place to produce maximum twitch with the minimum stimulus, then block such points. However, although the actual neuromuscular junctions may be located near the motor point, it will be difficult to say that they are exactly located under the motor point, for actually they are present on each muscle fibers and are spread throughout the muscle.
26 Although finding the location of the motor endplate using electromyography might be possible through observing the spontaneous activity with the characteristic shapes (end-plate activity), this method could be time consuming and ensure great pain to patients. In clinical practice, although the results of our study could not substitute for the motor point block with electromyography, it could be contributed to increase the efficiency and the effectiveness of the motor point block. In addition, the results of our study could be available directly if fixing were difficult as in the block for young patients or asses to EMG equipment were impossible. It is thought that the future studies based on the results of our study, about the specific way of botulinum toxin injection and the subsequent difference of the actual clinical efficacy, will be needed.
The biggest limitation with respect to our experiment is that we could not totally exclude the likelihood that the volume conduction of the deep muscles had contributed to the generation of the compound muscle action potential. In such regard, the future research through the analysis of the waveform of biceps brachii and if possible, including brachialis, is thought to be necessary. In addition, when obtaining the compound muscle action potentials by stimulating the main nerve, inter-trial variation could happen. To reduce this possibility as much as possible, in our study, one author conducted a research, looking at the aspects of the waveforms from the beginning to the end of the test. However, complete exclusion was thought to be impossible. For this, future research using multi-channel recording, etc. should be considered. Further, in the actual clinical application, if considering that the biceps brachii is a superficial muscle, using good resolution ultrasound could be useful.
In addition to motor point block, the results of our study could be very useful for setting insertion site of needle electrode in electromyography, specifying the location of the electrodes in electrical stimulation and performing motor point muscle biopsy in the disease such as myasthenia gravis.
Go to :







 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download