Abstract
Lipedema is a chronic disease of lipid metabolism that results in the symmetrical impairment of fatty tissue distribution and storage combined with the hyperplasia of individual fat cells. Lipedema occurs almost exclusively in women and is usually associated with a family history and characteristic features. It can be diagnosed based on clinical history and physical examination. Lipedema is usually symmetrical, but spares the feet, is often painful to palpation, and is negative for Stemmer's sign. Additionally, lipedema patients can present with microangiopathies and lipomas. The well-known therapies for lipedema include complex decongestive therapy, pneumatic compression, and diet modifications. However, whether these treatments help reduce swelling is debatable. We encountered a case of lipedema that was initially misdiagnosed as lymphedema. The patient's clinical features and history were different from those typical of lymphedema, prompting a diagnosis of lipedema and she was treated with a complex decongestive therapy program.
Lipedema is a chronic disease of lipid metabolism marked by a bilateral and symmetrical swelling of the lower extremities caused by impairment of symmetrical fatty tissue distribution and storage combined with hyperplasia of individual fat cells. It can be diagnosed using clinical features rather than diagnostic tests.1 It almost exclusively affects women and 15% of patients have a family history of lipedema.2 Lipedema occurs primarily in the lower extremities and is rarely accompanied by edema of the upper extremities.1,3,4 Edema of the lower extremities is observed between the pelvic crest and the ankle, and occurs symmetrically on both sides.3 Here, we report a case of lipedema with a review of the literature.
A 60-year-old female patient was admitted to the Department of Gastroenterology, Kosin University Gospel Hospital, for stomach evaluation because esophagogastroduodenoscopic findings at a regular health check-up were suspicious for stomach cancer. After admission, an esophagogastroduodenoscopy, colonoscopy, chest computed tomography scan, abdominal computed tomography scan, and bone scan were carried. No abnormal findings of stomach cancer were observed.
The patient reported a 3-year history of edema of both lower extremities, and was transferred to the Department of Physical Medicine and Rehabilitation for the evaluation and treatment of the lymphedema. The patient had undergone an operation for the fracture of the left tarsal bone 9 years previously and a hysterectomy with bilateral salpingo-oophorectomy due to uterine myoma 4 years previously. At presentation, the patient reported taking metformin (Dae Woong Pham, Seoul, Korea) and glimepirid (Han Mi Pham, Seoul, Korea) for diabetes, and valsartan (Novartis Korea, Seoul, Korea) and amlodipine (MSD Korea, Seoul, Korea) for hypertension. The patient's weight gain started 10 years earlier and the edema of both lower extremities, which showed intermittent improvement and deterioration, appeared 3 years previously. More recently, the edema had continued without any improvement, although the patient did not have any family history related to lower extremity edema.
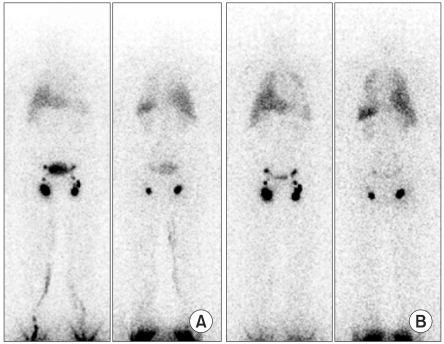
Muscle strength and sensory and muscle stretch reflexes of both the upper and lower extremities were normal on a physical examination that was carried out following transfer of the patient. The circumferences of both lower limbs were measured 10 cm proximal and distal to the lateral condyle of the femur to assess the degree of lower extremity edema (Table 1). Soft edema with negative Stemmer's sign was evident. Obvious differences in both lower extremities were not observed and edema was not evident in the ankles or feet. Upon examination, petechiae were noted in both lower extremities and a lipoma was observed under the right knee joint (Fig. 1, 2). The patient reported tenderness in lower extremities on palpation and, specifically, more severe pain on the outer surface of the left thigh. There were no abnormalities noted upon neurological examination.
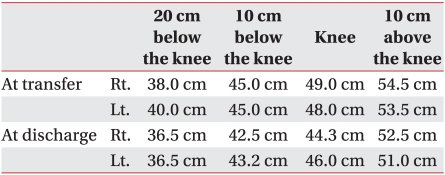
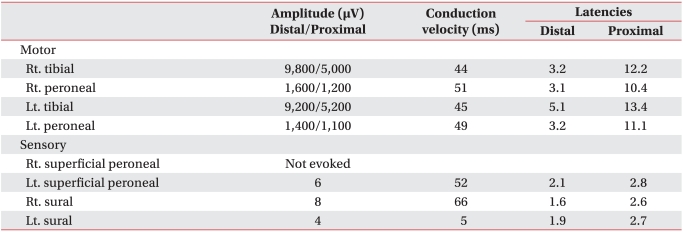
Blood tests for diseases of the thyroid gland, heart, and kidney were all normal. Three-dimensional computed tomography angiography was performed to determine whether the edema was a result of vascular lesions. Vascular lesions, including deep vein thrombosis, were not observed. Technetium-99m human serum albumin lymphangiography was also conducted to assess the presence of lymphedema, but there were no abnormalities (Fig. 3). In addition, motor nerve and sensory nerve conduction studies were performed to identify the cause of the lower extremity pain. The amplitude of the motor nerve action potential for both deep peroneal nerves, which were recorded in the short extensors of the toes, was reduced. There was no nerve action potential in the right superficial peroneal nerve. The amplitude of the sensory nerve action potential was reduced in the left superficial peroneal and both sural nerves. However, it was difficult to diagnose this as clear polyneuropathy as there were no abnormalities in the onset latencies and nerve conduction velocities and there were no denervation potentials on needle electromyography.
We suspected that the absence of, and reduction in, potentials was due to serious edema and the increase in subcutaneous tissue rather than an abnormality of the nerve conduction velocity due to peripheral polyneuropathies because there was no motor or sensory response irregularities except for tenderness on palpation in the neurological exam (Table 2).
We diagnosed the patient with lipedema based on the edema with negative Stemmer's sign that occurred symmetrically in the legs, clinical history, physical exam findings, and other diagnostic test results. Complex decongestive therapy was administered to reduce the edema and pain. Bandaging was not applied due to the patient's pain. Manual lymphatic drainage with low intensity and remedial massage were performed during the first week of treatment. Thereafter, complex decongestive therapy including bandaging was actively performed after the patient's tenderness on pressure was reduced. Upon symptom improvement, dietary modifications were attempted in consultation with a nutritionist in conjunction with an exercise prescription that focused on aerobic exercise. The circumferences of both lower extremities were measured at one-week intervals using the same method beginning immediately after transfer to the Department of Physical Medicine and Rehabilitation. The treatment continued for a month. There was no significant change in total weight over the treatment period, but the reduction in edema resulted in decreased circumference of 2.75 cm and 2.45 cm in the right and left lower extremities, respectively. The circumferences of the lower extremities were reduced by 2.75 cm on average compared to measurements taken prior to treatment (Table 1).
Lipedema is a condition that occurs bilaterally and symmetrically in the lower extremities and arises from the deposition of fat tissue starting at the hips and ending at the ankles, in a pattern that is visually similar to riding breeches.4 A family history of lipedema is noted in many patients, as it is a disease that occurs due to an abnormal distribution of fat because of genetic or hormonal abnormalities. Edema is also observed in the hips and both legs due to abnormal fat distribution, but not in the ankles and feet.1-7 The prevalence of lipedema in women has been reported as 11%. Other characteristics of lipedema include hematomas or petechiae that can easily arise from a minor shock or slight touch due to the increased fragility of the microvessels. In addition, tenderness can develop in response to small stimuli and palpations, and it is possible that the variably-sized nodules formed by the accumulation of subcutaneous fats are palpable.1,6
Lipedema tends to be generally misdiagnosed as lymphedema. In our patient, the edema in both lower extremities was misdiagnosed as lymphedema because of a medical history of hysterectomy. However, unlike the indicators for lymphedema, lymph node dissection was not performed as part of the hysterectomy for uterine myoma, but the presence of bilateral symmetrical edema led us to suspect lipedema. Additionally, drugs are often suspected as the cause of edema of the bilateral extremities; however, in this case, the lower extremity edema differed from drug-induced generalized edema because only bilateral lower extremity edema sparing the ankles and feet was observed. Drug-induced edema could also be excluded because the medical history was unremarkable for drugs such as diuretics or immunosuppressants, which are known to cause edema.1,4
Contrary to lymphedema, a family history of lipedema is common. Lipedema occurs bilaterally and symmetrically, and edema is not distinctively observed in the ankles and feet. Stemmer's sign is absent in lipedema because skin fibrosis is rare, and it can be accompanied by damaged skin microvessels due to accumulation of fat, microhematomas or petechiae due to circulatory disturbance.1-6 Serious pain on palpation is relatively common in lipedema compared to lymphedema, and it is rare to find a medical history of cellulitis.5,7 This patient was diagnosed with lipedema based on characteristics that were consistent with the clinical features of lipedema, including bilateral edema of the lower extremities, negative Stemmer's sign, and tenderness on applied pressure.
The progression of lipedema can be divided into three stages according to skin conditions and the sizes of the fat nodules. In the first, early stage of lipedema, soft skin and small, evenly distributed nodes can be observed in thick subcutaneous tissues. The skin appears orange peel-like in the second stage with larger, unevenly distributed nodes of subcutaneous tissue. In the third stage of lipedema, subcutaneous fat tissue projects outside the skin of the knees or thighs, which hinder mobility.1,3 This patient was diagnosed with second-stage lipedema based on the presence of large fat nodes and orange peel-like skin.
Petechiae of this patient were observed in the pretibial portion of the lower extremities, and lipomas were distinctly observed on ultrasonography. After active complex decongestive therapy, the size of the lipomas decreased slightly, but remained. Lipomas are not generally found in patients with lipedema, but some cases of patients with lipedema accompanied by multicentric lipomas have been reported. The pathogenesis with respect to the accumulation of fat tissue is the same, so it is thought that there is a correlation between the two diseases.5 Presently, histological examinations of the lipomas and micropetechiae were not performed because the patient's clinical symptoms and medical history were significant for the characteristics of lipedema. However, histological methods of diagnosis can be considered for this disease.
The symptoms of peripheral polyneuropathies due to diabetes were not observed in this patient, but the patient reported pain from weak pressure. The cause of this pain was not obvious, but it is thought that sensory nerves from each sympathetic nerve fiber are distributed in fat cells and impairment such inflammation of these autonomous nerves can cause tenderness and pain. This impairment may lead to a misinterpretation of protopathic sensory inputs such as sensations of pressure, temperature, or postures. When this impairment is accompanied by microangiopathies, the degree of pain can be increased. Presently, an improvement in pain was be evident after low-intensity manual lymphatic drainage and remedial massage performed for one week.4 In addition, the circulation of lymph is generally normal in patients with lipedema. However, when the disease is chronically progressed, circulatory disturbance occurs due to the pressure of fat cells on lymph collectors at the superficial layers. Moreover, microangiopathy occurs in the regions of edema, altering microcirculation and leading to increased permeability and protein-rich fluid extravasation, which further increases the amount of lymph. In prolonged courses of lipedema, the lymph vessels are unable to maintain their function, and altered microcirculation leads to impaired lymph transport capacity and the accumulation of lymph fluid. The high protein and fat contents of lymph fluid induce fibrosis with positive Stemmer's sign and subsequent progression to lipolymphedema.3,8
If adequate treatment is not administered even though the disease has progressed to chronic lipolymphedema, it has a similar prognosis and progresses to lymphedema. Thus, lipedema can be seriously damaging to the quality of life due to a reduction in the patients' mobility and aesthetic issues.
Active treatment for lipedema is required because early diagnosis and treatment can determine the patient's long-term prognosis. Therapy for lipedema can be largely divided into conservative treatments to reduce edema and surgical treatments such as liposuction. Conservative treatment can first be performed with complex decongestive therapy, which is usually used for patients with lymphedema. Although the long-term therapeutic effects for patients with lipolymphedema are good, the therapeutic effects for those with simple lipedema can be slow and weak. Complex decongestive therapy cannot affect fat tissue, but can contribute to treatment by reducing interstitial edema. No bandages should be used until the pain subsides because, unlike lymphedema patients, those with lipedema report pain and hypersensitivity in the edema areas when complex decongestive therapy is performed. The use of bandages after the pain disappears is helpful in reducing edema. In our case, manual lymphatic drainage was performed for this patient without bandages for one week because of reported tenderness upon the application of pressure to the legs during early treatment. There was an improvement in tenderness after one week of treatment. After the loss of tenderness, complex decongestive therapy including manual lymphatic drainage and bandaging were performed for a month and a reduction in leg circumference was observed. As in the present case, manual lymphatic drainage is typically performed every day during the edema reduction phase and twice weekly in the subsequent preservation phase. After edema reduction through complex decongestive therapy, compression stockings can be considered. According to several reports, a reduction in the excessive fatty tissue in lipedema is possible if the compression stockings are worn constantly and if compression bandages are applied at night.3,4,6,9 However, continuous treatment is critical because the edema will recur or worsen if complex decongestive therapy is stopped.1
Presently, conservative treatment produced a reduction in pain and edema. However, surgical treatment can be considered for patients with lipedema who do not respond to conservative treatment.1 Liposuction was performed under general anesthesia in the early 1990s, but this was associated with some complications such as excessive bleeding or permanent lymphedema due to damage to the lymphatic system. Now, the damage to important tissues such as nerves or blood vessels can be minimized by performing liposuction with thin (2-4 mm diameter) catheters under local anesthesia with advanced anesthesia and operation technologies. For this reason, liposuction is currently the standard surgical treatment method. Complex decongestive therapy for an early period after the operation is helpful in preventing the recurrence of edema because there is still the possibility of damage to the lymphatic system after the operation.1,3-5,7
Additionally, a better treatment effect for obese patients can be expected if their weight management is successful through proper exercise and diet modifications.1,3 Presently, although loss of weight and body fat was expected with diet modifications and aerobic exercise, these effects were not significant.
According to the differing pathophysiologies of lipedema, which occurs due to the accumulation and impaired distribution of fat tissues, and lymphedema, which occurs due to the accumulation of lymph because of abnormalities in lymph circulation, their progression and prognoses differ. Thus, distinguishing between the two diseases at an early stage is important for both clinicians and patients to understand the prognosis and determine the best treatment approach. It is extremely likely that lipedema can be improved if proper treatment is applied before 35-years-of-age, but delayed management makes the prognosis of lipedema similar to that of lymphedema as the disease progresses to lipolymphedema.3
If lipedema is not treated, complications that are detrimental to mental health and life-threatening can occur. These complications include mental problems such as eating disorders and generalized complications including hypertension, diabetes, and heart failure. Furthermore, patients may develop pseudo-Bartter's syndrome, which is characterized by hyperaldosteronism and hypokalemia due to the excessive use of diuretics, and joint problems in the spine or lower extremities due to excessive body weight.3 This patient had continued daily life without special treatment after the occurrence of lipedema, and serious complications resulting from increased body weight (except for hypertension and diabetes) were not observed. Lipedema is a rare disease that has been scarcely reported in Korea. If it is diagnosed and treated early by taking into account its causes and clinical characteristics, complications can be reduced so that the patient can maintain better health and quality of life.
Lipedema is rare and is diagnosed based on a patient's medical history and physical examinations. To diagnose lipedema accurately, it is essential for it to be clearly distinguished from other diseases that can cause lower extremity edema. Lipedema can be easily confused with lymphedema, which is relatively common, because lipedema is a comparatively rare disease. Knowing the clinical features and differences in medical histories from the patients with lipedema will enable clinicians to achieve a good prognosis through quick diagnosis and treatment.
References
1. Weisseleder H, Schuchhardt C. Lymphedema diagnosis and therapy. 2008. 4th ed. Germany: Viavital;p. 294–323.
2. Child AH, Gordon KD, Sharpe P, Brice G, Ostergaard P, Jeffery S, Mortimer PS. Lipedema: an inherited condition. Am J Med Genet A. 2010; 152A:970–976. PMID: 20358611.

3. Juther JE. Lymphedema management: the comprehensive guide for practitioners. 2005. 1st ed. New York: Thieme;p. 87–89.
4. Földi E, Földi M, Ströβenreuther R, Kubik S. Textbook of lymphology for physicians and lymphedema therapists. 2006. 2nd ed. Munchen: URBAN & FISCHER;p. 396–403.
5. Pascucci A, Lynch PJ. Lipedema with multiple lipomas. Dermatol Online J. 2010; 16:4–9. PMID: 20875325.

6. Szolnoky G, Nagy N, Kovacs RK, Dosa-Racz E, Szabo A, Barsony K, Balogh M, Kemeny L. Complex decongestive physiotherapy decreases capillary fragility in lipedema. Lymphology. 2008; 41:161–166. PMID: 19306662.
7. Rudkin GH, Miller TA. Lipedema: a clinical entity distinct from lymphedema. Plast Reconstr Surg. 1994; 94:841–847. PMID: 7972431.
8. Szolnoky G, Borsos B, Barsony K, Balogh M, Kemeny L. Complete docongestive physiotherapy with and without pneumatic compression for threatment of lipedema: a pilot study. Lymphology. 2008; 41:40–44. PMID: 18581957.
9. Macdonald JM, Sims N, Mayrovitz HN. Lymphedema, lipedema, and the open wound: the role of compression therapy. Surg Clin North Am. 2003; 83:639–658. PMID: 12822730.
Fig. 1
Photograph of both lower limbs of the patient. Swelling is seen in both lower limbs except for the feet.

Fig. 2
Photograph of the patient's right lateral thigh. Multiple micropetechiae are seen on the right lateral thigh and calf.
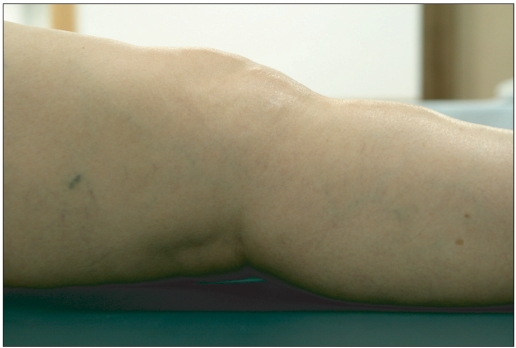
Fig. 3
Results of Technetium-99m human serum albumin lymphoscintigraphy. (A) Lower extremity Technetium-99m human serum albumin lymphoscintigraphy obtained 30 minutes after the injection of radionuclides revealing normal lymphatic drainage. (B) Lower extremity Technetium-99m human serum albumin lymphoscintigraphy obtained three hours after the injection of radionuclides revealing normal lymphatic drainage.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download