Abstract
Objective
To evaluate quiet standing balance of patients with Wallenberg syndrome before and after rehabilitation.
Method
Six patients with Wallenberg syndrome were enrolled within one month after being affected by an infarct of the lateral medulla. Quiet standing balance was assessed using posturography with eyes open and closed. The assessment was repeated after the patients had undergone rehabilitation treatment for three to nine months, and the results of the two assessments were compared.
Results
The quiet standing balance evaluation was performed by measurement of center of pressure (CoP) movement. In the initial test, the mean scores of mediolateral and anteroposterior speed, velocity movement, mediolateral and anteroposterior extent of CoP were all high, indicating impairments of quiet standing balance in the patients. After rehabilitation treatment, the anteroposterior speed and extent, the mediolateral speed and extent, and velocity moment of CoP showed statistically significant reductions in the eyes open condition (p<0.05), and the anteroposterior speed and extent and velocity moment of CoP had decreased in the eyes closed condition (p<0.05). Mediolateral speed and extent of CoP in the eyes closed condition had also decreased, but the reduction was not statistically significant.
Conclusion
This study demonstrated improvements of quiet standing balance, especially anteroposterior balance, in patients with Wallenberg syndrome following rehabilitation. We suggest that balance training is important in the rehabilitation of Wallenberg syndrome and that, as an objective measure of balance status, posturography is useful in the assessment of quiet standing balance.
Go to : 
Wallenberg syndrome, also known as lateral medullary syndrome, is a disease produced by a lateral medullary infarction, which can arise as the result of a stenosis or occlusion of the vertebral artery or the posterior inferior cerebellar artery. The clinical features of this syndrome correspond to the anatomic structures involved and are vertigo, nystagmus, impairment of contralateral pain and temperature, ipsilateral impaired sensation of the face, dysphagia, dysphonia, ataxia, nausea, and vomiting.1,2 Ataxia and balance impairments may affect the gait pattern and daily activities of patients with this syndrome, resulting in a low quality of life and a high risk of falls. Ataxia presents in almost patients with Wallenberg syndrome, and it persists for years even after recovery from the other symptoms.2 Weakness of limbs is rare, so balance impairment is the most important factor for independent gait and daily activities. Improvement of balance is therefore the target goal in the rehabilitation training of patients with this syndrome. The training program consists of sitting balance training, standing balance training, gait training, biofeedback training using a mirror, and balance training with a balance board.3
There are many tools for the evaluation of standing balance, and posturography has recently been widely used. Posturography measures the postural sway of the body in a standing posture by the use of a force platform, which continuously records changes in the center of gravity and is useful as a objective test of standing balance.4 The posturography system consists of a triangular force platform, a computer, and Bluetooth wireless technology which links the platform to the computer. The system measures the postural sway of a subject by sensing the vertical force on platform and analyzing the track of movements in the center of pressure (CoP) while the subject maintains a quiet standing position on the platform.
Several Korean studies have reported the use of posturography to compare the balance control of younger and older adults5,6 and to assess the balance of stroke patients and those with Parkinson's disease, cerebral palsy and low back pain.7-10 However, the study was limited that evaluate the balance control of patients with Wallenberg syndrome, a disease characterized by an ataxia and balance impairment.
In this study, we objectively assessed the quiet standing balance of patients with Wallenberg syndrome by posturography, and than investigated the improvement of balance control of the patients after rehabilitation treatment.
Go to : 
The patient group of subjects was recruited from patients with Wallenberg syndrome, who transferred to our rehabilitation center during the period September, 2009 to April, 2010 within one month after the lateral medullary infarction occurred. They all needed the comprehensive rehabilitation in view of their lack of independent gait and difficulties in performing activities of daily living, mainly because of ataxia and balance impairment. We excluded the subjects, who were unable to stand independently due to vertigo or severe balance impairment, because their quiet standing balance could not be assessed. We also excluded the patients, who could not undergo rehabilitation treatment because of an orthopedic disease or a severe medical problem, such as cardiopulmonary disease. Eight patients with Wallenberg syndrome were recruited for this study, but one was subsequently excluded due to severe vertigo, and another patient was lost to follow up after rehabilitation treatment, leaving only six patients for inclusion in the final analysis.
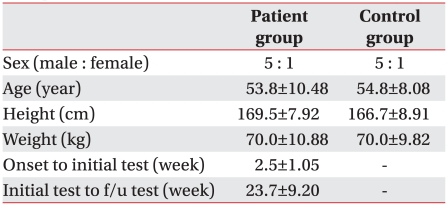
The control group subjects consisted of normal adults who had no history of neurologic disease or balance impairment, and who were able to walk and independently perform daily activities. They were no significant differences in sex, age, height or weight between the patient and control groups. The patient and control groups both consisted of five males and one female, and their average ages were 53.8±10.48 and 54.8±8.08 years, respectively (Table 1).
This study was approved by the Institutional Review Board (IRB) of medical research center at our hospital.
Quiet standing balance was evaluated using posturography Good Balance Evaluator® (Metitur Ltd., Jyväskylä, Finland), which measured postural swaying. The force plate was a regular triangle shape with a side length of 800 mm and a height of 90 mm. Information about vertical force pressure on the plate was obtained by 3-channel direct current amplification and was then transmitted to a computer via a standard Bluetooth wireless link. The Good Balance software analyzed the transmitted information. Postural sway was measured in a quiet, upright standing position and therefore reflected the body's effort to maintain balance in that position. Increasing sway indicated greater effort and poorer balance.11,12
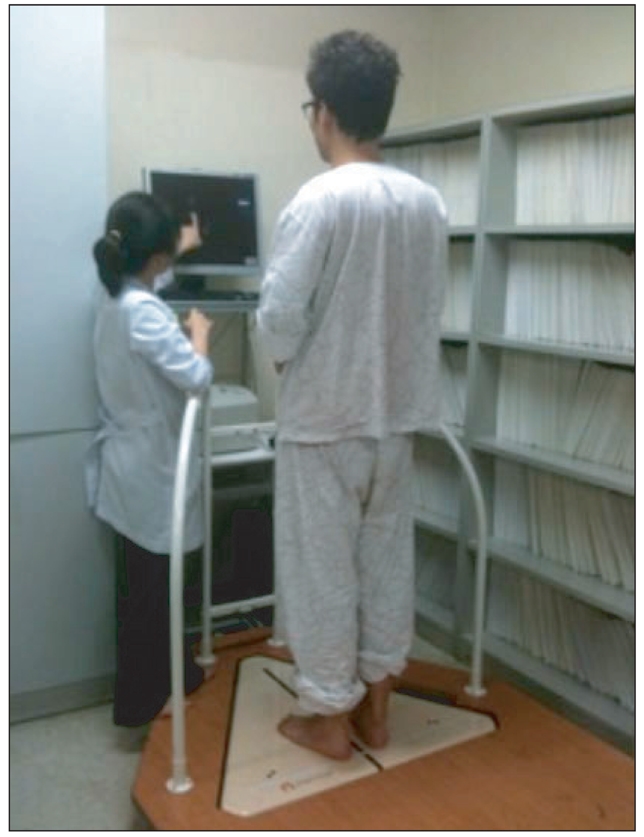
Subjects removed their shoes and stood on the force plate with feet 10 cm apart at the midline of their heels. They stood at attention looking straight ahead in an independent standing position without grasping anything in the surrounding environment or leaning on other person (Fig. 1). After allowing sufficient time for the subjects to stabilize their position, the balance evaluation was started with the subjects attempting to balance themselves without swaying for 30 seconds. The test environment was kept quiet and relaxed in order not to distract the subjects during the procedure. Each subject was assessed twice, once with eyes open and once with eyes closed. The quiet standing balance evaluation was performed on one occasion for the control group and on two occasions for the patient group, before (initial) and after (follow-up) rehabilitation.
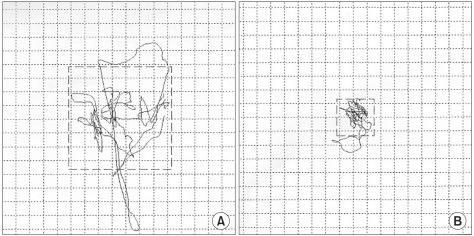
We analyzed the movements of the body's CoP (Fig. 2) during the 30 seconds when the subject stood on the platform and expressed balance in terms of five indices. Mediolateral speed (ML-S, mm/s) and anteroposterior speed (AP-S, mm/s) were average speeds of each mediolateral and anteroposterior pathway of the CoP. Higher ML-S and AP-S meant faster swaying of body, indicating poorer balance. Mediolateral extent (ML-E, mm) and anteroposterior extent (AP-E, mm) were the total extents of the line in each mediolateral and anteroposterior pathway of the CoP. Higher ML-E and AP-E meant larger swaying of body and also indicated poorer balance. Velocity moment (VM, mm2/s) was a moment of speed from the CoP pathway. A higher VM meant more body sway and was another indication of poorer balance.
The patient group of subjects with Wallenberg syndrome was admitted to hospital and underwent rehabilitation treatment. The rehabilitation treatment was conventional balance rehabilitation adapted to each individual's balance problems and consisted of standing balance training, gait training, and one leg standing training. Six patients underwent rehabilitation treatment at the hospital for 2-10 weeks (average time 5.2±3.37 weeks), five days per week, and two hours in a day. After discharge, they underwent a home balance exercise program and were followed up for balance evaluation at the outpatient clinic. The average time between the initial and follow-up tests was 23.7±9.20 weeks.
SPSS version 15.0 was used for all analyses. Differences in balance indices between the Wallenberg patient group and the control group were analyzed using the Mann-Whitney U test. The balance indices of the patient group before and after rehabilitation were compared using the Wilcoxon sign-rank test. Statistical significance was assumed at p<0.05.
Go to : 
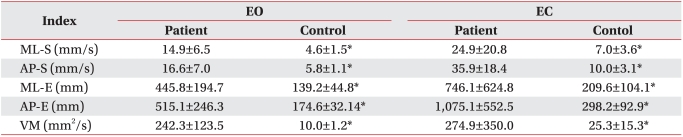
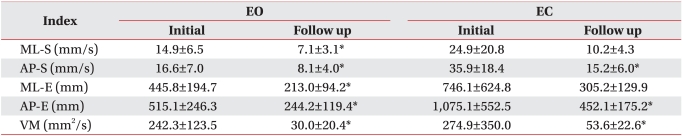
There was no significant difference between patient and control groups in general characteristics such as age, sex, height, and weight. The movements of CoP measured and analyzed by posturography showed significant differences between the patient group and the control group on all five indices of balance (ML-S, AP-S, ML-E, AP-E, VM) under both the eyes open and closed conditions (p<0.05 in both cases) (Table 2).
In the eyes open condition, the patients showed significant (p<0.05) reductions (i.e balance improvements) on all five indices of balance control.
In the eyes closed condition, significant (p<0.05) improvements occurred in three of the five balance indices (AP-S, AP-E, and VM). Although scores on both the remaining two indices (ML-S and ML-E) decreased, the changes were not significant (Table 3).
When the indices of the patient group after rehabilitation were compared with those of the control group, the indices of patient group after rehabilitation were slightly higher, but no significant differences were found except for VM in the eyes closed condition. So we found that balance of patient with Wallenberg syndrome was on the way of improving after rehabilitation.
Go to : 
In this study, we evaluated the quiet standing balance of patients with Wallenberg syndrome by posturography and investigated improvements in balance control by comparing the outcome of posturography assessments before and after a rehabilitation treatment involving balance training. Our results showed that the quiet standing balance of patients with this syndrome was significantly poorer on all of balance indexes than in normal people with similar physical characteristics. This finding is consistent with the previous literature on balance impairment in Wallenberg syndrome.
After the patients underwent a comprehensive rehabilitation program individualized to their state of balance control, quiet standing balance improved in most balance indices. The specific analysis of movement of CoP showed significant improvements of both mediolateral and anteroposterior sway in an eyes open condition. However, under the eyes closed condition, the significant improvements occurred in anteroposterior sway, but not in mediolateral sway. In terms of scores, it showed improvement in all of the balance indices on both eyes open and eyes closed conditions.
Truncal lateropulsion in patients with Wallenberg syndrome is defined as an abnormal tilt to ipsilateral side of the lesion following acute infarction.13 This phenomenon can explain why, in the eyes closed state when visual compensation cannot occur, anteroposterior sway was significantly improved while the mediolateral sway was relatively less improved after rehabilitation training. A mediolateral sway of CoP is the most important predictive indicator for falls. Several previous studies have demonstrated that the more the mediolateral sway, the higher is the risk of falls.14,15 Patients with Wallenberg syndrome had a higher risk of falls towards the ipsilateral side of their lesion, and the degree of correction of standing balance by rehabilitation training was less for mediolateral sway. For this reason, rehabilitation programs of balance training should focus on improving balance control on the side of the brain lesion.
Many clinical assessment tools such as the one leg stance test, the time up and go test, and the functional reach test have been reported for evaluating balance control, but these tests have been limited as objective measures and difficult to use in assessing the diversity of balance control.16,17 To compensate for these limitations and provide a quantitative evaluation of balance control, attempts have been made to use balance tests based on studies of kinematics, kinetics, and dynamic electromyography.18,19 To estimate the balance control of the body exactly, a kinematic analysis of the movements of the body's center of mass is necessary, but it is so hard to measure the center of mass.20 The center of pressure (CoP) reflects the center of mass of the body and is easier to measure. A kinetic analysis of CoP measured by a force platform is therefore widely used.4,7 The Good Balance Evaluator was the posturography apparatus used in the present study, and this analyzes the movements of CoP, showing the digitized speed and extent of its movements in both mediolateral and anteroposterior directions. We suggest that posturography is useful in the balance testing of patients with balance impairments, such as those occurring in Wallenberg syndrome, and that with posturography we can monitor subtle improvements in balance objectively.
Rehabilitation for balance impairment starts with a physical assessment of lower extremity sensation, balance control, gait, and endurance. A specific program is developed and targeted toward the patient's main complaints and functional deficits. Dynamic balance and gait training, and visual feedback training are part of this program, which also includes the application of behavior modification techniques to decrease fear and the teaching of safety recommendations regarding movement and gait.21
A patient with Wallenberg syndrome has truncal lateropulsion tilting to the ipsilateral side of the brain lesion and mobility impairment due to gait ataxia. Rehabilitation involves the correction of these symptoms. An effective treatment guide for these problems has not been well investigated, but studies using treadmill ambulation with partial body-weight support show promise in managing balance and the "pusher's syndrome". Dysphagia and dysphonia are frequently present, and an early assessment of swallowing with appropriate diet modification can prevent aspiration pneumonia. Vertigo can be difficult to treat and generally responds poorly to medication. Therapeutic options for vertigo include postural control and visual-vestibular interaction exercises.22
This study has several limitations. Firstly, the patient group was too small, so it is hard to apply the findings of the study to all Wallenberg syndrome patients. Secondly, the length of time from initial test to follow up test varied (11-39 weeks), since patients differed in the amount of time needed to recover sufficient balance control for a return to daily life. Lastly, the patient group consisted of individuals with different degrees of Wallenberg syndrome, and symptoms of balance impairment varied from mild to severe. There is a wide spectrum of balance impairments in Wallenberg syndrome patients, from independent gait with mild instability to unstable sitting balance. We were unable to compare the degree of balance improvement among patients with different balance impairments. Further research based on a larger patient group with this syndrome is necessary.
Go to : 
We evaluated the use of an objective balance control measurement procedure involving posturography in patients with Wallenberg syndrome, who had an impairment of quiet standing balance. Using posturography, improvements in quiet standing balance were observed after rehabilitation treatment. On testing without visual compensation, these improvements were more significant in anteroposterior sway than in mediolateral sway. In conclusion, an initial balance control assessment by posturography is recommended for patients with Wallenberg syndrome. And an early balance rehabilitation program based on their posturography results enables them to improve their quality of life by balance training.
Go to : 
References
1. Delisa JA, Gans BM, Walsh NE. Physical medicine & rehabilitation principles and practice. 2005. 4th ed. Philadelphia: Lippincott Williams and Wilkins;p. 1660.
2. Lee SS, Roh JK, Lee SB, Myung HJ. A clinical study of 21 patients with lateral medullary syndrome. J Korean Neurol Assoc. 1989; 7:42–51.
3. Lee KG, Chun MH, Kim BR, Kang SH. The effects of biofeedback balance training using interactive balance system in acute stroke patients. J Korean Acad Rehabil Med. 2009; 33:41–47.
4. Kim HD, Kweon DC, Park IS, Im JJ, Nam SH, Park SJ. Quantitative measurement of postural sway during upright posture. J Korean Acad Rehabil Med. 1995; 19:495–499.
5. Kim CR, Chun MH, Lee GA. Assessments of balance control using Tetra-ataxiametric posturography. J Korean Acad Rehabil Med. 2009; 33:429–435.
6. Lim KB, Na YM, Lee HJ, Joo SJ. Comparison of postural control measures between older and younger adults using balance master system. J Korean Acad Rehabil Med. 2003; 27:418–423.
7. Rha DW, Park CI, Chung HI, Kim MJ, Kim HB, Park ES. Comparison of postural control mechanisms during quiet standing between healthy children and children with spastic diplegic cerebral palsy. J Korean Acad Rehabil Med. 2006; 30:468–474.
8. Lim KB, Lee HJ, Joo SJ, Lim SS. Postural control measures of patients with lower back pain using balance master system. J Korean Acad Rehabil Med. 2007; 31:30–36.
9. Kim BR, Choi KH, Chun MH, Lee MC, Chung SJ, Jang KW. Evaluation of balance control in patients with idiopathic Parkinson's disease using Tetraataxiametric posturography. J Korean Acad Rehabil Med. 2009; 33:538–546.
10. Kim HS, Lee KW, Sung DH, Hwang JH, Kim TU. Posturographic characteristics of lesion site in stroke patients. J Korean Acad Rehabil Med. 2000; 24:363–369.
11. Kim SH, Seok H, Lee H, Lee HJ, Suh JW. The effects of transcutaneous electrical nerve stimulation for standing balance in patients with hemiplegia. J Korean Acad Rehabil Med. 2009; 33:159–164.
12. Thapa PB, Gideon P, Brockman KG, Fought RL, Ray WA. Clincal and biomechanical measures of balance as fall predictors in ambulatory nursing home residents. J Gerontol A Biol Sci Med Sci. 1996; 51:M239–M246. PMID: 8808996.
13. Lee H. Central nervous system disorders presenting as vertigo. J Korean Bal Soc. 2004; 3:95–101.
14. Piirtola M, Era P. Force platform measurements as predictors of falls among older people-a review. Gerontology. 2006; 52:1–16. PMID: 16439819.
15. Pajala S, Era P, Markku K, Jaakko K, Timo T, Taina R. Force platform balance measures as predictors of indoor and outdoor falls in community-dwelling woman aged 63-76 years. J Gerontol A Biol Sci Med Sci. 2008; 63:171–178. PMID: 18314453.
16. Berg K, Williams JI. The balance scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995; 27:27–36. PMID: 7792547.
17. Yelnik A, Bonan I. Clinical tools for assessing balance disorder. Neurophysiol Clin. 2008; 38:439–445. PMID: 19026963.
18. Gage WH, Winter DA. Kinematic and kinetic validity of the inverted pendulum model in quiet standing. Gait Posture. 2004; 19:124–132. PMID: 15013500.

19. Lehmann JF, Boswell S, Price R, Burleigh A, deLateur BJ, Jaffe KM, Hertling D. Quantitative evaluation of sway as an indicator of functional balance in post-traumatic brain injury. Arch Phys Med Rehabil. 1990; 71:955–962. PMID: 2241541.
20. Winter DA, Patla AE. Motor mechanisms of balance during quiet standing. J Electromyogr Kinesiol. 2003; 13:49–56. PMID: 12488086.

21. Badke MB, Shea TA, Miedaner JA, Grove CR. Outcomes after rehabilitation for adults with balance dysfunction. Arch Phys Med Rehabil. 2004; 85:227–233. PMID: 14966706.

22. Kirsteins AE, Black-Schaffer RM, Harvey RL. Stroke rehabilitation. 3. Rehabilitation management. Arch Phys Med Rehabil. 1999; 80:S17–S20. PMID: 10326899.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download