Abstract
Objective
To investigate the usefulness of bioimpedance measurement for predicting the treatment outcome in breast cancer related lymphedema (BCRL) patients.
Method
Unilateral BCRL patients who received complex decongestive therapy (CDT) for 2 weeks (5 days per week) were enrolled in this study. We measured the ratio of extracellular fluid (ECF) volume by using bioelectrical impedance spectroscopy (BIS), and single frequency bioimpedance analysis (SFBIA) at a 5 kHz frequency before treatment. Arm circumferences were measured at 10 cm above and below the elbow before and after treatment. We also investigated whether there is correlation between ECF ratio and SFBIA ratio with the change of arm circumference after CDT.
Results
A total of 73 patients were enrolled in this study. The higher ECF ratio was significantly correlated with higher reduction of arm circumference at both above and below the elbow after treatment, but the higher SFBIA ratio was correlated only with the higher reduction of arm circumference below the elbow.
Lymphedema is a chronic disease of the lymphatic system and is characterized by interstitial accumulation of protein, fluid, and subsequent inflammation and fibrosis.1 Primary lymphedema is a rare condition in the general population and occurs secondary to congenital anatomic abnormalities of the lymphatic system, such as lymphatic dysplasia or lymphatic valve dysfunction. Secondary lymphedema is a relatively common condition after treatment of malignancy, especially in breast cancer patients who were treated with axillary lymph nodes dissection and/or radiation therapy on axillary lymph nodes. Secondary lymphedema can cause pain, swelling, limited joint range of motion, and infections such as cellulitis on an affected region.2 Reports concerning the incidence of secondary lymphedema after breast cancer treatment range from 2% to 83%, but the incidence is generally accepted as being -30% in patients treated with axillary surgery and radiotherapy. The incidence is higher in patients with axillary lymph node dissection than in those with sentinel lymph node biopsy, and it is known to occur within 1-2 years after treatment of breast cancer.3-7
The International Society of Lymphology classified lymphedema on a scale of 0 to 3 using the following parameters: Stage 0 refers to a latent or subclinical condition where swelling is not evident despite impaired lymphatic transformation. Stage I is a condition during which protein rich fluid accumulates and the edema subsides with limb elevation. In stage II, tissue fibrosis develops and limb elevation alone rarely reduces tissue edema. Finally, tissue edema and fibrosis are aggravated and trophic skin changes are developed in stage III.1 Because prognosis is worse and more complications occur as disease progresses, early treatment and maintenance are important.3,4,8-10
The severity of lymphedema can be evaluated by measuring limb circumference, volume, tissue tonometry, or water displacement method. Although these methods are simple and convenient, they cannot describe the tissue composition of affected limbs. On the other hand, Bioimpedance measurement is a recently developed method and it attempts to calculate the amount of body fluid by measuring impedance to electrical current that passes through a body segment. This method can be used on limbs with lymphedema; to determine whether the affected limb consists mainly of fluid or other components.11 Several researchers studied the usefulness of bioimpedance in patients with lymphedema, but those reports discussed diagnosis or evaluation of severity,2,7,12,13 and there was no report concerning a bioimpedance measurement being used to predict prognosis after treatment of lymphedema. We suggested the prognosis of lymphedema would be different by the tissue composition, and we attempted to predict prognosis of lymphedema by assessing tissue composition by measuring bioimpedance.
Patients who visited the Asan Medical Center Lymphedema Clinic from April, 2010 to October, 2010 were considered for entry into the trial. The following criteria had to be met before a patient was enrolled into the trial: age of ≥18 years, female gender only, history of surgery and/or radiotherapy and/or chemotherapy, diagnosis of lymphedema by lymphoscintigraphy, circumference difference of both arms >2 cm at 10 cm either below or above elbow. Participants were excluded on the following criteria: presence of certain comorbidities (current meta stasis, active infectious condition, such as cellulitis of affected arm), history of trauma, or surgery to the affected arm.
Complex decongestive therapy (CDT) was conducted on patients for 30 minutes a day, for 10 days (5 days per week). CDT was composed of manual lymphatic drainage, compression bandaging, exercises to enhance lymphatic drainage, and patient education. During treatment periods, CDT was performed by same physical therapist for each patient.
Prior to CDT, we evaluated the calculated extracellular fluid (ECF) and single frequency bioimpedance analysis (SFBIA) value at 5 kHz for both upper extremities with Inbody 720® (Biospace, Seoul, South Korea). Circumferences of both arms 10 cm at above and below the elbow were also checked before and after 2 weeks of the CDT period.
The ECF ratios of the unaffected to affected side and affected to unaffected side ratio of SFBIA value at 5 kHz were calculated and we investigated whether there was a correlation between these values and arm circumference changes after 2 weeks of CDT. After evaluation of bioimpedance values and arm circumferences changes, we investigated whether these bioimpedance values can predict the extent of improvement.
All statistical analyses were performed using SPSS, version 18.0. Data evaluated in our study did not show a normal distribution, and we performed a Spearman's correlation coefficient to investigate the correlation of bioimpedance values and differences between both arm circumferences, and arm circumference changes after treatment. A partial correlation coefficient was also calculated to adjust for age, body mass index (BMI), disease duration, because these factors can affect the result of this study. Statistical significance was defined as a p-value<0.05.
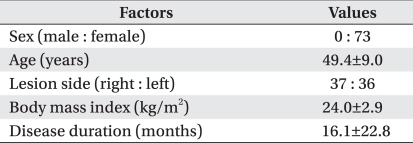
A total of 73 BCRL patients were enrolled in our study. Their mean age was 49.4±9.0 years and mean disease duration was 16.1±22.8 months (Table 1).
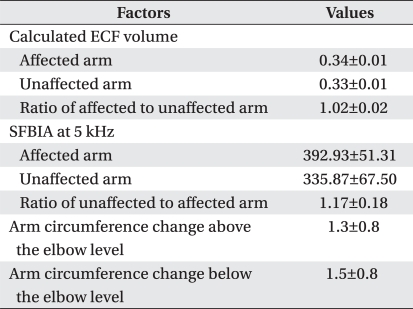
Calculated ECF, SFBIA values at 5 kHz, and their ratios before treatment of lymphedema, and arm circumferences changes after CDT are presented in Table 2. Before CDT, higher calculated ECF and SFBIA ratios were significantly correlated with higher differences of arm circumferences between both sides (Fig. 1).
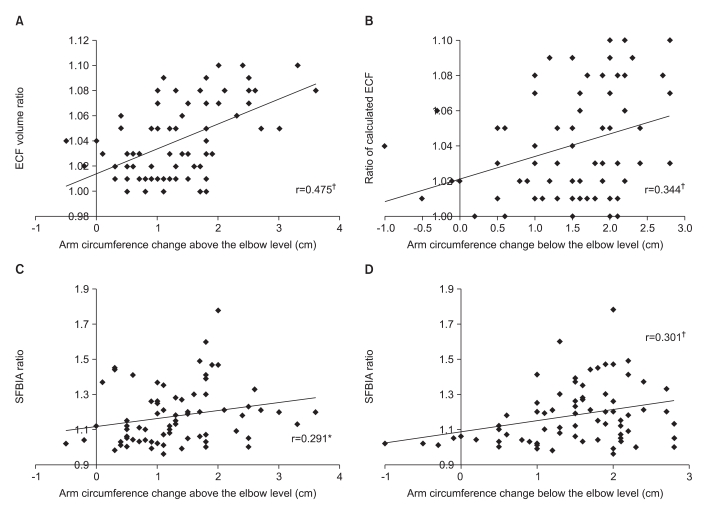
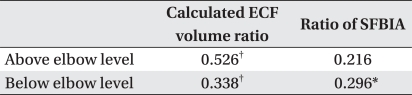
Because calculated ECF ratios were higher, arm circumference changes at 10 cm above and below the elbow were higher (Fig. 2-A, B), and the same results were shown after adjustment for age, BMI, and disease duration (Table 3). Higher SFBIA ratio was significantly correlated with arm circumference changes at 10 cm both above and below elbow (Fig. 2-C, D), but the correlation of SFBIA and arm circumference change at 10 cm above the elbow was not significant after adjustment of age, BMI, and disease duration (Table 3).
The primary object of this study was to investigate whether bioimpedance measurements could help in predicting the treatment outcome in BCRL patients. There was a significant difference between bioimpedance values of an affected arm and those of an unaffected arm in our study, and this result is in agreement with results from previous studies.2,12-14
Protein, fluid, fibrotic and fatty tissues are accumulated in extremities with lymphedema. Composition of an extre mity is influenced by stages and the treatment outcome differs by composition of the extremity. In other words, when there is more fluid than fibrotic or fatty tissue, the treatment outcome will be better. We hypothesized that calculating the extent of fluid in upper extremities with lymphedema would predict the treatment outcome of BCRL patients, and we observed a larger arm circumference reduction in patients with more fluid in an upper extremity.
Bioimpedance analysis measures body response to applied electrical current and calculates the body fluid volume. This technique is relatively new and one of several methods available to differentiate extracellular fluid from total limb volume. There are reports that measurement of bioimpedance is useful for early diagnosis and assessing severity of lymphedema.14,15 Current flow in biological tissue is frequency dependent. At higher frequencies, reactance of cellular membranes decreases, and electrical current can pass through both the extra- and intracellular fluid. However, electrical current at zero frequency can pass only extracellular fluid at zero frequencies, because reactance from cellular membranes acts as insulator to electrical current. Therefore, a bioimpedance measurement at zero frequency is useful in evaluating lymphedema, when fluid accumulates mainly in the extracellular space. Bioimpedance measurements at zero frequency are currently impossible to obtain. There are alternative methods for overcoming limitations of this technique. One method is bioelectrical impedance spectroscopy (BIS), which measures impedance at many frequencies and calculates the impedance at zero frequency. The other method is single frequency bioimpedance analysis (SFBIA), which measures impedance at a single, low frequency that is close to zero.11 In our study, we defined the calculated ECF ratio as a ratio of the affected to the unaffected side, and SFBIA ratio as a ratio of the unaffected to the affected side. A lower value of SFBIA at 5 kHz suggests that there is fluid in extracellular space, and higher ratios of both calculated ECF and SFBIA suggest that there is more ECF.
Warren et al. reported that BIS values of an affected arm in BCRL patients were significantly higher than those of healthy control subjects, thus they suggested BIS as a useful technique in diagnosing lymphedema.2 According to Cornish et al., patients in which BIS values were > 3 standard deviations from those of healthy controls were diagnosed as having lymphedema after 10 months.13 Ward et al. reported that total arm volume measured by perometry was highly correlated with arm fluid volumes predicted by BIS, and the correlation of total arm volume with ECF volume was higher than that of total arm volume with ICF volume.12 As these studies show, BIS is an accurate technique for assessing lymphedema. SFBIA is known to be less accurate than BIS, but the clinical usefulness of SFBIA has been reported by investigators. York et al. reported the high correlation of SFBIA and BIS and they concluded that SFBIA is a simple accurate alternative to BIS for the clinical assessment of unilateral lymphedema.15
Many studies have applied bioimpedance measurements to lymphedema patients, but they concerned early diagnosis and assessing severity of lymphedema. To the best of our knowledge, no prior study has conducted to predict the treatment outcome using bioimpedance measurements, and our study is the first to investigate whether a bioimpedance measurement is useful for predicting treatment outcome. Arm circumference and volume measurements have been frequently used to assess severity of lymphedema, but these methods cannot determine the composition of an affected arm and thus it was difficult to predict treatment outcome with these methods. We attempted to predict treatment outcome by measurement of bioimpedance. In our present study, higher ratios of calculated ECF and SFBIA were significantly correlated with differences of both arm circumferences and changes of affected arm circumference. However, SFBIA ratio was not significantly correlated with arm circumference change at 10 cm above the elbow after adjustment for age, BMI, and disease duration. Although there were significant correlations between ratios of bioimpedance values and clinical data, calculated ECF and SFBIA ratios did not show a strong correlation with differences of arms circumference (Fig. 1), and arm circumference changes (Table 3).
In our study, difference and change of arm circumference were correlated with calculated ECF than SFBIA. And these results are in agreement with results from pre vious study.15 The SFBIA ratio at 5 kHz predicted the arm circumference change at below the elbow level, but was not significantly correlated with arm circumference change above the elbow level. This may be because the severity of lymphedema can be different in regions above and below the elbow, but this technique cannot separately measure fluid volumes below and above the elbow level.
In our present study, we suggest that measurement of bioimpedance can help in predicting treatment outcome by estimating fluid volume of the affected arm in lymphedema patients. However, correlation coefficients of bioimpedance values and clinical data indicate that bioimpedance measure is not very accurate for predicting treatment outcome. This means that while bioimpedance measurements are useful tools for assessing severity and predicting treatment outcome, it is better to interpret the results of bioimpedance measure comparising with evaluation tools, such as arm circumference and volume measure, water displacement method, and lymph scintigraphy. BIS is a more accurate method than SFBIA, but the BIS device requires a large amount of space. On the other hand, the SFBIA device is simple and small, so it can be easily used in clinical situations. Physicians need to understand the advantages and disadvantages of these devices and appropriately apply them to patients.
There are some limitations in our study. First, our sample size was small; however, sample sizes of previous studies on bioimpedance measurement were smaller than that of our study2,7,12,13,15 and more reliable results would be expected if more patients are enrolled. Second, except for the study of Carati et al.7, devices used in other studies were different from that used in our study. Third, our device could not directly measure ECF volume, but could only calculate the ratio of ECF to total arm volume. If we could directly measure ECF volume, more accurate results could be expected. Therefore, further studies with devices that directly measure ECF volume are needed. Finally, our study considered the disease duration, but we did not consider the stage of lymphedema. Because treatment outcome differs with different disease stage, if we analyzed our results relative to disease stage, we could obtain more accurate results.
In the present study, bioimpedance values measured by BIS and SFBIA were significantly correlated with arm circumferences changes, and it appears that BIS is more accurate than SFBIA. Thus, estimating ECF volume with bioimpedance measurement may be a useful modality for assessing severity and predicting treatment outcome in lymphedema patients. Further studies concerning the accuracy and usefulness of bioimpedance measure will be needed.
References
1. Warren AG, Brorson H, Borud LJ, Slavin SA. Lymphedema: a comprehensive review. Ann Plast Surg. 2007; 59:464–472. PMID: 17901744.
2. Warren AG, Janz BA, Slavin SA, Borud LJ. The use of bioimpedance analysis to evaluate lymphedema. Ann Plast Surg. 2007; 58:541–543. PMID: 17452840.

3. Hayes SC, Janda M, Cornish B, Battistutta D, Newman B. Lymphedema after breast cancer: incidence, risk factors, and effect on upper body function. J Clin Oncol. 2008; 26:3536–3542. PMID: 18640935.

4. Sener SF, Winchester DJ, Martz CH, Feldman JL, Cavanaugh JA, Winchester DP, Weigel B, Bonnefoi K, Kirby K, Morehead C. Lymphedema after sentinel lymphadenectomy for breast carcinoma. Cancer. 2001; 92:748–752. PMID: 11550143.

5. Meneses KD, McNees MP. Upper extremity lymphedema after treatment for breast cancer: a review of the literature. Ostomy Wound Manage. 2007; 53:16–29. PMID: 17551172.
6. Erickson VS, Pearson ML, Ganz PA, Adams J, Kahn KL. Arm edema in breast cancer patients. J Natl Cancer Inst. 2001; 93:96–111. PMID: 11208879.

7. Carati CJ, Anderson SN, Gannon BJ, Piller NB. Treatment of postmastectomy lymphedema with low-level laser therapy: a double blind, placebo-controlled trial. Cancer. 2003; 98:1114–1122. PMID: 12973834.
8. Petrek JA, Heelan MC. Incidence of breast carcinoma-related lymphedema. Cancer. 1998; 83:2776–2781. PMID: 9874397.

9. Rietman JS, Dijkstra PU, Geertzen JH, Baas P, de Vries J, Dolsma WV, Groothoff JW, Eisma WH, Hoekstra HJ. Treatment-related upper limb morbidity 1 year after sentinel lymph node biopsy or axillary lymph node dissection for stage I or II breast cancer. Ann Surg Oncol. 2004; 11:1018–1024. PMID: 15525832.

10. Szuba A, Rockson SG. Lymphedema: classification, diagnosis and therapy. Vasc Med. 1998; 3:145–156. PMID: 9796078.

11. Cornish B. Bioimpedance analysis: scientific background. Lymphat Res Biol. 2006; 4:47–50. PMID: 16569208.

12. Ward LC, Czerniec S, Kilbreath SL. Quantitative bioim pedance spectroscopy for the assessment of lymphoedema. Breast Cancer Res Treat. 2009; 117:541–547. PMID: 19082708.
13. Cornish BH, Chapman M, Hirst C, Mirolo B, Bunce IH, Ward LC, Thomas BJ. Early diagnosis of lymphedema using multiple frequency bioimpedance. Lymphology. 2001; 34:2–11. PMID: 11307661.
14. Ward LC. Bioelectrical impedance analysis: proven utility in lymphedema risk assessment and thera peutic monitoring. Lymphat Res Biol. 2006; 4:51–56. PMID: 16569209.
15. York SL, Ward LC, Czerniec S, Lee MJ, Refshauge KM, Kilbreath SL. Single frequency versus bioimpedance spectroscopy for the assessment of lymphedema. Breast Cancer Res Treat. 2009; 117:177–182. PMID: 18563555.

Fig. 1
Relationship of bioimpedance value with differences of bilateral arm circumference above (A, C) and below the elbow (B, D) (*p<0.05, †p<0.01). ECF: Extracellular fluid, SFBIA: single frequency bioimpedance analysis.
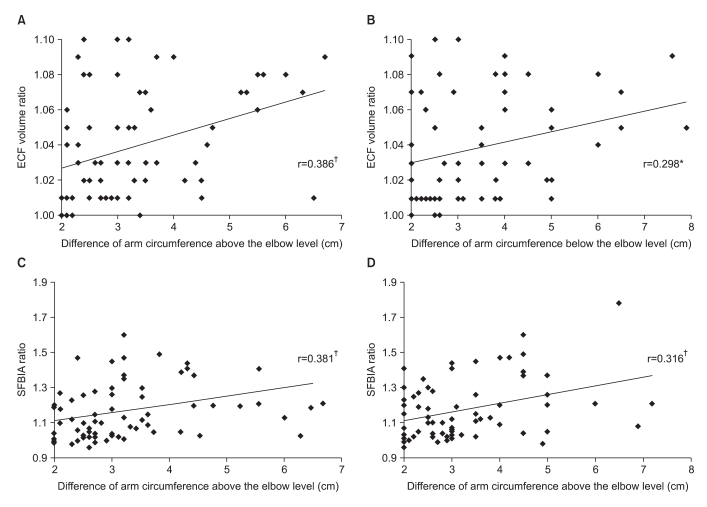
Fig. 2
Correlation of bioimpedance value and change of arm circumferences above (A, C) and below elbow (B, D) (*p<0.05, †p<0.01). ECF: Extracellular fluid, SFBIA: single frequency bioimpedance analysis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download